Community Health Program
Overview
Community health services are an integral part of Victoria’s primary care network. They deliver a diverse range of clinical and non-medical services, including the state-funded Community Health Program (CHP). The CHP is administered by the Department of Health and Human Services (DHHS), and aims to provide disadvantaged Victorians with access to high-quality general counselling, allied health, and nursing services.
In this audit, we examined whether the CHP effectively contributes to good healthcare outcomes for Victoria’s priority populations. We analysed DHHS’s management of the CHP, with a particular focus on its strategic direction, access and demand management, and performance monitoring.
This audit is important because well-coordinated primary care services may improve Victorian’s health and wellbeing, and reduce avoidable hospital admissions.
As a follow-the-dollar audit, we also looked at 10 community health services:
- four integrated health services—Bendigo Health, East Wimmera Health Service, Monash Health and Peninsula Health
- five registered community health services—Bendigo Community Health Service, cohealth, Gippsland Lakes Community Health, Latrobe Community Health Service and North Richmond Community Health
- one multipurpose health service—Orbost Regional Health.
We made seven recommendations to DHHS in this audit.
Transmittal letter
Ordered to be published
VICTORIAN GOVERNMENT PRINTER June 2018
PP No 397, Session 2014–18
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report Community Health Program.
Yours faithfully
Andrew Greaves
Auditor-General
6 June 2018
Acronyms and abbreviations
| CHMDS | Community Health Minimum Dataset |
| CHP | Community Health Program |
| DHHS | Department of Health and Human Services |
| DPAC | Divisional Performance Assurance Compliance |
| FOPMF | Funded organisation performance monitoring framework |
| INI | Initial needs identification |
| PEF | Performance escalation framework |
| PHW Plan | Victorian public health and wellbeing plan 2015-19 |
| VAGO | Victorian Auditor-General's Office |
| VHES | Victorian Healthcare Experience Survey |
Audit overview
Primary care is an integral part of Victoria's health system—it includes services such as general practice, pharmaceutical services, allied health, and community nursing. In Victoria, the state and Commonwealth governments both fund the provision of primary care.
Community health services are essential to Victoria's primary care network. They deliver a range of state- and Commonwealth-funded programs, including the state-funded Community Health Program (CHP). There are 85 community health services located in rural, regional and metropolitan Victoria. These operate under two distinct legal and governance arrangements:
- Fifty-five community health services operate as part of regional or metropolitan Victorian public health services. These 'integrated' community health services are subject to the accountability frameworks of the broader health service.
- Thirty registered community health services operate as companies limited by guarantee. To receive state government funding, they must register as a community health service under the Health Services Act 1988.
The CHP aims to provide effective healthcare services and support to Victoria's priority populations. These populations receive priority access to services because they are socially or economically disadvantaged, experience poorer health outcomes, and have complex care needs or limited access to appropriate healthcare services.
The Department of Health and Human Services (DHHS) administers the CHP through funding paid to community health services. DHHS's central office and divisions—North, South, East and West—are responsible for delivering the CHP. Each division operates several regional offices that are located across the state.
This audit examined whether the CHP effectively contributes to good healthcare outcomes for Victoria's priority populations. We analysed DHHS's management of the CHP, focusing on their strategic direction, access and demand management, and performance monitoring.
Conclusion
The CHP is a valuable tool for DHHS to keep Victoria's priority populations well, out of hospital, and productive in society. However, maximising these benefits requires DHHS to analyse demand and unmet need, and evaluate program outcomes.
DHHS does not regularly monitor whether the CHP's limited service hours are being provided primarily to Victoria's priority populations or what outcomes these services are delivering. Nor does it know where there is demand for the CHP or the extent of this demand across Victoria.
DHHS's funding model and distribution methods are based on historical data as opposed to analysis of changed population demographics. This may affect community health services' ability to deliver timely, effective and appropriate care to Victoria's priority populations. The community health services we audited do not necessarily promote their services due to lack of capacity.
DHHS's limited insights mean it is missing an important opportunity to take a more strategic approach when funding community health services, informed by a broad understanding of health service needs and utilisation across the spectrum of care services.
Recognising this, DHHS is currently progressing a number of projects to improve the CHP. These include considering a new funding model and making improvements to the Community Health Minimum Dataset (CHMDS) and use of its data. It will be necessary for DHHS to carefully monitor the results of this work and use that information to refine the program. Though the CHP's budget is very small in comparison to that for acute care services, there is a clear opportunity for DHHS to realise a significant return on its investment through effective preventative and primary health care services for the most disadvantaged Victorians.
Findings
Strategic management
Long-term health strategies
DHHS has two long-term strategies relevant to the CHP—Health 2040: Advancing health, access and care (Health 2040) and the Victorian public health and wellbeing plan 2015–19 (PHW Plan). DHHS has also released the Statewide design, service and infrastructure plan for Victoria's health system 2017–2037 to operationalise Health 2040.
The CHP's objective to provide effective healthcare services to Victoria's priority populations aligns with DHHS's long-term health strategies for better health, access and care. However, DHHS's ability to measure the CHP's effectiveness or contribution to DHHS's strategic directions is limited because DHHS does not have outcome measures or relevant data.
Evidence base for the CHP
DHHS's Community health integrated program guidelines have strong theoretical underpinnings and emphasise person-centred care. While DHHS has a range of demographic information, it does not incorporate on-the-ground information, such as indices of disadvantage or demographic data, into the CHP's evidence base. This limits DHHS's ability to translate theory into practice and deliver effective healthcare services to the right people in the right place at the right time.
DHHS should strengthen its evidence base by using population health data and information from the CHMDS. DHHS demonstrated this approach when identifying sites for the expansion of its Healthy Mothers, Healthy Babies Program.
Funding for the CHP
DHHS implemented a new funding model in 2007. Since then, DHHS has not reviewed the CHP's funding. As a result, DHHS cannot assure itself that its funding model supports the achievement of the CHP's objectives. DHHS has not reviewed:
- the unit price, to ensure that it reflects the true cost of providing one hour of service delivery
- the total amount of funding for the CHP
- the distribution of the CHP's funding across community health services.
DHHS's executive board has approved a proposal to undertake further research, analysis and sector engagement to inform any future funding reform options.
Access and demand
Timely access to the CHP is important—it ensures that disadvantaged people who cannot afford privately funded primary care receive the treatment that they need. Timely treatment means individuals can have better health, avoid hospital admissions and participate in society.
While DHHS can monitor who accesses the CHP, it does not do this regularly. Therefore, DHHS has limited oversight of whether services are provided to priority populations. DHHS's analysis of current or unmet demand for the CHP is limited and it does not know whether the CHP provides priority populations with effective, timely and sufficient care.
DHHS's key guidance document for managing access to the CHP is Towards a demand management framework for community health services. DHHS has not reviewed this guidance since its publication in 2008.
All the community health services we audited managed client intake in accordance with DHHS's guidance. Community health services commented that they update the tools used to prioritise clients to reflect current research. Community health services do this work in isolation from each other, duplicating effort, and do not receive specific funding for this.
DHHS is currently evaluating future health demand in the northern growth corridor by examining health risk factors, such as smoking and education levels. It has also commenced a project to examine demand in community health services by using past data and future population estimates.
Performance and quality
DHHS's performance management system
While DHHS has some tools to monitor quality, the CHP's current measuring, monitoring and reporting system focuses on outputs and lacks performance measures that assess whether care was timely and effective. As a result, DHHS cannot provide assurance through its current performance management system that the CHP delivers good healthcare outcomes for Victoria's priority populations. DHHS's sole performance measure—the number of service hours delivered—provides little insight into the efficiency, effectiveness or equity of care.
|
Process-based indicators evaluate the implementation of care as opposed to its outcomes. |
In 2014–15, DHHS piloted a set of process-based indicators to evaluate the client's administrative journey from admission to discharge. DHHS stopped collecting this data in 2016–17, following feedback from the sector that the data collection method imposed significant administrative burden on community health services. DHHS is addressing some of its data issues through a wide‑reaching improvement project and, after consulting with the sector, has begun to embed some of the process-based indicators into the CHMDS.
DHHS's management of community health services
DHHS uses a standardised performance monitoring framework to govern registered community health services. However, DHHS's divisions apply certain elements of the framework inconsistently, which leads to variances in performance management across agencies.
Adding further variation to performance management in the sector, DHHS lacks a specific performance monitoring framework for integrated community health services. This limits DHHS's oversight of integrated community health services, which may, in turn, limit its ability to identify and address performance issues in a timely and effective manner.
Program quality
As the CHP's performance measures focus solely on quantity, DHHS has limited oversight of the program's effectiveness and impact beyond community health services' accreditation cycles. DHHS is currently extending its knowledge of the CHP's quality through the collection of process-based indicators and the Victorian Healthcare Experience Survey (VHES), which assesses client satisfaction. While both tools provide insight regarding the provision of care and represent a step in the right direction, DHHS must ensure that the results of the survey are shared and used in a productive manner to yield value for the sector.
Recommendations
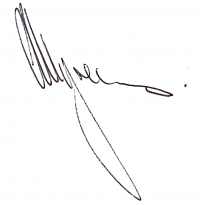
We recommend that the Department of Health and Human Services:
1. link its key strategic documents—such as Health 2040: Advancing health, access and care and the Victorian public health and wellbeing plan 2015−19—to the Community Health Program (see Section 2.2)
2. ensure it collects purposeful data to monitor that CHP funded services are provided to the identified priority populations (see Section 3.4)
3. review its CHP unit pricing to ensure that it meets the cost of providing services to Victoria's priority populations (see Section 2.4)
4. develop a more sophisticated funding model by identifying and understanding the different service needs, demand and priorities for community health service locations across Victoria, to inform the quantum and distribution of funding (see Section 2.4)
5. in conjunction with community health services, regularly review and revise the demand management framework and clinical priority tools to ensure that they reflect optimal practice (see Section 3.3)
6. have internal and publicly available quality performance measures that assess program equity and client satisfaction, while working towards outcome measures for the Community Health Program (see Section 4.3)
7. provide divisional offices with guidance that standardises their monitoring of community health services (see Section 4.5).
Responses to recommendations
We have consulted with DHHS, Bendigo Health, East Wimmera Health Service, Monash Health, Peninsula Health, Bendigo Community Health Service, cohealth, Gippsland Lakes Community Health, Latrobe Community Health Service, North Richmond Community Health and Orbost Regional Health. We considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report to those agencies and asked for their submissions or comments. We also provided a copy of the report to the Department of Premier and Cabinet.
The following is a summary of those responses. The full responses are included in Appendix A.
DHHS acknowledged that the audit provides an opportunity to build on existing initiatives supporting community health services, especially for disadvantaged Victorians. DHHS accepted all our recommendations and provided an action plan detailing how these recommendations will be implemented, including its intention to form a Community Health Taskforce to consult with the sector and assist DHHS to implement the recommendations.
cohealth responded and was supportive of our recommendations, noting that their implementation will require resourcing for both DHHS and the community health sector.
1 Audit context
Primary care is a fundamental pillar of Victoria's health system—it includes services such as general practice, pharmaceutical services, allied health and community nursing. Well-coordinated primary care should improve the health and wellbeing of Victorian communities, enable the effective treatment of people with chronic diseases, and enhance outcomes for disadvantaged Victorians.
Generally, primary care is a person's first point of contact with the broader health system and it becomes the central point for ongoing, coordinated treatment. Acute care, in contrast, involves specialised, short-term intervention to address severe illness or injury. Acute care generally occurs in a hospital setting and includes admitted and non-admitted services. A good primary care system should alleviate pressure on the acute sector through the prevention and effective management of chronic diseases, reducing the number of avoidable hospital admissions per year.
In Victoria, the state and Commonwealth governments fund the provision of primary care. The Commonwealth Government provides the majority of funding through entitlement programs such as the Medicare Benefits Schedule and the Pharmaceutical Benefits Scheme. Private allied health practitioners also operate across Victoria and provide an additional option for people seeking healthcare.
1.1 Community health services
Community health services are an integral part of Victoria's primary care network. They aim to reduce social inequity through effective consumer engagement and have strong connections to their local areas.
Community health services occupy a unique role in the Victorian landscape as a state-funded provider of primary care services. They work alongside other Commonwealth and privately-funded programs to deliver a diverse range of clinical and non-medical services. They prioritise access for people who generally have the poorest healthcare outcomes and are the most disadvantaged.
Community health services, however, are not the sole provider of primary care to disadvantaged people. These groups also access other service types, such as bulk-billing general practitioners.
Importantly, community health services are 'platform providers' of both health and social services—they can deliver up to 30 different programs through 60 different funding streams. Community health services thus facilitate a broad range of both state and Commonwealth initiatives that holistically address their clients' needs.
There are currently 85 community health services across Victoria—see Figures 1A and 1B. These differ in size and the range of programs they offer.
Most of the state's community health services formed in the 1970s to deliver the social model of health. The social model of health recognises that Victorians have unequal access to education, healthcare, cultural activities and employment. It aims to enhance outcomes for disadvantaged Victorians by providing equitable and affordable healthcare. Fundamentally, the social model acknowledges that a person's environment influences his or her health in addition to disease and injury.
Figure 1A
Community health services across Victoria
Note: LGAs = local government areas.
Source: DHHS.
Figure 1B
Community health services across metropolitan Melbourne
Note: LGAs = local government areas.
Source: DHHS.
There is great diversity across the community health sector, not just in the services they provide, but also in their operating models and their strategic priorities. While some organisations are small local services, primarily focused on the delivery of health services to disadvantaged groups within their local areas, others have grown or amalgamated to be very large organisations and operate from multiple 'satellite sites' across Victoria.
In Victoria, community health services operate under two distinct legal and governance arrangements and have different accountability mechanisms under legislation:
- Fifty-five community health services are part of rural or metropolitan public health services. They are subject to the regulatory provisions set out in Division 9B of the Health Services Act 1988.
- Thirty registered community health services are companies limited by guarantee. Registered community health services are subject to the regulatory provisions set out in Division 6 of the Health Services Act 1988.
1.2 The Community Health Program
The CHP aims to deliver effective primary care services to Victoria's priority populations. According to the CHP's guidelines, 'priority populations' refers to people who are socially or economically disadvantaged, experience poorer overall health outcomes, and have complex care needs or limited access to appropriate healthcare. These priority populations include:
- Aboriginal and Torres Strait Islander people
- people with an intellectual disability
- children in out-of-home care
- people with a mental illness
- refugees and asylum seekers
- people experiencing or at risk of homelessness.
DHHS administers the CHP through a flexible funding source paid to community health services. Community health services deliver the CHP in addition to a broader suite of state- and Commonwealth-funded initiatives.
Figure 1C shows the range of state-funded primary and community health programs that community health services can deliver.
DHHS funds some community health services to deliver particular programs. For example, the Healthy Mothers, Healthy Babies Program—a specialised initiative—targets vulnerable, at-risk pregnant women and is only available in 20 local government areas. In contrast, the CHP is universal to all community health services.
Figure 1C
State-funded primary and community health programs
Note: MDC=multidisciplinary centre.
Source: VAGO based on DHHS documentation.
As shown in Figure 1D, the CHP funds community health services to deliver a range of activities, such as general counselling, allied health and nursing services. Community health services—in conjunction with DHHS—determine the mix of activities that they deliver. This flexible funding source enables community health services to customise the CHP to meet the needs of their local communities.
Figure 1D
Activities funded by the CHP
Source: VAGO based on DHHS documentation.
Client profile
In 2016–17, the CHP provided 705 318 hours of allied health, generalist counselling and nursing services to 181 977 individual registered clients. Of these:
- 57.7 per cent were female
- 1.9 per cent identified as either Aboriginal or Torres Strait Islander
- 2.9 per cent identified as a refugee
- 17.6 per cent had a chronic and complex condition
- 46 per cent had a concession card.
1.3 Department of Health and Human Services
DHHS's central office has statewide responsibility for managing the CHP. This includes collecting and monitoring performance information, leading service improvement initiatives, and developing and implementing key policy and strategic directions.
DHHS's regional offices monitor the CHP's delivery by community health services and escalate performance issues to the central office when required. The central office provides key support through the provision of data and performance reports.
The Health Services Act 1988 establishes Victoria's public health services, public hospitals and multipurpose services as independent legal entities. Integrated community health services are part of rural or metropolitan health services. They are covered by the regulatory provisions set out in Division 9B of the Health Services Act 1988. A key accountability mechanism is the Statement of Priorities which is negotiated annually by DHHS with each Victorian public health service and public hospital.
Registered community health services are governed by the regulatory provisions set out in Division 6 of the Health Services Act 1988. A key accountability mechanism is the service agreement established between DHHS and the funded agency.
Overall the legislative and accountability frameworks provide both integrated and registered community health services with the flexibility to make decisions about services they deliver with state government funding, based on local needs.
Both types of community health services are subject to established performance monitoring processes, and DHHS may intervene if there are concerns about the delivery of funded programs and services.
1.4 Service delivery
DHHS funds community health services to deliver a defined number of hours of primary care. While community health services must deliver care within these thresholds, they have the flexibility to develop innovative approaches that reflect the needs of their local areas.
The CHP promotes a person-centred approach that assists clients to manage their own care, improve their understanding of the health system, and make informed decisions. It encourages community health services to undertake a team-based approach and deliver evidence-based services that 'wrap around' the individual—that is, multiple practitioners should collaborate to create a care plan that addresses the client's needs. The CHP also promotes early intervention, as this reduces the risk of further deterioration and produces better outcomes for clients.
1.5 Program funding
In 2017–18, the 85 community health services will receive approximately $105 million in funding to deliver allied health and nursing services under the CHP. This equates to around one million hours of service delivery. When compared to the overall Victorian health budget, the CHP makes up less than 1 per cent of Victoria's expenditure.
The CHP's funding is based on units and measured in service hours. In 2017–18, community health services will receive $104.93 for each hour of allied health practice and $93.62 for each hour of nursing that they deliver. This unit price must cover the community health services' travel expenses, general operating costs, rent, access coordination and the maintenance of facilities.
1.6 Why this audit is important
DHHS funds the CHP to provide effective healthcare and support to Victoria's priority populations. Community health services have the flexibility to develop innovative approaches to service delivery, such as the formation of multidisciplinary teams to support clients through a 'wrap around' model of care.
This audit is important because it is the first audit we have done of the CHP. It is also important because the CHP provides healthcare to priority populations that otherwise may not be able to afford these types of services. Along with other important primary care services—such as general practice—these forms of care can improve clients' health and wellbeing outcomes and reduce avoidable hospital admissions.
1.7 What this audit examined and how
This audit examined whether the CHP effectively contributes to good healthcare outcomes for Victoria's priority populations. We analysed DHHS's management of the CHP, with a particular focus on its strategic direction, access and demand management, and performance monitoring.
As a follow-the-dollar audit, we also included 10 community health services:
- four integrated health services—Bendigo Health, East Wimmera Health Service, Monash Health and Peninsula Health
- five registered community health services—Bendigo Community Health Service, cohealth, Gippsland Lakes Community Health, Latrobe Community Health Service and North Richmond Community Health
- one multipurpose health service—Orbost Regional Health.
We focused on how community health services manage demand and how they implement DHHS's guidelines.
The audit methods included:
- interviews with DHHS and community health service staff
- reviews of strategies, program delivery documents, policies, procedures and waiting lists
- site visits to all 10 community health services
- analysis of the CHMDS.
We conducted our audit in accordance with section 15 of the Audit Act 1994 and ASAE 3500 Performance Engagements. We complied with the independence and other relevant ethical requirements related to assurance engagements. The cost of this audit was $440 000.
1.8 Report structure
The remainder of this report is structured as follows:
- Part 2 examines the strategic management of the CHP
- Part 3 examines access and demand management for the CHP
- Part 4 examines the use of outcomes measures for the CHP.
2 Strategic management
DHHS's strategic management of the CHP is important to ensure the program has the resources required to meet its overarching objective. It is also important that DHHS can measure the contribution the CHP makes to long-term health strategies.
In this part of the report, we evaluate whether the CHP supports DHHS's strategic direction and fulfils its overarching objective of delivering effective healthcare to Victoria's priority populations. We also assessed the CHP's evidence base and examined whether its funding model is sound, regularly reviewed and strategically aligned.
2.1 Conclusion
DHHS's strategic management of the CHP partly supports the achievement of the program's objectives. A strong evidence base supports the CHP's model of care, but DHHS could strengthen this by using population health data and information from the CHMDS to better target effort. While the CHP aligns with DHHS's long‑term health strategies, DHHS is unable to measure the contribution that the CHP makes to those strategies.
While the current funding model supports some flexibility in the delivery of services, the CHP's funding model does not support DHHS to achieve the program's objectives. DHHS does not know whether the unit price, funding for the CHP and the allocation of funding provide effective healthcare to Victoria's priority populations. Further work is required to develop a funding model that aligns with the purpose of the CHP.
2.2 Long-term health strategies
Health 2040: Advancing health, access and care
The Victorian Government released Health 2040 in December 2016 after consultation with the public and the sector. By 2040, it aims for all Victorians to experience:
- better health—building skills and delivering support to be healthy and well
- better access—fair, timely and easier access to care
- better care—world-class healthcare every time.
Statewide design, service and infrastructure plan for Victoria's health system 2017–2037
The Victorian Government released the Statewide design, service and infrastructure plan for Victoria's health system 2017–2037 in December 2017 to support the delivery of Health 2040's vision. It provides a blueprint for health service and infrastructure investment for the next 20 years.
The plan includes five priority areas that will deliver Health 2040's three objectives. The five priority areas are:
- Priority area 1: Building a proactive system that promotes health and anticipates demand
- Priority area 2: Creating a safety and quality-led system
- Priority area 3: Integrating care across the health and social service system
- Priority area 4: Strengthening regional and rural health services
- Priority area 5: Investing in the future—the next generation of healthcare.
Each priority area specifies a number of focuses and actions to implement the plan's five-year goals and 20-year outcomes. Priority areas 1 and 3 relate directly to community health. The relevant actions include:
- integrating prevention and early intervention
- expanding primary care service options
- establishing health and wellbeing hubs.
The plan states that community health is a central part of Victoria's healthcare system. It commits to consolidating the sector's role by including community health in provider alliances, and health and wellbeing hubs. Importantly, it acknowledges that DHHS's current funding and organisational arrangements limit the capacity of such services to maximise integration. This may affect the delivery of services to people with chronic and complex needs.
Overall, Health 2040's vision for better health, access and care clearly aligns with the CHP's objectives to provide timely, affordable and effective healthcare to Victoria's priority populations.
As DHHS launched the plan in December 2017, it is too early to see progress. However, DHHS has formed an internal steering committee to oversee action and has committed to report on progress against the plan every two years.
Victorian public health and wellbeing plan 2015–19
The Public Health and Wellbeing Act 2008 mandates that Victoria must have a public health and wellbeing plan that identifies the state's needs, examines data and establishes key objectives. The current PHW Plan acknowledges the correlation between poor health and other social inequalities, such as limited access to housing, education, employment and public transport. It aims to reduce the avoidable burden of disease and injury so that all Victorians can experience the highest attainable standards of health, wellbeing and social participation. In October 2016, DHHS released an associated document—the Victorian public health and wellbeing outcomes framework (outcomes framework). This outlines DHHS's vision for a disease-free Victoria by progressively improving people's health.
The outcomes framework contains indicators, targets and measures for each of DHHS's strategic domains. These enable DHHS to track changes in Victorians' health and wellbeing levels over time at a population level. Two population level targets explicitly relate to the mitigation of chronic disease, including:
- 25 per cent decrease in premature deaths due to chronic disease by 2025 from 2010 baseline
- halting the rise in diabetes prevalence by 2025.
|
Place-based approaches to healthcare aim to provide Victorians with access to locally available and integrated services. |
The objective of the CHP aligns with the PHW Plan's overall vision for a healthier Victoria. The CHP helps disadvantaged people—who statistically are shown to experience poorer health outcomes—deal with issues such as chronic disease and receive support to adopt preventative health behaviours. In line with the PHW Plan, the CHP provides a place-based approach to healthcare.
The work done by community health services directly supports the measures in the outcomes framework, and the CHP prioritises services for people with chronic diseases. However, DHHS does not collect data that enables it to measure the CHP's contribution to the PHW Plan's vision.
The outcomes framework notes that rigorous evaluation of programs and continuous efforts to understand what works in different contexts should complement its reporting cycle. DHHS has not undertaken any reviews or assessments of the CHP to understand its effectiveness or impact.
2.3 Evidence base for the CHP
An effective evidence base for the CHP should:
- have sound theoretical underpinnings through the use of current, reliable and relevant research
- analyse demographics and indices of disadvantage at the local level to ensure that services and funding are appropriately targeted and address demand
- rigorously evaluate the program's impact on Victoria's priority populations.
Theoretical underpinnings
DHHS published the Community health integrated program guidelines in March 2015. These are a key component of the CHP's underlying evidence base. According to the guidelines' principles, care must:
|
Health literacy is a person's ability to understand health-related information and use this information to inform his or her decisions and actions. Good health literacy is important, as it influences a person's health and experience of the healthcare system. |
- be person centred, culturally responsive, goal directed and evidence based
- take a team approach that supports the client's health literacy levels
- encourage early intervention
- engage with health promotion.
The philosophy of person-centred care is fundamental to the CHP. Person‑centred care supports clients to participate in decision-making while respecting their preferences, diversity and background. DHHS established the CHP's underlying principles following a comprehensive literature review in September 2012. This research component of the CHP's evidence base complies with optimal practice.
DHHS's use of information
While DHHS has a range of demographic information, it does not incorporate this, indices of disadvantage or analysis of local demand issues into the CHP's evidence base. This information would strengthen the CHP, and enable DHHS to appropriately target its services and ensure that priority populations receive effective, timely and appropriate care. DHHS has begun to incorporate demographic and local demand information for other state-funded community health initiatives. For example, when identifying sites for the expansion of its Healthy Mothers, Healthy Babies Program, DHHS assessed various indicators of disadvantage, such as the concentration of child protection reports across the state. DHHS should apply the same methodological rigour to the CHP to ensure that it delivers services based on robust and practical evidence.
The CHP's impact on priority populations
Likewise, DHHS has limited oversight of the CHP's effectiveness. As discussed in Part 4 of this report, DHHS's key performance measure for the CHP focuses solely on the quantity of service hours delivered. This impairs DHHS's ability to improve and innovate the CHP's service delivery model, as it lacks information regarding the quality, appropriateness and timeliness of care.
Overall, DHHS's evidence base for the CHP is lacking—it does not adequately reflect Victoria's needs and priorities, and provides limited insight into the impact of the program.
Community health services' contribution to the evidence base
The audited community health services advised us that they maintain their own evidence base. These reflect the needs of their local areas and align with their broader strategic directions. DHHS should leverage the skills and knowledge of the sector when planning service delivery.
For example, Bendigo Community Health Service funds a Strategy, Planning and Analysis team to evaluate current research and produce guidance. This ensures that its services align with optimal practice. In July 2017, the team published an internal guide Scoping of Service Delivery Models for Generalist Counselling, which outlines the benefits, risks and challenges of various approaches to care, such as telephone psychotherapy and online counselling. Guidance like this enables Bendigo Community Health Service's clinicians to offer innovative services and make informed treatment decisions while maximising their client‑ facing time. DHHS does not specifically fund research teams at community health services, however, Bendigo Community Health Service has found that the advantages outweigh the cost. DHHS could better leverage such work across the CHP.
2.4 Funding for the CHP
DHHS funds community health services to deliver the CHP to Victoria's priority populations. To do this effectively, DHHS should:
- ensure that the CHP's unit prices for one hour of nursing and one hour of allied health care accurately reflect the current costs of service delivery
- ensure the amount of funding allocated to the CHP meets the needs of the Victorian population
- ensure that the CHP's funding is distributed according to need.
The evolution of the CHP's funding model
DHHS's unit pricing for service delivery aims to fund an hour of care, as well as the community health services' associated costs.
|
Governments may fund programs through 'block funding.' This means that the money comes with general spending instructions. Activity-based funding, on the other hand, has stricter provisions. |
DHHS adopted its previous model, the Primary Health Funding Approach, in July 2002. It included three major components:
- a unit price for service delivery
- block funding for health promotion activities (no longer part of the CHP funding model)
- a resourcing component to support any associated infrastructure costs.
DHHS commissioned a review of the Primary Health Funding Approach in 2004, which evaluated different aspects of the model. This included a survey of community health services' expenditure, visits to 20 community health services and document analysis. The consultant's report recommended that DHHS collect further evidence to inform the unit price.
DHHS's 'Frequently Asked Questions' fact sheet, dated October 2008, introduces its new funding model. The fact sheet states that DHHS undertook further work following the consultant's report before deciding on a model.
DHHS formed a steering committee to oversee the implementation of the funding model. Meeting notes from the steering committee note that the unit price for the CHP is the same as that of the Home and Community Care Program, for people aged over 65, which has transferred to the Commonwealth, and the continuing Home and Community Care Program for Younger People funded by the Victorian Government. However, DHHS has not been able to provide us with the evidence of further work undertaken to inform the development of the Primary Health Funding Approach for the CHP.
DHHS's current funding model
Unit costing
DHHS annually updates its funding requirements through the Policy and funding guidelines. This document specifies the current unit price for service delivery.
DHHS advised that the CHP's unit prices rise in line with DHHS's internal indexation, approved by the Victorian Government. The level of indexation has been between 1.5 per cent and 2.5 per cent each year for the past five years. However, DHHS has not reviewed the unit cost for the CHP since 2007—so it does not know whether the unit price accurately reflects the current cost of care in community health services.
Funding amount for the CHP
The CHP currently receives approximately $105 million in funding for the delivery of nursing and allied health services. The program received additional recurrent funding of about $1 million from 2013–14. However, DHHS has not undertaken a significant review of the CHP's total funding allocation to determine whether it addresses the needs of Victoria's priority populations.
Funding distribution
DHHS describes its current CHP funding distribution model as population based. However, DHHS lacks documentation to show how it developed the model or what calculations it uses to allocate funding to community health services.
In a December 2013 memorandum to the Minister for Health regarding additional recurrent funding, DHHS noted that it allocated the funding according to population growth, social disadvantage, the catchment population of children and the percentage of developmentally vulnerable children. This appears to be a sound approach, however, DHHS cannot produce any evidence to demonstrate its application.
DHHS has not reviewed community health services' funding allocations since 2007. Community health services located in growth corridors have not received an increase in funding proportionate to the increase in their area's population. In addition, DHHS's funding allocation does not recognise demographic changes, such as increases in disadvantage.
Therefore, the funding model may compromise the CHP's ability to provide effective healthcare to Victoria's priority populations.
Proposed new funding model
DHHS is currently considering the development of new funding models for the spectrum of healthcare that Victoria funds and manages, including the CHP. DHHS has undertaken preliminary work, including commissioning research and a literature review. This includes consideration of a new funding model based on packaged funding for specific cohorts whereby community health services are funded for the number of enrolled clients at their service.
Clients with greater complexity and those from the CHP's priority populations would attract higher payments. DHHS's executive board has approved further research, analysis and engagement with the sector before it implements any reform options.
This proposed funding model is more closely aligned to the objectives of the CHP than DHHS's current funding model.
3 Access and demand
Timely access to primary care services—such as the CHP—is important for Victoria's priority populations, as early intervention may prevent people's conditions from worsening. This can also reduce pressure on the health services providing acute care.
DHHS provides community health services with set CHP funding on an annual basis. With limited resources available, it is important for community health services to manage access and demand at the local level. Similarly, DHHS must monitor the state's access and demand issues to effectively oversee the CHP.
In this part of the report, we examine DHHS's guidance regarding the management of access and demand, and its implementation at community health services. We also assess the demand management analysis undertaken by DHHS and community health services to ensure that it supports the provision of timely and effective care.
3.1 Conclusion
Timely access to the CHP is important to prevent individuals being admitted to hospital and to support their health and wellbeing. At a local level, the community health services we audited had effective strategies in place to manage their known demand. However, as a whole, DHHS cannot demonstrate that the CHP is providing timely and equitable access across the state and meeting the demand and needs of its priority populations.
3.2 Guidance for access and demand
Community health services require guidance on access and demand procedures to deliver the CHP effectively. DHHS's guidance should ensure that community health services prioritise access for clients who are most in need.
DHHS's framework for managing demand
DHHS's framework for managing access to the CHP is outlined in its key guidance document Towards a demand management framework for community health services (demand management framework). The demand management framework assists community health services to prioritise their clients and address pressures at each stage of service delivery—inflow, flow through and outflow.
Inflow
The demand management framework provides community health services with a model for inflow—or intake of clients. The initial needs identification (INI) is an important screening process that aims to identify a client's presenting and underlying needs. DHHS provides Service Coordination Tool Templates for INI, which community health services use to seek information about clients' living arrangements, health behaviours and psychosocial status. In 2016–17, INI accounted for almost 8.5 per cent of the total service hours delivered. This demonstrates the importance of funding for this process.
To ensure community health services treat clients in the appropriate order, INI enables practitioners to triage clients as priority 1, 2 or 3. Priority 1 clients require urgent intervention, whereas priority 3 clients can safely wait for care. There are, however, no clinically recommended treatment time frames for each priority group.
To facilitate the triage process, DHHS provides community health services with two sets of tools for prioritising clients:
- a generic priority tool that identifies priority populations, those at risk of imminent harm, and people with multiple complex needs
- clinical priority tools for seven of the CHP's allied health specialties.
Flow through
Flow through describes the client's journey through the community health service until they exit. The guidelines provide a number of processes to effectively manage client flow through. These include:
- waiting list management
- appointment processes
- particular models of service delivery, such as group-based work or goal‑based intervention.
The guidelines are not prescriptive and provide community health services with the autonomy to implement and tailor processes to their individual practices.
Outflow
Outflow focuses on ensuring clients exit the community health service safely and appropriately. The demand management framework states that community health services should start planning a client's exit from the service at the first appointment. There are a number of reasons that people will exit care, including:
- only needing short-term intervention
- reaching their goals
- needing to be referred to another service for different care.
Usefulness of the demand management framework
DHHS published the demand management framework in 2008. While it provides guidance for community health services, it is now out of date. For example, it refers to A Fairer Victoria—a social strategy launched in 2005.
The demand management framework contains suggestions for community health services on how to undertake different processes, but since DHHS produced this guidance, some community health services have implemented different demand management processes—for example, for dealing with clients cancelling or failing to attend appointments. Community health services we audited commented that they were not aware of what demand management techniques other services were using and were interested in having more guidance on demand management techniques.
DHHS should review the demand management framework to determine whether it is comprehensive, evidence based and in line with current processes.
3.3 Administering the demand management framework
Community health services are responsible for administering the demand management framework. We discussed with community health services how they implement the framework in their day-to-day work.
Inflow
Various sources—such as general practitioners, health services and other community organisations—refer clients to the CHP. Individuals can also refer themselves to community health services.
Service access
All the audited community health services have service access staff to manage client intake. Typically, service access staff receive referrals from internal or external practitioners, or calls directly from clients. Service access staff are generally responsible for determining whether a client is appropriate for the CHP, initially triaging the client and scheduling an appointment. If no appointments are available, the client may be placed on a waiting list. This process takes anywhere from 10 minutes to an hour and depends on the client's complexity.
Community health services have guidelines for service access staff that are consistent with DHHS's demand management framework. Coordinating service access is an important process, as it ensures that clients receive the right care at the right time and can access services efficiently and effectively. DHHS does not specifically fund service access through the CHP, but incorporates it into the hourly cost of care.
As discussed in Part 2, DHHS has not reviewed the CHP's unit price and consequently does not know if it adequately covers community health services' cost of delivering services.
Priority tools
Service access staff first assess incoming clients against the generic priority tool. If the client is from a priority group, they receive priority 1 status. If not, service access staff use the clinical priority tools to determine whether an individual is a priority 1, 2 or 3.
DHHS developed clinical priority tools in conjunction with community health services and consumers in 2008. It formed working groups for funded allied health specialities—nursing, counselling, dietetics, adult and paediatric occupational therapy, physiotherapy, podiatry and speech pathology.
All the audited community health services commented that DHHS's clinical priority tools are general in scope. However, as shown in the case study in Figure 3A, this gives community health services the flexibility to adapt them to reflect local practice.
Figure 3A
Case study: Bendigo Community Health Service's podiatry service
|
Bendigo Community Health Service has a busy podiatry service. The podiatry team has created its own clinical priority tools to maintain consistency among practitioners. It uses the University of Texas (UT) Foot Wound Classification System to grade wounds according to their severity. This system enables the health service's podiatrists to objectively assess their clients' needs. For example, using the health service's clinical priority tool, a client with a category 3 wound according to UT's system (a wound that penetrates the bone or joint and requires immediate medical attention) would be categorised as priority 1. In addition, Bendigo Community Health Service collaborates with Bendigo Health's integrated community health service to ensure that high-risk clients receive clinically appropriate care in a safe environment. This partnership represents best practice, as it aims to ensure that clients receive the right care at the right time in the right place. |
Source: VAGO based on Bendigo Community Health Service documentation.
As DHHS last updated its clinical priority tools in 2008, community health services commented that they had to adjust DHHS's clinical priority tools to reflect current research.
In 2008, DHHS engaged consultants to evaluate initial use of the tools at eight community health services. They evaluated the tools' use by service access staff and clinicians, and tested their effectiveness in further discussions with clients.
The consultants presented a report of their findings to DHHS in 2009. The report raised specific issues with the clinical priority tools and made a number of general recommendations, including that DHHS:
- implement a mechanism for continual feedback on the clinical priority tools so DHHS can understand how they are used in practice
- review the relevant literature on clinical disciplines to ensure the clinical priority tools reflect an evidence-based approach.
DHHS advised that it would consider these recommendations in the context of its resources and priorities. There is no evidence that DHHS has implemented recommendations from this 2009 review.
DHHS's clinical priority tools aim to provide consistency in the way community health services prioritise CHP clients across Victoria. It is positive that community health services have modified the tools to reflect their local practice. However, community health services are doing this independently. This means that all 85 community health services are spending time and resources updating the tools, despite DHHS neither facilitating nor funding the process. In addition to this duplication of effort, there is a risk that community health services may have inconsistent guidelines which means some clients with the same level of need may not receive the same level of access or timely intervention.
DHHS should update the clinical priority tools to promote consistent practice and reduce duplicated effort among community health services.
Flow through and outflow
The amount of time and resources required to treat individual clients influences the community health service's ability to treat new people. This impacts the number of clients that flow through community health services. Almost all community health services reported high demand for their allied health specialties. To ensure that new clients flow through efficiently and effectively, community health services have strategies that manage access. Strategies include:
- running group sessions for some services, such as speech therapy
- regularly reviewing client care needs to identify the earliest possible exit from the community health service.
Analysis of the CHMDS shows that 90 per cent of the CHP's clients access services for 10 sessions or fewer—see Figure 3B. While some clients may only need short-term intervention, this demonstrates that community health services are implementing strategies to manage outflow and provide access to more clients.
Figure 3B
Clients accessing CHP treatment
Note: The data range 11–370 is an aggregated figure.
Source: VAGO based on DHHS documentation.
DHHS's oversight of access at community health services
DHHS receives quarterly data from community health services on the number of service hours delivered in the CHP. Divisional offices use this data to assess whether community health services meet their targets, however, DHHS has no oversight of whether access is equitable. This is due to limitations in DHHS's performance measures and dataset, discussed in Part 4.
3.4 Demand in community health services
Measuring demand is important for the CHP—at a whole-of-state level, it allows DHHS to determine whether the CHP receives adequate funding and is meeting community needs.
DHHS's past and current demand measurement processes
Managing demand for the CHP is complex. There is no evidence that DHHS has undertaken any analysis of potential or hidden demand across Victoria. However, DHHS has recently commenced a demand forecasting project.
DHHS's oversight of current demand pressures is further limited, because the CHMDS contains incomplete and inaccurate data fields. For example, DHHS requires community health services to collect the concession card status of CHP clients, however, this field is blank or inadequately described in 44.5 per cent of records. This compromises DHHS's ability to understand whether community health services adequately manage demand to ensure that priority populations receive preferential and timely access to care. DHHS is undertaking a data streamlining project which it believes will support improved data collection practices by agencies. DHHS also does not collect waiting list data, which further limits its oversight of the state's demand pressures.
As discussed in Part 4, DHHS's key performance measure for the CHP focuses solely on the number of service hours delivered. Without further information, DHHS is unable to determine whether the CHP adequately services its priority populations with sufficient care, in the right place and within a reasonable time.
Action taken to improve DHHS's demand measurement processes into the future
DHHS has begun to evaluate demand in key catchment areas to address the gaps in its knowledge. For example, in August 2017, it produced a draft version of the Design, service and infrastructure plan for the Northern Growth Corridor. The report provides a high-level framework for planning in the northern growth corridor, which has experienced rapid population growth in recent years. The document profiles the catchment's diversity, service use, level of socioeconomic disadvantage, access to education, and prevalence of health risk factors, such as smoking rates. It aims to strengthen the northern growth corridor's existing healthcare network and enhance the flexible use of services to lessen disparities for disadvantaged Victorians. DHHS intends for future modelling to explore the rate of people moving into the area as well as projected use of services.
In addition, DHHS's System Intelligence and Analytics Branch has recently produced a project specification to understand how current and past investments in community health services have influenced activity patterns. It intends to use past activity data—2008–09 to 2016–17—and population estimates to gain insight into future activities and demand, and increase DHHS's knowledge of its clients. The document outlines a detailed methodology, identifies various risks, and assumes that no changes will be made to the CHP's funding formula. The project specification demonstrates DHHS's commitment to improving its oversight of demand pressures in community health services and is a step in the right direction.
Community health services' demand measurement processes
DHHS's demand management framework states that community health services should keep waiting lists to effectively manage their clients. The audited community health services all keep waiting lists and use these to monitor access. If possible, community health services avoid placing clients on waiting lists, as long delays can discourage and frustrate both parties. Waiting lists cause an administrative burden, as staff must generate acknowledgement letters, regularly maintain the waiting list, and conduct follow-up calls and status updates. Community health services have various strategies for managing demand, including:
- involving practitioners and clinicians in more detailed screening to ensure that clients are appropriately triaged, as this influences waiting times and the provision of effective care
- undertaking group therapy where clinically appropriate, for example, speech pathology for children aged five and under
- expediting access to speech pathology services for children about to start school.
DHHS acknowledges that funding for the CHP is capped, which has consequences for community health services' ability to manage their demand pressures. DHHS also acknowledges the significance of robust service planning and funding model development to support community health services to improve access for priority populations.
These funding constraints have consequences for community health services' ability to manage their demand pressures. For example, five community health services that we spoke to advised that they are unable to advertise their services or proactively seek clients, as they cannot provide care to all eligible people within the community.
Gippsland Lakes Community Health noted that in rural areas, people are under‑serviced and need is often only noticed when people travel to other areas to access service. Therefore, people in rural areas need services placed in locations where there is demand to improve access.
In addition, workforce retention rates also affect community health services' ability to meet demand. Sometimes, allied health professionals are difficult to recruit. Rural and remote community health services are affected by this more severely, as they are commonly the sole providers of allied health services in their communities. Such allied health positions may remain vacant for extended periods, which affects the community health service's ability to care for its local population.
For example, Orbost Regional Health has difficulty attracting allied health specialists—particularly physiotherapists—to its region, as it is in an isolated rural location. It often relies on graduate physiotherapists to fulfil its needs, however, most work for the community health service for only 12–18 months before leaving. When Orbost Regional Health is without a physiotherapist, it refers its clients to neighbouring services, such as Gippsland Lakes Community Health. The health service advised that this impacts access for its clients, as the region lacks regular public transport services.
To address this issue, Orbost Regional Health collaborates with different community health services across the region to share allied health specialists when they are in limited supply. For example, after the health service was unable to recruit a physiotherapist, it arranged for one from Bairnsdale to visit on a weekly basis so that its clients could continue to receive timely care. Sometimes, rural community health services—such as Orbost Regional Health —will fill service gaps with locums, however, this is an expensive option and is considered a last resort.
4 Performance and quality
Performance monitoring and reporting promotes transparency, good governance and effective management. It delineates the roles and responsibilities of agencies and is government's key accountability mechanism. Monitoring and reporting cycles require fair, relevant and consistent measures to effectively scrutinise performance.
DHHS collects data from various sources—such as feedback from staff and clients, clinical activity and local intelligence—to paint a picture of day-to-day performance at community health services.
In this part of the report, we examined whether DHHS's performance management system allows it to:
- demonstrate achievement of the CHP's objectives
- hold community health services accountable for their performance
- test and evaluate evidence-based strategies for broader policy-making within the sector
- improve the CHP and its service delivery model.
4.1 Conclusion
DHHS's performance management framework is unable to assess whether the CHP meets its objective of delivering effective healthcare services and support to Victoria's priority populations. DHHS lacks insight regarding the timeliness, equity, appropriateness or impact of care because its public and internal reporting largely focuses on the number of service hours that community health services deliver. To assess whether the CHP provides good healthcare outcomes for Victoria's priority populations, DHHS requires both quality-based and outcomes-focused performance measures.
DHHS is beginning to expand its oversight of the CHP through the client experience survey, which is a step in the right direction. While this tool provides insight into clients' experiences of the CHP and, by proxy, its effectiveness, the survey requires further research and evaluation to produce optimal results for the sector. In its current form, it has a low response rate, lacks the methodological rigour of tools used by better practice jurisdictions—such as New Zealand—and is long and cumbersome.
In addition, DHHS could improve its oversight of both registered and integrated community health services by standardising its existing monitoring procedures. DHHS uses the Funded organisation performance monitoring framework (FOPMF) to manage registered community health services, however, this is a relatively new tool and it is not consistently applied. DHHS's four divisions set their own monitoring regime for integrated community health services, which creates further variations in performance management.
4.2 DHHS's performance management system
As shown in Figure 4A, DHHS's performance management system has multiple layers—each with varying objectives. At both the state and agency levels, performance measuring, monitoring and reporting emphasise outputs rather than the effectiveness and impact of care.
Figure 4A
DHHS's performance management system
Source: VAGO.
4.3 State-level performance management
DHHS's public performance measures and reporting
DHHS sets public performance targets each year in the Victorian Budget Paper 3: Service Delivery (BP3). DHHS assesses the performance of community health care using six performance measures. As shown in Figure 4B, only two relate to the CHP.
Figure 4B
DHHS's BP3 performance measures for community health care
|
Performance measure |
Type |
Relevant |
|---|---|---|
|
Number of Better Health Channel Visits |
Quantity |
✘ |
|
Number of referrals made using secure electronic referral systems |
✔ |
|
|
Percentage of Primary Care Partnerships with reviewed and updated strategic plans |
✘ |
|
|
Number of service delivery hours in community health care |
✔ |
|
|
Percentage of agencies with an Integrated Health Promotion Plan that meets the stipulated planning requirements |
Quality |
✘ |
|
Total output cost |
Cost |
✘ |
Note: The performance measure for the number of referrals relates to all referrals made to community health services.
Source: VAGO, derived from BP3.
Two performance measures relate to the CHP, however, these both assess the quantity of care provided. DHHS lacks publicly available performance measures that specifically evaluate the quality, impact or cost of care.
DHHS's public reporting against performance measures
Figure 4C shows DHHS's publicly reported performance measures and performance for the CHP since 2014–15.
Figure 4C
DHHS's performance against targets for selected BP3 measures
|
Performance measure |
2014–15 |
2015–16 |
2016–17 |
2017–18 |
||||
|---|---|---|---|---|---|---|---|---|
|
Target |
Actual |
Target |
Actual |
Target |
Actual |
Target |
||
|
Number of referrals made using secure electronic referral systems |
250 000 |
250 000 |
250 000 |
250 000 |
250 000 |
125 000(a) |
250 000 |
|
|
Number of service delivery hours in community health care |
988 000 |
1 055 000 |
988 000 |
1 062 000 |
1 000 000 |
1 101 000 |
1 015 000 |
|
(a) According to DHHS's 2016–17 Annual Report, this result is lower than the target due to a reduction in the number of electronic referrals made through the state system, following the introduction of additional referral portals associated with Commonwealth initiatives—My Aged Care and National Disability Insurance Scheme—that redirect flow to the Commonwealth systems.
Source: VAGO based on DHHS annual reports and BP3.
The Department of Treasury and Finance's performance management framework outlines the mandatory requirements for presenting and assessing performance information. According to the Department of Treasury and Finance, departments should 'develop performance measures that can demonstrate service efficiency and effectiveness, and cover all major activities of the output'.
DHHS's measures do not comply with this mandatory requirement, as they cannot determine whether the CHP fulfils these criteria. For example, DHHS does not publicly explain how or why the number of service hours changes over time. As a result, it is difficult for the public to assess whether annual fluctuations in service hours are due to improved efficiencies, over‑performance, or factors beyond the community health sector's control.
Likewise, current performance measures do not analyse the CHP's quality. While increasing the number of service hours may suggest that the CHP can support more clients, leading to better health outcomes, unless there is public assurance that care is high quality and effective, the program's achievements are unknown. Good measures of program effectiveness and quality generally include consultation with clients, such as analysis of client satisfaction surveys, as well as objective measures of health improvements. Importantly, this conforms to the sector's overarching philosophy of person-centred care and provides insight into the CHP's value.
In addition, while using the number of referrals made using secure electronic referral systems as a measure offers some insight into the program's efficiency, it is largely a comment on the sector's technical integration. As a measure, it is somewhat redundant, because the community health sector has continuously met DHHS's target since its introduction in 2011–12. The target of 250 000 has been precisely met every year except 2016–17, which raises questions regarding the accuracy of DHHS's reporting.
Last year, the sector only met 50 per cent of its target, however, this was due to the introduction of new referral portals at the Commonwealth level. DHHS noted it will reduce the 2018–19 target to 75 000 to reflect this change in referral pathways.
DHHS's internal performance measures and reporting
DHHS's internal reporting for the CHP uses the same performance measure—'the number of service hours delivered'. Community health services receive quarterly feedback from DHHS regarding their performance through the Funded Agency Channel. The Funded Agency Channel is a central platform that DHHS uses to convey information to community health services, such as procedural changes. DHHS's quarterly performance reports analyse the number of service hours that community health services have delivered against their prescribed targets. This quantitative review lacks supporting commentary and does not promote or encourage good practice.
In addition, this performance measure does not align with the program's objective—to provide effective healthcare services and support to Victoria's priority populations. According to DHHS's guidelines, effective care is culturally responsive, goal directed, health promoting and evidence based. However, the CHP's current external performance measure is incapable of reflecting these principles, because it lacks a person-centred focus and cannot determine whether care benefited the client. Likewise, as this measure fails to assess whether the CHP targets the right people, it does not encourage community health services to provide preferential access to Victoria's priority populations. Therefore, DHHS's internal reporting cannot determine whether the program meets its overall objective.
DHHS should consider implementing quality-based performance measures that assess client satisfaction following treatment, and outcomes-focused performance measures that assess self- and/or clinician-reported changes in health-related outcomes, behaviours and knowledge.
4.4 Action taken to address the gaps in current performance measures
In 2014–15, DHHS piloted the Victorian Community Health Indicators Project to strengthen the program's evidence base and foster a culture of continuous improvement. The project aimed to deliver two complementary suites of indicators—one focused on processes, the other on outcomes.
Process-based indicators evaluate the clients' administrative journey from entry to discharge, while outcomes-based indicators assess the impact of care. To date, DHHS has only completed its set of process-based indicators.
Process‑based indicators provide a particular view of service delivery, as they test the community health services' performance against DHHS's minimum requirements. Rather than outcomes, they enable community health services to assess a different aspect of care—its implementation—which reflects the client experience of service delivery. Process-based indicators represent better practice, as they conform to the sector's key strategic objective of person‑centred care.
DHHS's process-based indicators include measures such as:
- the percentage of clients with multiple or complex needs who have a care plan
- the percentage of complaints acknowledged by the organisation within twoworking days of receipt of the complaint.
In 2016–17, DHHS stopped collecting data against the process-based indicators due to feedback from the sector. While the indicators were positively received by community health services, they imposed significant administrative burden, as they required community health services to collect information that was supplementary to DHHS's standard reporting template. The sector's diverse range of client management systems was also an issue, as the necessary software updates were difficult and expensive.
To address this burden, DHHS is attempting to streamline the indicators' collection as part of its Community Health Data Alignment Project. DHHS has begun to embed the following five indicators into the CHMDS following consultation with the sector:
- timely initial needs identification
- interpreter use
- waiting time for highest-priority clients
- waiting time for mid-priority clients
- waiting time for lowest-priority clients.
DHHS advises that it will continue to consult with the sector as it integrates additional indicators into the CHMDS.
However, the absence of a complementary suite of outcomes-based indicators diminishes the project's overall value, as DHHS cannot conclusively determine whether the CHP provides effective health care to Victoria's priority populations. According to the Victorian Health Priorities Framework 2012–2022: Metropolitan Health Plan, poor care coordination increases the risk of poor outcomes for people with chronic disease. To analyse the relationship, DHHS requires information on both processes and outcomes.
4.5 Agency-level performance management across the sector
DHHS has four divisions—North, South, East and West. Each division operates several regional offices that are located across the state. Regional offices assign program advisors to the community health services within their jurisdiction. Program advisors are community health services' primary point of contact and carry out most of DHHS's monitoring duties.
DHHS's performance management system differs between registered and integrated community health services. DHHS's oversight of registered community health services is more rigorous than for integrated community health services, because the integrated health services are subject to the broader accountability systems of the hospital sector.
Agency-level monitoring considers community health services through a holistic lens and evaluates aspects of governance and management. It goes beyond program-level monitoring and assesses structural issues that may affect performance.
Monitoring of registered community health services
Every four years, DHHS sets a service agreement with registered community health services. This outlines the responsibilities of both parties to deliver high‑quality services and formalises their commitment to improving Victoria's health and wellbeing.
Through the service agreement, DHHS allocates funding to each program and stipulates any associated requirements. DHHS's regional offices use the FOPMF to assess whether community health services comply with their service agreements.
The FOPMF addresses the Minister for Health's gazetted performance standards, which are:
- governance—the agency must be effectively governed at all times
- management—the agency must be effectively managed at all times
- financial management—the agency must maintain effective financial management at all times
- risk management—the agency must effectively manage the risk associated with its business to ensure continuous, safe, responsive and efficient services
- quality accreditation and service delivery—the agency must demonstrate that it is able to meet quality and safety standards as established by an independent accreditation body.
The Victorian Government applies the FOPMF to various initiatives across DHHS and the Department of Education and Training—it is not specific to community health. FOPMF assesses foundational business elements, such as governance, safety and workforce arrangements. Program advisors may scrutinise the CHP's performance as part of the community health services' broader delivery platform, and some explicitly identify the CHP when assessing performance risks and issues.
DHHS rolled out the FOPMF in January 2016 alongside an 18-month change management process. As the FOPMF is relatively new, there are some inconsistencies in the way DHHS applies it across community health services. DHHS has advised us that it provides regular training opportunities to its divisional staff to increase their familiarity with the FOPMF and its tools.
The FOPMF has two mandatory requirements—monitoring checklists and the annual desktop review. Program advisors complete these tasks with the aid of a risk assessment tool and Live Monitoring log. Figure 4D illustrates the elements of the FOPMF for monitoring registered community health services.
Figure 4D
Framework for monitoring registered community health services
Note: SAMS2 = Service Agreement Monitoring System.
Source: VAGO.
Funded organisation performance monitoring framework
Monitoring checklists
The FOPMF contains two checklists. These are the:
- service agreement monitoring checklist—which focuses on service delivery
- organisational compliance checklist≠—which primarily assesses the community health services' governance arrangements.
Program advisors must complete the FOPMF checklists annually for registered community health services. The checklists outline DHHS's expectations for effective service delivery and support program advisors to conduct inquiries in line with the minister's gazetted performance standards.
To complete the checklists, program advisors sight evidence and determine the agency's level of compliance. Program advisors rate the agency's performance against each standardised question, and use the risk assessment tool to assign one of the following severity ratings:
- 0—no issue
- 1—minor
- 2—moderate
- 3—major
- 4—critical.
How program advisors fulfil their duties is also at the discretion of their respective divisional offices. For example, to complete the monitoring checklists, program advisors may only require one face-to-face meeting with the agency, with follow-up conversations required to fulfil all the requirements. DHHS does not require program advisors to conduct additional monitoring—they must use their professional judgement.
Risk assessment tool
The risk assessment tool assists program advisors to complete the checklist and outlines follow-up actions based on their results. DHHS's guidelines recommend that regional offices perform a specific set of actions to address issues.
DHHS's risk assessment tool lacks consistent definitions for program advisors. It describes each severity rating—or particular level of risk—using a series of hypothetical scenarios. For example, a 'minor disruption' in the provision of services results in a 'minor' severity rating, whereas a 'modest disruption' equates to a 'moderate' severity rating. In the absence of quantifiable thresholds, program advisors must subjectively judge the difference between minor and modest. This leads to inconsistent performance management across DHHS's divisions.
As shown in Figure 4E, DHHS's West division created the performance escalation framework (PEF) to overcome these issues and support consistent application of the FOPMF across its agencies. DHHS's central office is aware of this document, however, DHHS does not know at this stage whether it will implement it across the state.
Figure 4E
West division's performance escalation framework
|
The West division's PEF helps the division's staff to assess and remediate issues in a consistent manner. It assigns a point-scale to three major risk areas or 'categories,' which program advisors use to determine an agency's PEF score. If a program's PEF score surpasses the thresholds for the major risk categories—levels 1, 2 and 3—the division intensifies its monitoring. As shown below, the seniority of the team member responsible for ongoing monitoring activities increases with the agency's PEF score. Category 1 compares a program's reported activity against its allocated target. This is an important indicator, as under- or over-performance may point to other issues, such as data entry errors or service delivery failures. Category 2 refers to the number of reportable periods that a program has failed to achieve its target. This enables staff to identify systemic issues, as sustained under-performance may require organisational changes. Finally, Category 3—'other identified risk factors'—assesses the number of 'minor' or 'moderate' issues logged in the agency's Live Monitoring log. This strengthens existing monitoring procedures, as the FOPMF only escalates 'major' or 'critical' issues to the director or manager, and lacks thorough guidance for the remediation of other problems. The West division's increased oversight encourages timely risk mitigation, which may prevent smaller issues from escalating. As shown in the figure below, program advisors also weight a program's PEF score according to its financial value. This assists staff to prioritise their duties across a range of agencies and programs. The PEF enables the West division's program advisors to discharge their monitoring duties in a standardised manner, which creates greater consistency and ensures that the right people address issues at the right time. |
Source: VAGO based on documentation from DHHS's West division.
Live Monitoring log
The Live Monitoring log is a key component of the Service Agreement Monitoring System, DHHS's primary management platform. According to DHHS's guidelines, program advisors must use the log to catalogue any issues and manage their agencies' remediation plans.
DHHS's guidelines also advise program advisors to promote their agencies' 'success stories' through the Live Monitoring log to encourage greater recognition of their innovative projects.
DHHS's divisions used the Live Monitoring log inconsistently. For example, the North division identified two 'moderate' performance risks at one community health service in 2016–17. The program advisor flagged these issues in the appropriate checklist but failed to enter them into the log. This limits the North division's ability to identify trends, as it lacks a centralised history of the community health service's performance.
In contrast, the North division's checklists identified four issues at another community health service. The program advisor appropriately catalogued these issues in the Live Monitoring log alongside the health service's remediating plans. This complies with DHHS's guidelines and represents good practice, as the division has oversight of the actions undertaken to improve performance.
We heard from both divisional offices and community health services that some program advisors prefer not to register issues in the Live Monitoring log, as each entry generates multiple emails, which clutters their inboxes. This practice causes confusion for the affected community health services, as DHHS's behaviour and expectations differ from program advisor to program advisor.
We did not see any evidence of DHHS promoting innovative practices through the Live Monitoring log. Instead, most program advisors flagged good practice in the annual desktop review. It is unknown how cataloguing 'success stories' on either platform provides community health services with greater recognition, as their performance information is neither visible to their peers nor promoted within DHHS.
Desktop review
Program advisors collate an agency's annual monitoring portfolio—including the completed checklists, Live Monitoring log and any additional communication—to produce a desktop review. Desktop reviews aim to identify any risks or trends and inform the agency's overall monitoring-level. If the desktop review identifies significant issues, DHHS may intervene or initiate a service review. This involves a full-scale investigation into the agency's activities and performance.
There is a degree of duplication between the content of the annual desktop review and the monitoring checklists. As these tools provide point-in-time analysis, their effectiveness is reduced if they are completed within a short time frame.
For example, DHHS finalised the 2016–17 desktop reviews for North Richmond Community Health and cohealth within two months of completing the checklists. The relevant offices, therefore, discharged their minimum monitoring duties within a short window. This may limit DHHS's identification of emerging risks, as DHHS's annual scrutiny covered a single quarter of the year. The West division addresses this potentially limited view through additional meetings with cohealth, however, the North division did not provide us with evidence of continued engagement with North Richmond Community Health.
South division's supplementary monitoring tools
As shown in Figure 4F, the South division has created two supplementary tools to help it identify activity-based issues—the 'traffic light' performance matrix and issues log. These give the division oversight beyond the FOPMF's minimum monitoring requirements and enable program advisors to track trends over various years. The tools also facilitate continued engagement with health services, as they create a centralised service history that assists program advisors to efficiently monitor agencies. DHHS's central office was not aware of these supplementary monitoring tools and should consider implementing them across the state.
Figure 4F
South division's 'traffic light' performance matrix and issues log
|
The South division's 'traffic light' performance matrix enables program advisors to evaluate the sector's performance from two different perspectives. As shown below, the vertical axis of the 'traffic light' matrix lists the South division's funded agencies, while the horizontal axis outlines the range of programs managed in the division. Each row highlights the performance of a single funded agency at the program level, while each column evaluates the program's total output. This allows the divisional office to identify whether performance issues are present across an entire program, or isolated to a particular agency. Source: DHHS's South division. The 'traffic light' matrix allows program advisors to identify performance risks at a glance and pinpoint emerging trends. It also tallies the 'unused dollars' for each funded agency. This functions as an additional performance measure for the division, as underspending may indicate other performance issues, such as workforce shortages, data entry errors or service delivery failures. The South division also has an issues log for each funded agency. The issues log tracks an agency's quarterly performance across various programs—including the CHP—for a range of years. It compares the number of service hours delivered against the agencies' prescribed target, and includes a space for qualitative remarks. While the 'comments' section does not explain every aspect of under- or over‑performance, it provides valuable information regarding any issues. For example, in 2016–17, Latrobe Community Health Service delivered 0 per cent of its Healthy Mothers, Healthy Babies Program target for quarters one, two and three and only 1 per cent in quarter four. The 'comments' section explains that Latrobe Community Health Service was unable to recruit for this position until the following financial year. This example demonstrates that the South division has continuous oversight. |
Source: VAGO based on DHHS documentation.
Monitoring of integrated community health services
In comparison to registered community health services, integrated community health services experience less formal monitoring from DHHS. This is because they are subject to the broader accountability systems of the hospital performance team, which operates from DHHS's central office. Each year, DHHS negotiates Statements of Priorities with Victoria's public health services. The Statement of Priorities is a legislative requirement that outlines the health services' key deliverables and performance targets, and assigns an annual budget to each major activity. DHHS uses the Victorian Health Services Performance monitoring framework (the framework) to determine whether agencies comply with their Statements of Priorities.
DHHS's central office and regionally based rural health teams are responsible for monitoring the performance of Victoria's public health services, public hospitals and multipurpose services. To oversee these health services, DHHS conducts quarterly meetings with each agency. Quarterly performance meetings assess the health service's performance against its Statement of Priorities and generally focus on acute and sub-acute activities, such as the elective surgery waiting list.
Victorian Health Services Performance monitoring framework
While DHHS's central office monitors the overall health service, its divisions are responsible for assessing health services' delivery of the CHP. The CHP, therefore, lacks standing representation at health services' quarterly meetings with DHHS's central office.
DHHS's divisional directors and regional program advisors do not conduct equivalent quarterly meetings with community health services. Instead, each office decides on individual monitoring schedules for its agencies. This diminishes DHHS's oversight of the CHP, as program advisors lack a standardised framework for continuous engagement. While some program advisors communicate with their agencies on a regular basis, others are less frequent.
As the framework's primary focus is acute and sub-acute performance, it has minimal relevance for integrated community health services. For example, none of its 98 indicators directly scrutinise the provision of community health care. As a result, DHHS's framework cannot assess whether integrated community health services deliver timely, safe or effective care to priority populations.
DHHS's engagement with integrated community health services
As DHHS's divisions do not have a formal monitoring framework specific to integrated community health services, there is no guidance regarding the frequency or scope of monitoring activities. As a result, DHHS's divisions take different approaches to monitoring across integrated community health services.
Monitoring of metropolitan and regional health services
The South division does not hold quarterly performance meetings with Monash Health or Peninsula Health. Instead, DHHS has 'annual update' meetings with both agencies. The South division supplements this oversight through informal correspondence, such as email chains. In contrast, the North division holds quarterly performance meetings with Bendigo Health.
In 2016–17, Bendigo Health's internal restructure affected the North division's monitoring schedule, and only two out of four meetings occurred. During this period, Bendigo Health's board and its community health service experienced various leadership changes. DHHS's Victorian Health Services Performance monitoring framework explicitly identifies 'recent turnover' as an underlying risk factor, as it may cause significant administrative issues. We saw no evidence of this issue being discussed at the broader health service's meetings with DHHS's central office.
While quarterly meetings are not mandatory for community health services, DHHS should have monitored Bendigo Health more closely during this period to ensure that this disruption did not impact the provision of care. DHHS advised us that monitoring via phone conversations occurred during this time. However, a lack of formal documentation creates issues if program advisors change duties, and may be difficult to verify.
Monitoring of small rural health services and multipurpose health services
In addition to divisional monitoring, DHHS's Rural Health team conducts quarterly performance meetings at East Wimmera Health Service and Orbost Regional Health. The meeting minutes demonstrate that DHHS has regular contact with both agencies and strong oversight of emerging risks.
Although community health is not a standing agenda item, East Wimmera Health Service's director of clinical and community health and Orbost Regional Health's director of community health attend their agencies' respective meetings. This means that there is a consistent communication channel between DHHS and the community health service.
DHHS publishes performance information from East Wimmera Health Service and Orbost Regional Health in the Small Rural Health Services' Monitor (the monitor) on a quarterly basis. The monitor benchmarks agencies in accordance with DHHS's key performance domains. As a result, it is largely concerned with clinical governance and delivery of acute services. While the monitor reports the number of service hours delivered in community health, it lacks contextual information—such as the effect of workforce shortages or the introduction of innovative programs—which diminishes its relevance to the broader sector.
4.6 The Divisional Performance Assurance and Compliance process
Both registered and integrated community health services are subject to DHHS's Divisional Performance Assurance Compliance (DPAC) process. The DPAC process, conducted biannually, aims to encourage continuous quality improvement through regular and transparent discussions with agencies. According to divisional staff, the DPAC process is a key accountability process for integrated community health services because—unlike their registered counterparts—they lack a formalised monitoring framework.
The DPAC process requires divisional directors to inform DHHS's executive board of their respective community health services' performance. Its purpose is to assure the board that divisional staff appropriately discharge their duties as relationship managers and performance monitors. While the DPAC process primarily focuses on outputs, directors also discuss key issues within their division, highlight areas for improvement and promote better practice.
The DPAC process is beneficial, as it ensures that community health services' performance is visible to the upper levels of DHHS management. However, it should function as an additional layer of scrutiny rather than as the sole monitoring mechanism for integrated community health services.
4.7 Data reporting for performance management
Complete, consistent and accurate data is essential for performance management, as it provides DHHS with a good analytical baseline. Each of DHHS's funded programs is subject to different reporting obligations and time lines. For example, DHHS requires quarterly submission of CHP data for the CHMDS and annual submission for data on health promotional activities. DHHS regularly updates its reporting guidelines to reflect any changes to the CHMDS and allows community health services to resubmit any missing or corrected files twice yearly.
The health system's devolved governance model means that community health services deliver funded programs with minimal interference from DHHS. As a result, DHHS does not provide community health services with a universal client management system to input their various datasets. Instead, community health services collect their data using a range of different products, each with different capabilities. Certain funded programs, such as Dental Health, mandate the use of a particular client management system. This means that community health services generally operate multiple client management systems to support their various programs. The Primary Care Partnerships Service Coordination survey undertaken in 2015 reported that there were 15 client management systems in use across the sector.
This wide variety of client management systems—coupled with DHHS's different reporting obligations for each dataset—do not support community health services to provide integrated care. Behind the scenes, community health services must disaggregate the different components of their 'wrap around' service delivery model to fulfil DHHS's varied reporting requirements, which is a time-consuming and cumbersome process. As different client management systems support different funded programs, it is difficult for community health services to obtain a clear image of their client's journey through the system. For example, a client's dental health treatment plan is stored in a separate software application to his or her allied health appointments. This also leads to duplicated effort for practitioners, as they must input clients' profiles across multiple systems.
In 2017, DHHS commenced the Community Health Data Alignment Project to reduce the reporting burden on community health services. DHHS commissioned specialists to undertake a review of three major datasets—Community Health, Dental Health, and Alcohol and other Drug Treatment Services—and make recommendations. The review found that DHHS uses inconsistent terminology across its datasets, which contain a mixture of redundant, irrelevant and complex data elements. It also found that some of DHHS's existing validation rules—or data cleansing methods—are out of date or insufficient.
The review also flagged DHHS's minimal feedback as a key issue for the community health sector. DHHS mandates the collection of various data elements, but fails to translate the data into meaningful information. For community health services, this decreases the relevance of complete, consistent and accurate data entry. The review further notes that data entry errors at community health services may be the result of limited training, software limitations and resource constraints.
To address this, DHHS is considering the annual release of de-identified data to enable benchmarking among community health services.
Since late 2016–17, DHHS has made various changes to the CHMDS, as outlined in its most recent Community Health Program Data Submission Guidelines. This includes the removal of redundant data elements, the addition of vital concepts and language alignments. DHHS has also conducted multiple workshops with the sector to identify concerns and communicate any progress. Overall, DHHS's Community Health Data Alignment Project is a step in the right direction.
DHHS has accepted all of the review's recommendations, which demonstrates its commitment to reducing the reporting burden for community health services. The project is scheduled for completion in mid-2018–19 and includes a post-implementation review to assess its impact.
4.8 High-quality service delivery
In addition to its performance management system, DHHS has guidance and tools for community health services to encourage high-quality service delivery. DHHS defines high-quality care as safe, effective and person centred. This means that community health services must reduce the risk of avoidable harm, deliver timely, appropriate and integrated care, and encourage clients to voice their opinions throughout their clinical journey. Continuous quality improvement is also a foundational principle of the CHP and one of DHHS's key underlying policies.
We assessed whether DHHS's guidance to community health services aligns with best practice principles for high-quality service delivery—such as accreditation and consumer engagement—and fulfils the CHP's objective of providing effective healthcare to Victoria's priority populations.
Accreditation
DHHS expects community health services to meet basic minimum requirements for safe, effective and person-centred care. These requirements are formalised in accreditation cycles and DHHS's guidelines.
Accreditation is pivotal to DHHS's quality assurance framework. It involves an external body formally reviewing an agency's policies, procedures and practices. Accrediting bodies will generally conduct top-down evaluations of an agency's outcomes, workforce retention rates, infrastructure and clinical governance arrangements. Accreditation is a legislative requirement for both integrated and registered community health services.
Accreditation aims to optimise safety and mitigate risks for both community health services and the Victorian public. DHHS oversees the state's accreditation register and may intervene at community health services to address any issues. Community health services undergo accreditation assessments for both Commonwealth- and state-funded programs.
Community health services' accreditation
As community health services deliver a range of programs, they often require multiple accreditation awards. We heard anecdotally from community health services that the accreditation cycle is resource intensive and creates a widespread administrative burden. According to the audited community health services, each accreditor requires similar documentation in a slightly different format, which leads to duplicated effort from allied health practitioners, doctors, nurses and support staff. Community health services recognise the importance and value of accreditation, but note that it increases their already heavy workloads.
As an example, Figure 4G shows the various accreditations held by cohealth as at 2016–17.
Figure 4G
cohealth's current accreditation awards
|
Accreditation award |
Accredited areas |
Next due |
|---|---|---|
|
Quality Improvement Council |
|
July 2018 |
|
Royal Australian College of General Practitioners |
|
Various throughout 2018 |
|
National Safety and Quality Health Standards |
|
July 2018 |
|
DHHS's standards |
|
July 2018 |
|
Home Care Standards |
|
August 2020 |
Source: VAGO based on cohealth's Annual Report 2016–17.
In July 2018, cohealth will be reassessed for three of the above standards. This means that cohealth will be subject to multiple accreditation assessments within a relatively short time frame, which may reduce the time its clinical staff can spend with clients.
Community Health Streamlining Accreditation Project
In 2017, DHHS commenced the Community Health Streamlining Accreditation Project to identify options that reduce the regulatory load for community health services. It engaged consultants to produce a sector accreditation profile, which confirmed the burden experienced by community health services. The consultants identified that, on average, community health services hold accreditation against five mandatory standards. Accreditation burdens community health services through membership fees, onsite assessments, staff exertion and unnecessary duplication. The report recommended various changes, such as reducing repetition through greater coordination of standards, streamlining assessments at the Commonwealth level, and supporting service delivery models that improve health services' use of resources. Importantly, the report emphasised that DHHS should proactively engage with other stakeholders—such as the Commonwealth—to encourage system-wide change and innovation.
To address these issues, DHHS has committed to reviewing the duplication between its internal standards and other regulatory mechanisms, such as the FOPMF. It will also advocate to the Commonwealth and support community health services to strengthen their governance capabilities. DHHS has amended its 2017–18 Policy and funding guidelines to note that if a community health service is already accredited for governance and management under a recognised standard, it is not required to gain this accreditation again for its primary and community health funded services. This demonstrates DHHS's commitment to understanding and addressing the sector's concerns.
Service Coordination Practice Manual
DHHS's Service Coordination Practice Manual (the manual) helps community health services align their intake and assessment procedures with optimal practice principles, such as person-centred care. The manual aims to improve the client experience by ensuring the following:
- People should receive the right care regardless of their entry point into the system—this is known as the 'no wrong door' policy.
- Independent providers—such as community health services—should develop transparent and consistent care pathways that are clear and understandable to clients. This requires effective information sharing between agencies so that clients receive seamless and integrated care.
- Practitioners should conduct effective assessments that identify their clients' needs at the earliest instance. This reduces the chance of further clinical deterioration.
The manual also outlines DHHS's expectations for the key stages of service coordination—initial contact, initial needs assessment and care planning. It assigns responsible staff members to these stages and describes each stage in detail, including good practice indicators and ideal client outcomes. This gives community health services a standard to emulate. The manual provides the foundations for continuous quality improvement and high-quality care.
In 2013 and 2015, DHHS conducted a statewide survey to assess whether community health services comply with the manual's best practice principles for care planning, information sharing and use of the Service Coordination Tool Templates. The survey specifically assessed whether community health services complied with indicators from the Primary Care Partnership's Program Logic 2013–17 strategy, which align with the manual's key concepts.
Overall, the 2015 survey shows that some service coordination occurs, however, there is room for improvement. For example, of the state's 339 respondents across DHHS's eight regions, 62 per cent have developed a local agreement that supports shared care planning, while only 46 per cent have gone on to implement the plan. The survey provides DHHS with valuable information regarding the manual's use at community health services and encourages benchmarking across the divisions. However, there is no evidence that DHHS used the survey results to improve service delivery, or facilitated information-sharing forums to assist community health services to learn, innovate and adapt their approaches.
Beyond the survey, DHHS has minimal oversight of the manual's integration in community health services. The South division, however, uses its benchmarking report as an additional quality assurance mechanism. As shown in Figure 4H, the division's report enables it to pinpoint areas for improvement and remind community health services of their obligations to deliver high-quality care. DHHS's central office is aware of this report, however, it is unknown whether it will be implemented across the state.
Figure 4H
Traralgon office's (South division) benchmarking report
|
DHHS's Traralgon office uses a benchmarking report to assess community health services' local performance across a range of different parameters. Benchmarking is a popular performance management tool, as it encourages cross-agency learning, the identification of service delivery gaps, and the implementation of best practice. To create the report, DHHS's Traralgon office consolidates information from the CHMDS and produces a series of graphs. The graphs reflect the performance of eight local community health services across a three-year period and explore various funded activities, such as allied health, nursing, care coordination and INI. According to the Traralgon office, the report provides a supportive approach to continuous improvement, as it encourages self-reflection and collegial behaviour. The audited community health services value the report as a catalyst for internal and external discussions, however, some advised that they would benefit from more qualitative commentary, such as the sharing of local innovations. In addition to its benchmarking role, the report enables DHHS to reiterate the importance of key principles, such as integrated care and robust data collection. For example, of the eight community health services assessed, only four collect information regarding INI—despite all community health services reporting that INI is an essential element of their service delivery models. Through the benchmarking report, the Traralgon office emphasises the importance of INI's role in securing holistic, multidisciplinary care. This may encourage community health services to reassess DHHS's good practice indicators—as outlined in the Service Coordination Practice Manual—and collect the relevant INI data going forwards. Overall, the report represents good practice, as it promotes introspective analysis across the region. The Southern metropolitan area has recently adopted Traralgon's template and is receiving similar feedback. |
Source: VAGO.
Engaging with clients
Engaging with their clients demonstrates community health services' commitment to high quality, person-centred care, as it values the individual's needs and opinions. Effective client engagement may also reduce waste, lower costs and enhance clients' outcomes. DHHS engages with the clients of community health services through feedback tools, such as patient experience surveys. It also requires each community health service to publish an annual 'quality account' to increase their public accountability.
Victorian Healthcare Experience Survey—Community Health
DHHS extended its annual VHES to the community health sector in late 2016. The survey aims to enhance person‑centred care by engaging local communities in improving the delivery of health services. It supplements the limited insight provided by DHHS's existing performance measures, and increases community health services' accountability.
DHHS distributed 50 000 surveys across 85 agencies and achieved an overall response rate of 15.2 per cent. The survey was voluntary and anonymous, and targeted adult clients across a three-month window. It contained 66 questions— 63 were multiple choice and three were free text. At the end of the survey, DHHS published the state's results through a secure online portal and imposed a minimum response threshold to ensure statistical integrity. As a result, agencies with a response rate of less than 30 surveys were unable to view their individual results, as small samples convey limited insight.
The survey evaluated different aspects of service delivery, such as access, staff attitudes, the agency's built environment, and the effectiveness of care planning. While community health services often conduct their own consultative exercises, DHHS's survey promotes continuous quality improvement, as it provides a standardised platform for benchmarking and cross-agency learnings. DHHS translated the survey into various languages to maximise inclusion, and some community health services assisted their clients to complete the questionnaire on site.
While the survey supports DHHS's commitment to person-centred care, it has various issues. For example, the survey is lengthy and does not consider the literacy levels of Victoria's priority populations. In designing the survey, DHHS met with consumer representatives from both Manningham Community Health Service and Caulfield Community Health Service as part of a broader advisory group, however, both representatives did not attend all three developmental workshops. Sixteen clients across Melbourne and Bendigo later piloted the draft survey and this informed its revisions. Therefore, DHHS's engagement with consumer representatives was low. In contrast, New Zealand trialled its equivalent survey with 10 focus groups containing 88 people during the first stage of its testing process, and later conducted numerous face-to-face interviews with clients.
DHHS intends for community health services to publicise certain aspects of the survey's results in their upcoming quality accounts, however, due to the survey's low response rate, it is unknown whether it will accurately portray community health services' performance.
Detailed client engagement is pivotal, as it enables governments to produce effective tools that adequately meet the needs of their target audience. This is emphasised by Orbost Regional Health's Consumer Reference Group, which vets and approves the agency's external communication prior to its release. All publicly available documents receive the reference group's 'consumer tick of approval for readability', which represents better practice as it validates the agency's commitment to person-centred care.
Quality accounts
DHHS mandates the publication of quality accounts. Quality accounts emphasise transparency and enable community health services to publicise their commitment to safe, effective and person-centred care. They are produced annually and aim to provide stakeholders with clear and accessible information regarding an agency's performance, with a particular emphasis on processes and outcomes.
DHHS outlines mandatory standards for agencies through its Quality Account Reporting Guidelines. These guidelines stress the importance of 'listening to patients' and demonstrating 'continuous improvement'. According to DHHS, community health services must publicise their methods of seeking and responding to client feedback, list their accreditation status, describe a quality improvement process that targets the program's priority populations, and demonstrate their commitment to continuity of care.
In addition, public health services—such as hospitals—report against a range of measures, including the results of the acute sector's patient experience survey and the prevalence of healthcare-associated infections.
Quality accounts provide public health services with a platform to explain their performance, and outline their improvement. In contrast, community health services lack standardised performance measures that enable the public to objectively evaluate the services' progress on an annual basis, and assess their level of improvement. The information presented within quality accounts is largely at the community health services' discretion and is generally qualitative in nature.
While quality accounts supplement the information provided in BP3, the absence of specific performance measures means that the public can neither benchmark services, nor track their progress over the years.
Appendix A. Audit Act 1994 section 16—submissions and comments
We have consulted with DHHS, Bendigo Health, East Wimmera Health Service, Monash Health, Peninsula Health, Bendigo Community Health Service, cohealth, Gippsland Lakes Community Health, Latrobe Community Health Service, North Richmond Community Health and Orbost Regional Health, and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report to those agencies and asked for their submissions or comments. We also provided a copy of the report to the Department of Premier and Cabinet.
Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
- DHHS
- cohealth
RESPONSE provided by the Secretary, DHHS

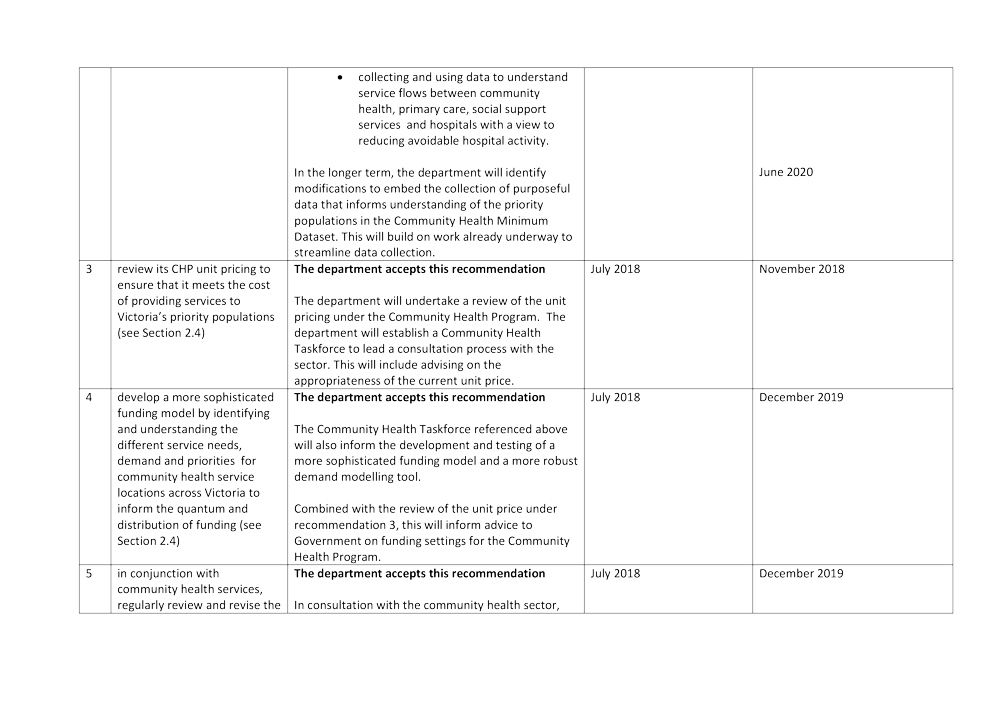
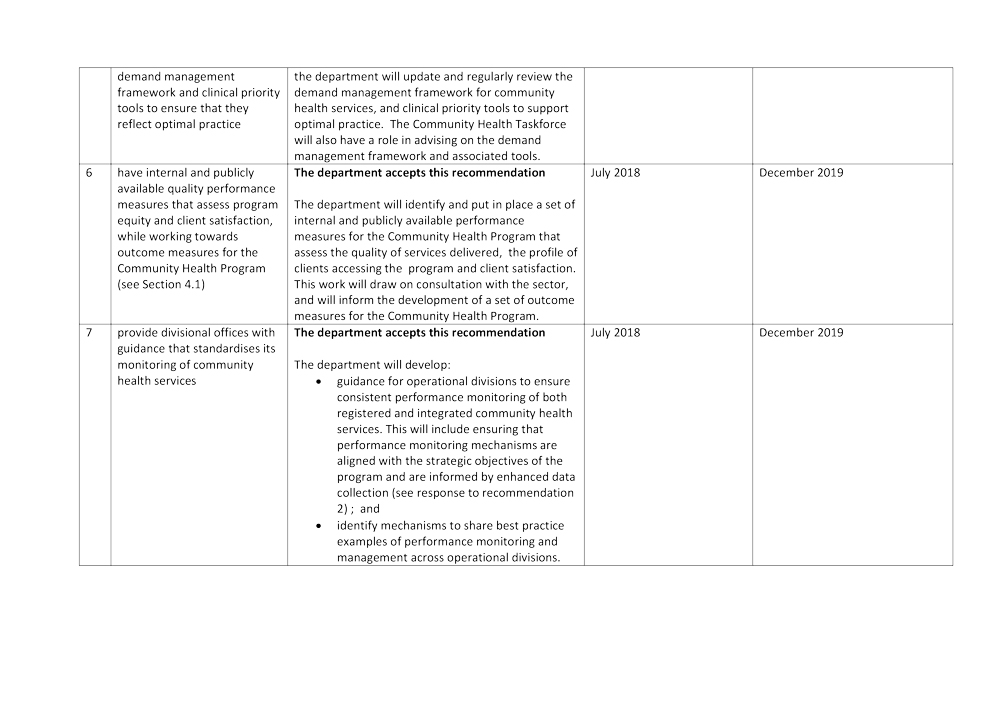
RESPONSE provided by the Chief Executive, cohealth