Heatwave Management: Reducing the Risk to Public Health
Overview
Heatwaves pose a significant risk to public health. Heat-related illness can range from mild conditions, such as a rash or cramps, through to heat exhaustion, and finally to potentially fatal conditions such as heat stroke. After the 2009 heatwave in Victoria, the Department of Health developed a heatwave framework to help reduce the impact on public health. While the framework and collective efforts of agencies contributed to a reduction in the severity of the impact of the 2014 heatwave, there are shortcomings that need to be addressed as a matter of urgency if Victoria is to be adequately prepared for, and able to respond appropriately to, a prolonged heatwave. Governance arrangements for heatwaves are not clear.
While Victoria Police is the identified control agency for the response to heatwaves, there is a lack of clear and effective leadership to provide a coordinated multi-agency approach to the state’s heatwave management. There is no mandatory requirement for agencies to have a heatwave plan. While each of the audited councils and health services had a plan, the effectiveness of the heatwave framework is compromised because it is being applied selectively by agencies. The quality of the plans, and the triggers for activation of the plans, are also variable.
Public health messages about the potentially significant health risks associated with extreme heat need to be disseminated more effectively to the broader community and not just targeted to the most vulnerable groups. Community members need to understand not only the nature of the potential risks to health but also how to manage these risks appropriately. "
Heatwave Management: Reducing the Risk to Public Health: Message
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report on the audit Heatwave Management: Reducing the Risk to Public Health.
The audit examined whether the Department of Health's heatwave framework has been effective in reducing the impact of extreme heat on public health. In particular, the audit assessed whether agencies are well prepared to respond to heatwaves and have effectively applied the heatwave framework.
While the framework has contributed to reducing the impact of extreme heat on public health, I found several shortcomings that need to be addressed if Victoria is to be adequately prepared for—and able to respond to—prolonged heatwaves. In particular, there needs to be greater clarity around the roles and responsibilities for the management of heatwaves and better public messaging. I have made eight recommendations which, if implemented, will strengthen Victoria's capacity to prepare for and respond to prolonged heatwaves.
Yours faithfully
John Doyle
Auditor-General
14 October 2014
Auditor-General's comments
 John Doyle John DoyleAuditor-General |
Audit team Michele Lonsdale—Engagement Leader Melinda Gambrell—Team Leader Aina Anisimova—Analyst Jason Cullen—Analyst Engagement Quality Control Reviewer Ray Winn |
Heatwaves have contributed to more deaths than any other natural disaster in Australia. In Victoria, the number of 'excess deaths' from the 2009 heatwave was much greater than the number of deaths arising from the Black Saturday bushfires the following week.
It is expected that the duration and severity of heatwaves will increase. Victoria's ageing population and the growing incidence of chronic disease, makes our community increasingly vulnerable to the impact of prolonged heatwaves. Despite this, the community continues to underestimate the impact of extreme heat on their health.
The audit examined whether the Department of Health's heatwave framework, which is consistent with international better practice, has been effective in reducing the impact of extreme heat on public health. I found that while implementation of the framework and the collective efforts of all agencies contributed to reducing the impact of extreme heat in the 2014 heatwave, there are several key shortcomings that need to be addressed.
There needs to be greater clarity around roles and responsibilities in the management of heatwaves. Currently governance arrangements are unclear—although Victoria Police is the identified control agency for the response to heatwaves, there is a lack of clear and effective leadership to provide a coordinated multi-agency approach to the state's management of heatwaves. The lack of clear understanding and definition of a heatwave has contributed to this.
While Victoria has a state-level emergency plan for tsunamis, it does not have a state-level plan for heatwaves, despite heatwaves being identified as one of the state's significant emergency management risks. Individual agency heatwave plans are not mandatory, their quality is variable, and there is lack of clarity around the triggers for activation of the plans. There is also inadequate assurance as to their quality.
While the Department of Health issued targeted messages to vulnerable groups in the community during the 2014 heatwave, better messaging and public education are needed to increase broader public understanding of the impact that extreme heat can have, and of the ways in which this impact can be managed. Assisting individuals to take more responsibility for the health and wellbeing of themselves and others in the community would help reduce pressure on emergency services, particularly Ambulance Victoria, during heatwaves.
There are insufficient assurance mechanisms in place to be confident that public health services are well prepared to manage the risk of critical infrastructure failure, such as air conditioning and emergency generators, during a heatwave. This is a serious risk given that hospitals care for the state's most vulnerable people, including those susceptible to extreme heat.
As we head into the 2014–15 summer season, these issues need to be addressed urgently and proactively if Victoria is to be better prepared to respond to heatwaves and adverse impacts on public health are to be minimised.
The report contains eight recommendations which, if implemented, will help improve the state's preparedness for and capacity to respond to heatwaves.
I intend to revisit the issues identified in this report to ensure they are being appropriately addressed.
I want to thank the staff in the Department of Health, Department of Human Services, Department of Justice, Ambulance Victoria, Victoria Police, the three audited health services and three audited councils who assisted with this audit and for their constructive engagement with the audit team throughout the audit.
John Doyle
Auditor-General
October 2014
Audit summary
Heatwaves pose a significant risk to public health. Heat-related illness can range from mild conditions, such as a rash or cramps, through to heat exhaustion, and finally to potentially fatal conditions such as heat stroke.
In the past five years, Victoria has endured two heatwaves that have contributed to significant loss of life. The Department of Health (the department) has estimated that during the 2009 heatwave there were 374 excess deaths—this is more than the number of deaths attributed to the Black Saturday bushfires the following week. A further 167 excess deaths occurred during the 2014 heatwave.
The Bureau of Meteorology states that the duration, frequency and intensity of heatwaves in Australia have increased since 1950. Heatwaves have become more prevalent in the past 20 years across the south-eastern states of Australia.
Heatwaves are expected to become more frequent in Victoria. Based on current trends, the Victorian Government's 2014 Emergency Risks in Victoria – Report of the 2012–13 State Emergency Risk Assessment estimated that the average annual number of days above 35ºC in Melbourne is likely to increase from nine days in 2014 to 11–13 days in 2030 and 15–26 days by 2070.
Since the 2009 heatwave, the department has developed a heatwave framework to reduce the impact of extreme heat on public health. The framework includes the Heatwave Plan for Victoria, the Heatwave Planning Guide for municipal councils, the Heat Health Alert System, the Heat Health Information Surveillance System and communication resources.
The objective of this audit was to determine whether applying the department's heatwave framework has been effective in reducing the impact of extreme heat on public health.
Conclusions
While there was a reduction in the estimated number of excess deaths associated with the impact of extreme heat on health during the 2014 heatwave, the department is not able to clearly attribute this outcome to the implementation of its framework. However, in 2009 there was no heatwave framework in place. It is likely that the framework and collective efforts of all agencies have contributed to the reduced impact on public health in 2014.
The heatwave framework is soundly based. It includes many of the elements accepted by leading international health and meteorological organisations as being essential to respond to the potentially significant health risks associated with heatwaves.
However, there are a number of critical gaps that were identified in the 2009 heatwave debrief that continue to be raised as issues—such as the need for clear roles and responsibilities, sufficient strategic monitoring, greater clarity around triggers for activation and sharing of data across multiple systems.
The Heatwave Plan for Victoria is not a state-level plan. While Victoria has a State Tsunami Emergency Plan and a State Earthquake Emergency Plan, there is no equivalent state-level plan for heatwaves, despite the recognised significant risk heatwaves present to the state and to the community.
Governance arrangements for heatwaves are not clear despite this being raised as an issue in the 2009 heatwave debrief. There is a lack of clarity over who is leading the response to heatwaves. While Victoria Police is the assigned control agency, it is not always recognised by others as the leader of heatwave emergency response and in 2014 did not assume or consistently apply its assigned responsibility across regions.
This means that no agency is making sure all support agencies have activated their heatwave plans or that resources are being directed to where they are needed most, or monitoring the effectiveness of those arrangements. As a consequence, the state's response to heatwaves is being managed at an operational rather than a strategic level.
There is no mandatory requirement for agencies to have a heatwave plan. Victoria Police, as the control agency for the response to heatwaves, is still finalising its operational guidelines for heatwaves with the intention of releasing these in time for the 2014–15 fire danger period. While each of the councils and health services we audited had a plan, the effectiveness of the heatwave framework is compromised because it is being applied selectively by agencies. There are significant gaps in quality control and quality assurance over state and local emergency management planning.
While there was a noticeable increase in the amount of public health messaging in the 2014 heatwave, messages about the potentially significant health risks associated with extreme heat, and the ways in which community members can prepare for and respond to heatwaves, are not being disseminated effectively to the broader population. This means community members are not being adequately prepared for heatwaves.
Findings
Governance arrangements are not clear
Roles and responsibilities for responding to and managing heatwave incidents are not clear or well understood by agencies. Victoria Police's role as control agency for the response to heatwaves was intended to be an interim arrangement, however, this arrangement has not been reviewed. There is currently a lack of clear and effective leadership to provide an integrated, multi-agency approach to the state's management of heatwaves.
Monitoring and reporting arrangements are not adequate given the significant risks associated with a heatwave emergency. For example, State Control Centre daily briefs show that most of the information reported as the 2014 heatwave progressed was on preparedness for the consequential impact of fire. There was no equivalent mapping or analysis of the extreme heat impacts across the community.
While all audited agencies had incident management systems, these did not fully capture key decisions made during the event.
Quality of planning for heatwaves is variable
There is no mandatory requirement for agencies to have a heatwave plan and there are no clearly articulated minimum requirements to guide development of state-level plans. The Heatwave Plan for Victoria is an operational plan, not a recognised state-level incident plan for heatwaves. Despite being the control agency for the response to heatwaves, Victoria Police is still finalising its operational guidelines in time for the 2014–15 fire danger period. While municipal councils may develop heatwave plans as sub-plans of their municipal emergency management plan, the currency and quality of these plans is not monitored or reviewed.
Sufficient and appropriate resources are not always available across all agencies to respond to heatwaves. Reduced staffing over the summer months affected some agencies' ability to respond effectively during both the 2009 and 2014 heatwaves. While health services were able to manage demand, the audited councils needed to recall staff from holidays to make contact with vulnerable people. During the 2014 heatwave, the Emergency Services Telecommunications Authority—the Triple Zero emergency call-taker—responded to the highest number of calls for ambulance services ever recorded. However, Ambulance Victoria needed to bring in additional resources to respond to demand.
Health services care for some of the state's most vulnerable people, who are particularly susceptible to extreme heat. For health services, a significant risk during a heatwave is failure of critical infrastructure and the performance of emergency generators. Recognising this risk, the department provides $25 million annually as part of the Engineering Infrastructure Program. However, there is no assurance that health services are prepared for the risk of critical infrastructure failure.
While training and emergency incident exercises are regularly provided, extreme heat and its impact on resources, infrastructure and the community, has not yet been adequately tested in the form of an emergency exercise. A more proactive approach to heatwave preparedness is needed which includes a prolonged heatwave scenario.
Public health messages are not always well targeted
The Heat Health Alert System (HHAS) is soundly based and accords with best practice internationally. However, the HHAS objective of notifying stakeholders of forecast heatwave conditions that are likely to have an impact on public health is not consistently and effectively achieved.
Public health messages do not fully meet community needs. For example, heat health alerts are not well understood and do not target the whole community. Although there was increased media focus on heatwaves in 2014, they do not receive the same level of media attention as other extreme weather events in relation to the impact on health and ways of minimising this impact.
While heat health messages are targeted at the most vulnerable, they need to be underpinned by education and awareness-raising activities to encourage community members to take responsibility for each other in order to reduce reliance on government or agency intervention.
Audited agencies found the department's communications resources suitable, although they acknowledged they could improve how well they distribute the department's information in the community.
Heatwave plans activation is not well understood
During the 2014 heatwave, the department monitored the activation of heatwave plans by health services and councils, establishing whether health services had an alternative power source and had checked its operation. While these measures are appropriate to the risk, they are not usual practice or reflected in the department's plan.
Activation is not well understood by agencies and is applied inconsistently. The department's HHAS does not follow the Victorian Warning Protocol to issue warnings in a phased approach. Activation of heatwave plans in municipal councils can mean anything from sending out a summer newsletter or forwarding a heat health alert, to establishing an incident control centre.
A department survey of councils in late January 2014 during a second spike in extreme heat—after the mid-January heatwave—identified inconsistent application of basic elements of sound heatwave management, as well as examples of good practice. However, there is no systematic dissemination of this good practice to inform future planning and drive improvement.
Recommendations
That Emergency Management Victoria:
- working with appropriate agencies, clarifies the control and other roles and responsibilities for heatwave arrangements
- facilitates the development and implementation of coordinated whole‑of-government heatwave arrangements
- facilitates the development of guidelines, including appropriate minimum standards for content in state-level sub-plans of the State Emergency Response Plan
- in developing the new emergency management planning legislation, clarifies the role of municipal councils and includes a quality assurance mechanism for municipal emergency management planning.
That the Department of Health:
- assures itself that public health services are well prepared to manage the risk of critical infrastructure failure during a heatwave
- develops a communication strategy for heatwaves that includes public awareness and education activities
- implements a phased approach to heat health alert warning categories in line with the Victorian Warning Protocol
- reviews the purpose and effectiveness of the Heat Health Information Surveillance System during a heatwave.
Submissions and comments received
In addition to progressive engagement during the course of the audit, in accordance with section 16(3) of the Audit Act 1994 a copy of this report, or relevant extracts from the report, was provided to the Department of Health, the Department of Human Services, the Department of Justice—which includes Emergency Management Victoria—Ambulance Victoria, Victoria Police and the three audited councils and three audited health services with a request for submissions or comments.
Agency views have been considered in reaching our audit conclusions and are represented to the extent relevant and warranted in preparing this report. Their full section 16(3) submissions and comments are included in Appendix A.
1 Background
1.1 Introduction
Heatwaves represent a significant risk to public health. In Victoria, the number of 'excess deaths' from the 2009 heatwave was much greater than the number of deaths arising from the Black Saturday bushfires the following week. Not only is the risk significant, but the likelihood and duration of heatwaves is expected to increase, while an ageing population with greater levels of chronic disease will make Victorians more vulnerable to the impact of these events.
Despite the gravity of this scenario, the potentially devastating impact of extreme heat on individuals and services is frequently underestimated by the community.
1.1.1 Impact of heatwaves
Heat-related illness occurs when the body is unable to adequately cool itself, ranging from mild conditions such as a rash or cramps, through to heat exhaustion, and finally to very serious and potentially fatal conditions such as heat stroke. Extreme heat events can also exacerbate pre-existing conditions, with the risk of heat-related mortality (death) and morbidity (disease, illness) increasing for people with illnesses—including cardiovascular disease, diabetes and cancer. The aged, infirm and isolated, young children, nursing mothers, and people on certain medications are all vulnerable. An additional area of concern is occupational heat stroke, particularly for outdoor workers and indoor workers with limited access to cooling systems.
In the past five years, Victoria has endured two heatwaves that have resulted in significant loss of life. Figure 1A shows that there were three days of extreme heat—mean above 30ºC temperatures—in Melbourne at the end of January 2009 and four days in mid-January 2014.
Figure 1A
Daily temperatures during extreme heat events in Melbourne, 2009 and 2014
|
2009 |
Max |
Min |
Mean |
2014 |
Max |
Min |
Mean |
|---|---|---|---|---|---|---|---|
|
26 Jan |
25.5 |
14.4 |
21.1 |
12 Jan |
22.8 |
16.5 |
19.0 |
|
27 Jan |
36.4 |
16.6 |
27.6 |
13 Jan |
31.1 |
15.2 |
24.7 |
|
28 Jan |
43.4 |
18.8 |
34.6 |
14 Jan |
42.8 |
18.2 |
35.7 |
|
29 Jan |
44.3 |
25.7 |
35.0 |
15 Jan |
41.7 |
28.6 |
34.4 |
|
30 Jan |
45.1 |
25.7 |
33.8 |
16 Jan |
43.9 |
27.0 |
34.8 |
|
31 Jan |
30.5 |
22.5 |
25.4 |
17 Jan |
43.9 |
25.6 |
32.7 |
|
1 Feb |
33.8 |
20.3 |
27.3 |
18 Jan |
24.0 |
21.4 |
20.1 |
Source: Victorian Auditor General's Office, using Bureau of Meteorology Melbourne regional office weather station data.
January 2009 heatwave
In 2009, the heatwave was of unprecedented intensity and duration with maximum temperatures 12–15ºCelsius (ºC) above normal for much of Victoria, while Melbourne endured three consecutive days of temperatures above 43ºC. There were 374 excess deaths during the heatwave—a 62 per cent increase in mortality compared to what is normally expected at that time of the year. The greatest number of excess deaths occurred in those 75 years or older, while deaths in those 65 years and older more than doubled compared with the same period in 2008.
January 2014 heatwave
In 2014, Melbourne experienced temperatures in excess of 41ºC each day between 14 and 17 January inclusive. Parts of the state experienced temperatures of 45ºC or more on three consecutive days during this period.
In 2014, there were 167 excess deaths during the heatwave. This heatwave was similar in intensity and duration to the 2009 heatwave. Although the maximum temperatures for the 2014 heatwave were slightly lower than those in 2009, the mean temperatures in January 2014 were higher and lasted longer than the temperatures experienced in 2009.
Comparison between the two heatwaves
In 2009, a heatwave was not yet formally recognised as an emergency in Victoria and there was no heatwave framework in place. Data available through the Heat Health Information Surveillance System shows a significant reduction in 'excess deaths' between the 2009 and 2014 heatwaves. Health services, the After Hours doctor service and the Coroner all experienced spikes on the day after the final day of the heatwave in both 2009 and 2014.
Figure 1B shows some of the impacts on public health and services during the two heatwaves.
Figure 1B
Impact on public health and services — 2009 and 2014 heatwaves
|
Nature of impact |
2009 (26 January |
2014 |
|---|---|---|
|
Excess deaths(a) |
374 |
167 |
|
Heat-related emergency department presentations |
714 |
621 |
|
After Hours doctor consultations |
1 955 |
3 687 |
|
Ambulance dispatches (metropolitan Melbourne) |
7 035 |
8 359 |
(a) Excess deaths are the number of deaths over what would normally be expected for the same period.
Source: Victorian Auditor-General's Office, using Department of Health information.
Figure 1C shows some additional evidence of the severity of the impact on public health and services during the 2014 heatwave.
Figure 1C
Further 2014 heatwave impacts
|
On 17 January 2014:
Between 12–18 January 2014:
|
Source: Victorian Auditor-General's Office, using Department of Health information.
Dehydration was the most common heat related condition at public hospital emergency departments during both heatwaves, followed by heat stroke and heat syncope—fainting due to extreme heat. Figure 1D shows the heat related emergency department presentations by patient condition.
Figure 1D
Heat-related emergency department presentations, by condition
Source: Victorian Auditor-General's Office, using Department of Health information.
The 2014 heatwave created a new record in the highest number of calls for ambulance services ever received in a day. On Thursday 16 January a new record was set, which was eclipsed the following day, Friday 17 January.
One of the most serious consequences from heatwave conditions is cardiac arrest. Ambulance Victoria responds to these incidents as a Priority 0 callout.
During the 2014 heatwave, there was an average of 49 Priority 0 callouts per day for metropolitan Melbourne, and during the 2009 heatwave there was an average of 25 Priority 0 callouts per day for metropolitan Melbourne.
1.2 What is a heatwave?
There is no single accepted definition for a heatwave because similar temperatures can have different impacts on communities at different times.
The Heatwave Plan for Victoria – Protecting health and reducing harm from heatwaves, defines a heatwave as 'a period of abnormally and uncomfortably hot weather that could impact on human health, community infrastructure and services'.
In 2013–14, as part of a heatwave forecast product trial, the Bureau of Meteorology developed a national definition of a heatwave—'three days or more of high maximum and minimum temperatures that is unusual for that location'.
Using findings from research undertaken by Monash University, the Department of Health (the department) has applied a technical definition of heatwave based on the minimum temperature threshold that is likely to impact on the health of a community and at which heat-related service activity increases. This is known as the heat health temperature threshold. At the threshold level, there is an increased risk of morbidity and mortality from heatwave conditions.
The department uses the Heat Health Alert System to monitor temperature using Bureau of Meteorology forecast information. This system was developed to notify agencies—such as local government, departmental units, hospitals and community service providers—of forecast temperatures likely to have an impact on public health.
1.2.1 The heat health temperature threshold
Three heat health temperature thresholds apply in Victoria, ranging from 30ºC in the south of the state, 32ºC across the centre of the state, to 34ºC in the north-west of the state. This is based on the research by Monash University that was used to develop the heat health threshold temperatures and reflects the varying levels of resilience to extreme heat across the state. For example, residents of Mildura in the north-west of the state have a higher level of resilience to extreme heat than residents in Geelong, therefore, the heat health temperature threshold for Mildura is 34ºC, whereas Geelong has a threshold of 30ºC.
The heat health threshold temperature is based on the average, or mean, temperature using the forecast day maximum and the forecast overnight temperature for the following day. For example, if Melbourne was forecast to have a maximum day temperature of 40ºC, the forecast overnight temperature would need to be 20ºC to trigger the heat health temperature threshold of 30ºC. If Mildura was forecast to have a maximum day temperature of 40ºC, the forecast overnight temperature would need to be 28ºC to trigger the heat health temperature threshold of 34ºC. Figure 1E shows the heat health temperature thresholds and corresponding weather forecast districts.
Figure 1E
Heat health temperature threshold and weather forecast districts
Source: Victorian Auditor-General's Office from the Department of Health's Heatwave Plan for Victoria – Protecting health and reducing harm from heatwaves, 2011
1.3 The heatwave framework
At the time of the 2009 heatwave, there was no heatwave framework in place.
In 2006, the government recognised that community and local government are the most appropriate levels for heatwave emergency planning and responses, and committed to the development of a Victorian heatwave emergency plan. As a result, the Department of Human Services developed the 2007 Victorian Heatwave Strategy, which provided the foundation for the subsequent 2009–10 heatwave framework.
The heatwave framework aims to reduce the impact of extreme health on public health and comprises the:
- Heatwave Plan for Victoria– Protecting health and reducing harm from heatwaves (2011)—to coordinate an integrated response to heatwaves
- Heatwave Planning Guide– Development of heatwave plans in local councils in Victoria (2009)—to assist municipal council heatwave planning
- Heat Health Alert System—to monitor climate conditions and alert stakeholders when the heat health threshold temperature is forecast to be met or exceeded
- Heat Health Information Surveillance System—to monitor and assess the human health impact of heatwaves
- communication resources—includes posters, brochures and information sheets.
1.4 Victoria's emergency management arrangements
Two significant external reviews of Victoria's emergency management arrangements in the past five years—the Victorian Bushfire Royal Commission and the Victorian Flood Review—have informed subsequent reforms to emergency management structures and arrangements.
In 2011, the Victorian Government released a Green Paper, Towards a More Disaster Resilient and Safer Victoria, which challenged Victoria's existing approach to crisis and emergency management arrangements. In 2012, a White Paper, Victorian Emergency Management Reform, paved the way for changes to the legislative framework governing emergency management. These developments are likely to result in further changes as the new legislation and associated governance arrangements are embedded.
1.4.1 Governance arrangements
The new Emergency Management Act 2013 came into effect on 1 July 2014 and, in conjunction with the earlier Emergency Management Act 1986, provides the legislative framework for the organisation of emergency management in Victoria. The objectives of the new legislation are to foster a sustainable and efficient emergency management system, establish efficient governance arrangements, and implement an 'all hazards—all agencies' approach based on networked arrangements and greater interoperability.
The new Act focuses on community, collaboration and capability. It establishes the:
- State Crisis and Resilience Council—the peak crisis and emergency management advisory body in Victoria
- Emergency Management Victoria (EMV)—the agency responsible for coordinating the development of whole-of-government policy for emergency management and implementing emergency management reform initiatives.
Emergency management governance arrangements are shown in Figure 1F.
Figure 1F
Source: Victorian Auditor-General's Office.
The new legislation supports the appointment of the:
- Chief Executive of Emergency Management Victoria—to provide advice and make recommendations on any issues relating to the functions of EMV, and to take a lead role in coordinating investment planning and large scale strategic projects on behalf of responding agencies.
- Emergency Management Commissioner—to coordinate the activities of responding agencies, ensure control arrangements are in place during an emergency and for consequence management for a major emergency.
- Inspector-General for Emergency Management—to provide assurance to government and the community on emergency management arrangements and to foster continuous improvement of emergency management in Victoria.
1.4.2 Planning arrangements
The Emergency Management Manual Victoria (EMMV) contains the policy and planning documents for emergency management. It includes emergency risk management and mitigation, the State Emergency Response Plan (SERP), municipal emergency planning arrangements and emergency management agency roles.
Figure 1G shows the relevant planning outputs from the 1986 and 2013 legislation, which are discussed below.
Figure 1G
Legislative framework – emergency management planning
Source: Victorian Auditor-General's Office.
State Emergency Response Plan
SERP identifies the organisational arrangements for managing the response to emergencies within—or with the potential to affect—Victoria. It identifies three key emergency management tasks of control, command and coordination:
- control is the overall direction of response activities in an emergency
- command is the direction of personnel and resources of an agency in the performance of that organisation's role and tasks
- coordination is the bringing together of agencies and resources to ensure effective response to and recovery from emergencies.
Municipal emergency management plans
The responsibilities of municipal councils are outlined in the Emergency Management Act 1986. Part six of EMMV operationalises these responsibilities, which include the requirement for councils to prepare and maintain a municipal emergency management plan (MEMP), to appoint a planning committee, and for the plan to be audited every three years by the Victoria State Emergency Service. Through the MEMP process, councils are required to identify key emergency risks—such as flood, pandemic and heatwave—and where appropriate, to develop sub-plans to specifically address these risks.
As part of the Victorian Heatwave Strategy 2007, the Department of Human Services funded a pilot project in 2008 to develop municipal council heatwave plans. The pilot informed the development of the Heatwave Planning Guide – Development of heatwave plans in local councils in Victoria, which was released in July 2009, several months after the 2009 heatwave.
Councils are also required under the Public Health and Wellbeing Act 2008 to develop municipal public health plans. Councils may develop municipal heatwave plans as a sub-plan to their MEMP, or as part of a municipal public health and wellbeing plan or in their municipal council strategic plan.
State Health Emergency Response Plan
The State Health Emergency Response Plan (SHERP) is the Victorian health response plan for emergency incidents and is a sub-plan of the SERP. The SHERP outlines the arrangements for coordinating the health response to emergency incidents that go beyond day-to-day business arrangements. It is an 'all-hazards', scalable plan and includes arrangements for regional and state health responses. It provides the framework for planning the health response to emergency incidents such as heatwave.
1.4.3 Roles and responsibilities
Part seven of the EMMV specifies agencies' roles in planning for, responding to, and recovering from an emergency. It specifies that Victoria Police is the control agency for the response to heatwave, and that other agencies, including the Department of Health, have a support role. A control agency leads the response to a particular type of emergency. Support agencies provide resources, such as personnel, essential services and materials, to support or assist a control agency or affected person.
Figure 1H shows the control and support agencies for the response to heatwaves.
Figure 1H
Agencies with a role in responding to heatwaves
Source: Victorian Auditor-General's Office.
1.5 Audit objectives and scope
The objective of this audit was to determine whether applying the Department of Health's heatwave framework has been effective in reducing the impact of extreme heat on public health.
To test this, the audit team examined whether:
- agencies have plans in place that are evidence-based and meet requirements
- governance arrangements are effective
- resources are fit for purpose and effectively deployed
- public health messages are appropriate and targeted
- activation of heatwave plans is monitored and reported
- the impact of extreme heat on public health has improved since 2009.
The Department of Health's central and regional offices, Ambulance Victoria, the Health and Human Services Emergency Management Branch within the Department of Human Services, Victoria Police, the Department of Justice—which includes Emergency Management Victoria—and a selection of public health services and municipal councils were included in the audit.
The Department of Environment and Primary Industries, Department of Transport, Planning and Local Infrastructure, and the Department of State Development, Business and Innovation were excluded from the scope as their roles relate largely to responding to infrastructure performance during a heatwave. Victoria's critical infrastructure resilience has been independently reviewed in 2013 (Evans Review) with a new strategy currently being developed.
1.6 Audit method and cost
The audit methodology included:
- reviewing relevant documents, such as:
- • heatwave emergency management plans, policies, standards and procedures
- • governance arrangements
- • debriefs, reviews and evaluations
- • staff training and development
- • heatwave communications
- analysing relevant data—including ambulance callouts and hospital presentations
- viewing key systems, such as the Heat Health Alert System and Heat Health Information Surveillance System
- interviewing key emergency management personnel in the Department of Health and Department of Human Services central and regional offices, Ambulance Victoria, Victoria Police, and in three selected health services and three councils in locations at high risk of adverse outcomes from the impact of extreme heat
- visiting the Health and Human Services State Emergency Management Centre, Ambulance Emergency Operations Centre, municipal councils and public health services, including public health services with residential aged care services
- assessing agencies' response to the 2009 and 2014 heatwaves
- consulting with other key stakeholders as identified through the audit.
The audit was conducted in accordance with section 15 of the Audit Act 1994 and Australian Auditing and Assurance Standards.
Pursuant to section 20(3) of the Audit Act 1994, any persons named in this report are not the subject of adverse comment or opinion.
The total cost of the audit was $340 000.
1.7 Structure of the report
The report is structured as follows:
- Part 2 examines the governance arrangements for heatwaves
- Part 3 examines how agencies plan for heatwaves
- Part 4 examines the response and activation of heatwave plans by agencies.
2 Governance arrangements
At a glance
Background
Governance is defined as the combination of processes and structures implemented by the governing body to inform, direct, manage, and monitor the activities of the agency towards the achievement of its objectives. Monitoring and reporting are key elements of good governance and provide opportunities for continuous improvement.
Conclusion
Governance arrangements for heatwaves are not clear, despite this being raised as an issue in both the 2009 and 2014 heatwave debriefs. Although there has been improvement since 2009, there is an ongoing lack of clarity in the sector regarding who is responsible for heatwave management, and a lack of recognition regarding the potential severity of the impact of heatwaves and the risks that they create for the community and to service delivery. The state response to heatwaves is being overseen at a functional level rather than a strategic level.
Findings
- Victoria Police's role as control agency for the response to heatwaves was only intended to be an interim arrangement.
- Not all issues identified in the 2009 heatwave debrief have been addressed.
- The 2014 heatwave debrief did not include all agencies with a recognised role in a heatwave emergency.
Recommendation
That Emergency Management Victoria, working with appropriate agencies, clarifies the control and other roles and responsibilities for heatwaves.
2.1 Introduction
The importance of effective emergency management governance arrangements cannot be overstated. The Victorian Bushfire Royal Commission's final report stated that, 'On 7 February 2009 state-level emergency management arrangements faltered as a result of confusion about responsibilities and accountability.'
A key objective of the Emergency Management Act 2013 is to establish efficient governance arrangements that clarify the roles and responsibilities of agencies, facilitate cooperation between agencies, and ensure the coordination of emergency management reform within the emergency management sector.
To assess the effectiveness of governance arrangements for heatwaves the audit examined whether:
- roles and responsibilities were clearly defined and understood
- appropriate monitoring and reporting arrangements were in place.
2.2 Conclusion
Governance arrangements for heatwaves are not clear, despite this being raised as an issue in both the 2009 and 2014 heatwave debriefs. While heatwaves are estimated to have contributed to more deaths than any other natural disaster nationally, there are no clear arrangements in place in Victoria to prepare for and drive the response to heatwaves.
There is lack of clarity in the sector about who is responsible for heatwave management. The impact of heatwaves and the risk they present to the community and service delivery are not well understood. Although there have been improvements in governance since 2009, the state response to heatwaves is being overseen at a functional rather than a strategic level. This makes it difficult for the state to provide a coordinated response to prolonged heatwaves.
2.3 Roles and responsibilities
Roles and responsibilities for heatwave incidents are neither clear nor well understood. Currently, Victoria Police is listed in the Emergency Management Manual Victoria (EMMV) as the control agency for managing the response to heatwaves. However this was an interim arrangement after the 2009 heatwave and has not been reviewed since. Preparing and responding to heatwaves is not being managed in an integrated manner and there is no clear leadership to anchor this process. The lack of clear understanding and definition of a heatwave has contributed to the lack of clarity around heatwave management in Victoria. The recent creation of the Emergency Management Commissioner is likely to lead to greater role clarity and a more integrated response.
2.3.1 Are roles and responsibilities clearly defined?
The EMMV identifies control and support agency roles. Support agency roles are split between community, public health, infrastructure and animal welfare—reflecting the impact of extreme heat on the community, public health, animals, and the operation of the state's electricity and transport infrastructure. The impact on public health is exacerbated when infrastructure fails.
Until recently, a heatwave was not a recognised emergency in the EMMV. The decision to allocate the control role to Victoria Police, which was made at a State Emergency Response Planning Committee meeting in October 2009, was an interim arrangement. Under the emergency management arrangements, Victoria Police assume the control role when there is no clear agency to be allocated control of the incident. The interim arrangement for heatwaves has not been reviewed.
Victoria Police has advised that it does not assume control of a the reponse to a heatwave until there is a period of three continuous days where a heat health alert has been issued. This is when Victoria Police determines that there is a heatwave, which becomes an emergency, triggering the state arrangements. It did not assume active state-level control of the heatwave response in 2014 even though the period of extreme heat exceeded three days.
The case study in Figure 2A is an example of how agencies can work together to meet the needs of their communities during a heatwave. In this example, Victoria Police was active early in the 2014 heatwave in response to infrastructure failure and the consequential impact of this on the rural community.
Figure 2A Case study – Integrated response to heatwaves
|
On 9 January 2014, the Chief Health Officer alerted the North East Weather District of forecast heatwave conditions for Tuesday 14 January. On January 13, a further alert was issued for 15 and 16 January. On 14 January, one of the major energy providers had scheduled maintenance in a location within this weather forecast district. Victoria Police became concerned about the significant impact the power outage was having on the community and liaised with the energy provider to restore power. Victoria Police at the local level worked with key agencies in response to the risk. Representatives from the Department of Human Services and the rural city council door-knocked in the affected area to provide residents with bottled water, and a relief centre was established in the local hotel. Victoria Police contacted the local media to let people know where water and relief were available and who to contact if they required water for livestock. Victoria Police checked on residents listed on the Vulnerable People's Register and the council contacted clients receiving Home and Community Care services. Power was restored to the community. |
Source: Victorian Auditor-General's Office based on information provided by and audited agency.
This case study highlights some of the issues with the current arrangements. While the Department of Health is best placed to respond to a public health emergency, Victoria Police has a played a lead role in directing the response to the consequences of heatwaves. Under the new legislation, the Emergency Management Commissioner has responsibility for consequence management—to minimise the adverse consequences to users of services or infrastructure when an interruption occurs as a consequence of a major emergency.
2.3.2 Are roles and responsibilities understood?
Not all audited agencies recognise that Victoria Police is the control agency for the response to heatwaves and reported receiving little or no direction from Victoria Police during the 2014 heatwave. If direction was provided, it was because of an associated threat of fire.
Figure 2B shows the different agencies in other Australian jurisdictions that have been allocated responsibility to control the response to heatwaves under state emergency management arrangements.
Figure 2B
Control agency for heatwaves – Australian jurisdictions
|
Victoria |
South Australia |
Western Australia |
New South Wales |
Queensland |
|---|---|---|---|---|
|
Victoria Police |
State Emergency Service |
Department of Health |
Commissioner of Police |
Queensland Health |
Source: Victorian Auditor General's Office.
In its 2009 heatwave debrief, the Department of Health raised the issue that the EMMV does not include responsibility for control during a heatwave—despite the likelihood of increased heatwaves. In its 2014 debrief of the effectiveness of its State Health Emergency Response Plan (SHERP) in response to the heatwave, the department identified that closer liaison with Victoria Police on heat health, and not simply infrastructure, was needed. The department also noted that the control and command roles were not clear.
Interviews with the Department of Health, Department of Human Services, Victoria Police and Ambulance Victoria all supported the need to clarify who is the control agency for heatwaves so that responsibilities are understood.
Given the likelihood of more frequent and prolonged heatwaves, the objectives of the new legislation, and the findings from the Victorian Bushfire Royal Commission, the lack of clarity regarding roles and responsibilities for heatwave needs to be addressed as a matter of priority.
2.4 Monitoring and reporting arrangements
Given the multiple consequential risks associated with periods of extreme heat, the current monitoring and reporting arrangements are not appropriate.
While state-level governance structures were in place throughout the 2014 heatwave—including the State Emergency Management Team—the main focus was more on preparing for the consequential risk of fire than for heatwaves and its impact on resources.
Under Victoria's emergency management arrangements, Victoria Police—as the incident controller for heatwaves—is responsible for strategic management of the incident. Responsibilities include:
- managing all response activities
- notifying support agencies
- establishing incident and emergency management teams
- collecting, analysing and disseminating information regarding the emergency
- leading multi-agency response planning
- issuing timely information and warnings to the community
- developing incident action plans.
The audit did not find evidence of Victoria Police strategically managing or assuming responsibility for the 2014 heatwave incident at the state level. For example, while the State Emergency Management Team held daily meetings in the State Control Centre, these meetings were more informative than strategic, with situation reports from each agency. There was no evidence of strategic consideration of the consequences of this information. The post season review conducted by Emergency Management Victoria supports this observation.
Ambulance Victoria and the Department of Health developed incident action plans during the heatwave. As support agencies, their plans show functional level support but the plans did not provide an integrated 'all agencies' response to heatwaves. While there was evidence of heatwave management activity by Victoria Police at the regional level, this was isolated and not monitored in a strategic way. For example, the Hume region had an active champion leading the response in that region.
Figure 2C shows the basic governance structure implemented by the Department of Health for the majority of the heatwave period in their State Emergency Management Centre.
Figure 2C
Department of Health heatwave response structure
Source: Victorian Auditor-General's office based on Health and Human Services Emergency Management information.
The State Health Incident Management Team structure was implemented for the response to heatwave from Tuesday 14 January 2014, when the centre was activated, until Saturday 18 January when the health incident arrangements were stood down.
2.4.1 Monitoring arrangements
State Emergency Management Team meetings were held throughout the heatwave and appropriately monitored identified risks, including:
- the issuing of heat health alerts
- expected increase in cardiac arrests
- pressure on Ambulance Victoria's resources
- increased pressure on power supply due to expected air conditioner use
- heat fatigue on infrastructure
- the risk to tourists being exposed to extreme heat.
However, State Control Centre daily briefs show that the majority of information reported as the heatwave progressed was on preparedness for the consequential threat of fire. Monitoring the risk of fire included mapping and analysis of areas vulnerable to fire, and information about the potential for lightening, precipitation and synoptic forecasting for the state by the Bureau of Meteorology.
On Monday 13 January 2014, the State Operations Centre in New South Wales (NSW) advised Victorian stakeholders, including Victoria Police, that NSW had activated their State Heatwave Sub Plan, due to advice from the Bureau of Meteorology that a heatwave would affect southern NSW until a cool change arrived on Friday.
The Department of Health's daily situation reports included health surveillance data, other weather information such as fire status, and reports from health services such as Ambulance Victoria. However, while issues with power supply and demand on ambulance services are captured in these reports, the reports are primarily at the operations level. For example, one situation report stated that the department was receiving conflicting information about the available power supply across the state—if the management of the response to the 2014 heatwave was monitored and reported effectively, all agencies with key roles in heatwave response would be hearing the same message. Lack of clear information indicates that this is not happening in a coordinated manner through the relevant communication channels, or emanating from a lead agency.
The Ambulance Emergency Operations Centre was effectively utilised. Ambulance Victoria's health incident action plans were more comprehensive than the heatwave plans developed by other agencies and included mapping, resource needs, and activities being actioned. As the health commander in the field, Ambulance Victoria is best able to monitor and report on the impact of extreme heat across the state and across incidents.
Incident management systems
Integration of incident management systems provides greater interoperability—one of the key objectives of the current legislative arrangements. However, the audit found that during the January 2014 heatwave none of the audited agencies shared the same incident management system, although there was limited access to the municipal council system. In some cases, no information was captured in the system at all.
The emergency management centre operated by the Department of Health did not capture all actions in its incident management system—with multiple sources holding pieces of information. However, it did report on the preparedness of health services to respond to the heatwave. As health services consider heatwaves to be a risk to business‑as-usual operations—because of the threat to critical hospital infrastructure—they do not respond to heatwave as an emergency incident unless it extends their capacity to respond or results in infrastructure failure.
Victoria Police established an incident in their emergency management system for the heatwave, however, it did not provide any evidence of a lead response to this incident. There was insufficient interaction with other support agencies. Instead, the system captured the operational response, including copies of heat health alerts issued and daily state control centre briefings.
By contrast, the incident management system used by Ambulance Victoria provided an active view of its actions in managing its operational response to the heatwave. This included building resource capacity and monitoring of its incident action plans.
The Interim Emergency Management Strategic Action Plan, released in July 2014 by Emergency Management Victoria, includes implementing the first stage of a common operating system across key emergency services. The results of this first stage will inform the development of a business case for a full common emergency information platform.
Comparing the issues raised in the 2009 and 2014 heatwave debriefs conducted by the various key agencies, it is clear that the lack of an integrated system remains an issue. The current move towards developing a common operating system should help improve the level of interoperability, a key objective of the Emergency Management Act 2013.
2.4.2 Reporting arrangements
There has not been an integrated 'all hazards, all agencies' approach adopted to debrief on the 2014 heatwave event. While the Department of Health conducted a debrief of SHERP on 29 January 2014, there was no debrief that included all agencies with a recognised role in a heatwave emergency. Yet it is critical that all agencies come together to learn from the incident.
Audited councils did not conduct debriefs. There was also no reference to the heatwave in the minutes of municipal emergency management planning committee meetings after the heatwave period.
While Victoria Police did not conduct a specific heatwave debrief with all support agencies with roles in responding to heatwaves, it participated in a broader statewide post-summer season review that examined both fire and heatwave related issues.
The Department of Health's January 2014 debrief identified the following governance‑related issues:
- a lack of clear understanding by regions and health services about the role of Health Command in leading the health response
- a need for better communication with regions
- confusion over how much assurance the department was able to get from health services given the devolved structure
- the risk in not monitoring health service preparedness
- health service debrief should be conducted
- limited follow up and much assumption about what activation of heatwave plans actually means in practice in councils
- the need to build redundancy into the incident management leadership team.
A comparison between the heatwave debrief conducted in 2009 and the individual debriefs conducted by agencies after the 2014 heatwave shows that while some improvements have been made, some key issues remain. Figure 2D shows areas of improvement since 2009, as well as issues identified in the earlier heatwave that have not yet been fully addressed.
Figure 2D
Lessons learnt from heatwave debriefs in 2009 and 2014
|
Improvements since 2009 |
Issues common to both 2009 and 2014 |
|---|---|
|
Heatwaves are now a recognised emergency in the EMMV The integration of Ambulance Victoria into the Department of Health's emergency response centre provided a better health response Emergency management structures are consistent across tiers and within centres The Department of Health's State Emergency Management Centre has developed an operations manual Training of staff in emergency management roles has increased Heatwave framework elements have been developed. |
Clarity around roles and responsibilities Sufficiency of strategic monitoring Clarity around triggers for activation of heatwave plans Planning for business continuity Involving more agencies in control centres and debriefs Clarifying the role of councils Sharing of data across multiple systems Determining the most appropriate data needs for monitoring purposes Involving more agencies in training and exercises Improving public communication messages Streamlining the number of warnings issued Confirming the effectiveness of warnings. |
Source: Victorian Auditor-General's Office.
The absence of a lead agency to take responsibility for the response to heatwaves means it is less likely that the individual reports are considered in an integrated way. The failure to undertake a heatwave-focused debrief as a group, after the 2014 heatwave, compounds this issue.
Recommendation
- That Emergency Management Victoria, working with appropriate agencies, clarifies the control and other roles and responsibilities for heatwave arrangements.
3 Preparedness to respond to heatwaves
At a glance
Background
Emergency Risks in Victoria – Report of the 2012–13 State Emergency Risk Assessment identified heatwaves as one of 15 emergency risks to have potentially significant consequences if realised. Being well prepared to respond to a heatwave requires agencies to have plans in place that are evidence-based and meet requirements, and sufficient staff capacity and capability to respond.
Conclusion
Agencies are not well prepared to respond to heatwaves. They do not all have evidence‑based plans that meet requirements because there are currently no standardised requirements to develop sub-plans of the State Emergency Response Plan.
The lack of an integrated planning framework means the quality of state and municipal planning, including risk assessment, is variable and that agency shortfalls cannot be identified and addressed.
Findings
- There are no minimum requirements for the development of a state-level plan.
- The Heatwave Plan for Victoria is an operational plan, not a state-level plan for heatwaves.
- The quality of municipal heatwave plans is not monitored or reviewed.
- Not all agencies sufficiently plan for resource needs during summer.
- There is no assurance that health services are well prepared for the risk of critical infrastructure failure.
Recommendations
That Emergency Management Victoria:
- facilitates the development and implementation of coordinated whole-of-government heatwave arrangements
- facilitates the development of guidelines, including appropriate minimum standards for content in state-level sub-plans of the State Emergency Response Plan
- in developing the new emergency management planning legislation, clarifies the role of municipal councils and includes a quality assurance mechanism for municipal emergency management planning.
That the Department of Health assures itself that public health services are well prepared to manage the risk of critical infrastructure failure during a heatwave.
3.1 Introduction
The 2011 Green Paper, Towards a More Disaster Resilient and Safer Victoria, acknowledged risk-based planning and mitigation measures as critical to minimising the impact of emergencies and increasing community resilience. Being well prepared to respond to a heatwave requires agencies to have plans in place that are evidence-based and meet requirements, and sufficient and appropriate resources to be able to respond appropriately.
3.2 Conclusion
Agencies are not well prepared to respond to heatwaves. They do not all have plans in place that are evidence-based and there are no clearly articulated minimum requirements to guide the development of sub-plans of the State Emergency Response Plan (SERP).
The quality of planning at the state and municipal level, including the risk assessment process, is variable. There is no integrated planning framework to strengthen the quality of state and local‑level incident plans and provide assurance that agencies are well prepared to respond. As a consequence of the weaknesses in heatwave planning, shortfalls in the preparedness of key agencies are not identified and addressed appropriately.
3.3 Quality of planning
The audit assessed whether Victoria Police, the Department of Health (the department), Ambulance Victoria, and a selection of municipal councils and their neighbouring health services were well prepared to respond to heatwaves, including whether they:
- had plans in place that were evidence-based—informed by better practice, past reviews and evaluations
- had plans that met requirements in legislation, policy and standards
- planned for sufficient and appropriate resources.
3.3.1 Do plans meet requirements?
There are no requirements specified for emergency management incident plans. This is because SERP does not provide any guidance, and standards have yet to be developed.
The Heatwave Plan for Victoria – Protecting health and reducing harm from heatwaves
While the Heatwave Plan for Victoria assumes the title of a state plan, it is not commensurate with, or recognised as, a state-level plan in the emergency management arrangements. Sub-plans of the SERP include a State Bushfire Plan, State Flood Emergency Plan, State Tsunami Plan and the Victorian Emergency Animal Welfare Plan. There is no heatwave sub-plan.
There is no guidance in the Emergency Management Manual Victoria (EMMV) around minimum requirements or standards for development of state-level emergency management incident plans. An assessment of a sample of state-recognised sub-plans of the SERP found a lack of consistent content and form, including recognisable branding as a state-approved sub-plan of the SERP. While the lack of consistent branding had been identified in October 2010 by the Victorian Emergency Management Council, no changes have been made to the suite of plans listed in the EMMV as sub-plans of the SERP.
The Heatwave Plan for Victoria explains the elements of the department's heatwave framework and who is vulnerable in a heatwave emergency. However, it does not:
- adequately refer to the roles and responsibilities of other support agencies
- clearly articulate the phases of an emergency and the requirements at each phase
- make reference to Victoria Police as the control agency during a heatwave.
Its content indicates it is more of an operational plan of the State Health Emergency Response Plan than a state-level incident plan for heatwaves, as a sub-plan of the SERP.
Victoria Police
Victoria Police, as the control agency for heatwaves, does not have an appropriate response plan in place. In consultation with the department and other agencies, Victoria Police developed an Extreme Heat Event Plan, which was endorsed by the State Emergency Response Planning Committee in October 2010 as an interim plan. This interim plan was never intended to be a sub-plan of the SERP, and was developed to fill a void. Victoria Police is finalising a new heatwave operational plan which is intended to be released for the 2014–15 fire danger period.
Municipal councils
The role and requirements of councils in emergency management planning are not clear. Key planning and assurance requirements that exist under the 1986 legislation have yet to be reflected in the 2013 legislation. These include the requirement for councils to appoint a municipal emergency management planning committee, prepare and maintain a municipal emergency management plan (MEMP), and have the plan audited by the State Emergency Service (SES) every three years.
The audit reviewed heatwaves and emergency management planning in three regions identified as being at high risk of adverse health impacts from heatwaves. Each of the councils visited during the audit had a heatwave plan. One council had developed a multi-year emergency management schedule, which included committee meeting dates, and review dates for all council plans. This was an example of better practice. However, because there are various pieces of legislation for heatwaves where a heatwave plan could be developed—each with different levels of oversight of the planning process—the audit was unable to determine whether all councils in the state have a heatwave plan and whether these plans are of high quality and subject to regular review.
As Emergency Management Victoria (EMV) progressively reviews the current emergency arrangements, it will be opportune for EMV to clarify the role of municipal councils and to consider a quality assurance mechanism for municipal emergency management planning arrangements.
Health services
Health services accommodate and care for some of the state's most vulnerable people, who are particularly susceptible to extreme heat. For health services, a significant risk during a heatwave is the failure of critical infrastructure, such as air conditioning, including chillers, and the performance of emergency generators.
Health services plan for heatwaves as part of business continuity planning and in response to the department's Emergency Preparedness Clients and Services Policy. The policy advises health services that they must have emergency management plans in place, including activation triggers and communication arrangements. These plans should be reviewed, exercised, and updated regularly.
Recognising the risk of critical infrastructure failure, and given that health services are self-governing bodies, the department provides $25 million annually as part of the Engineering Infrastructure Program. However, the department does not mandate what equipment health services purchase, monitor maintenance of engineering infrastructure, or require health services to conduct power failure testing such as 'black start' tests. The department advised that this was the responsibility of health services as self-governing bodies.
In the January 2014 heatwave, the State Emergency Management Team was advised that hospitals might lose power on 16 January 2014 due to the forecast temperatures and the inability of the system to cool down. On 16 January 2014, Casey Hospital and Dandenong Hospital lost power and their emergency generators failed, which led to ongoing issues with air conditioning, water supply, lifts and medical equipment at Casey Hospital. Other health services experienced power failure during the heatwave, including Ouyen and Manangatang hospitals.
Figure 3A is an example of a health service response to an actual infrastructure failure—a fire in a power substation—during the 2014 heatwave. This occurred on Thursday 16 January 2014. The temperature on this day reached 41.4ºC in this community. In the same week, fires blocked the major freeway and threatened homes. It shows the range of actions the health service took to identify and treat the impact of the incident on business continuity and patient care.
Figure 3A
Case study – Health service response to infrastructure failure, 16 January 2014
|
Fire in power substation A loss of power across the region, at a major shopping centre and at various hospital sites resulted in the health service taking the following actions:
|
Source: Victorian Auditor-General's Office based on information provided by the audited agency.
While the department contacted health services during the 2014 heatwave and specifically requested confirmation on generators, this was not its usual or planned practice. As the department relies on health services self-reporting of infrastructure failure it is not known if other health services experienced failure during the 2014 heatwave.
Our examination of health service business continuity plans identified that health services had measures in place, such as load shedding, to manage the consequences of infrastructure failure. However, not all audited health service business continuity plans identified how long the health service could maintain operations should their generator or air conditioning systems fail. One of the larger health services had identified the risk of infrastructure failure and estimated that they would have less than five hours before needing to purchase or hire a new generator. After two hours, air conditioning, security and mortuary refrigeration system are at significant risk and the health service would be seeking support from other larger health services, particularly to relocate bodies from the mortuary.
As part of summer preparedness activities, both the department and health services should assure themselves that the risks associated with critical infrastructure failure during a heatwave are being appropriately managed.
3.3.2 Are plans evidence based?
Evidence-based emergency planning requires plans to be developed based on complete and accurate information and for risk-based assessments to have been completed. The audit found a lack of risk management expertise and quality assurance of heatwave planning at the local level.
By 2011, all 79 councils had been supported to develop heatwave plans, either as part of their municipal emergency management plan (MEMP) or as part of their municipal public health and wellbeing plan. The Heatwave Planning Guide – Development of heatwave plans in local councils in Victoria and toolkit were developed by the Department of Health to support this process.
The audit identified that municipal emergency management planning was often reactive and not sufficiently risk based to adequately inform the development of sub‑plans to the MEMP. These sub-plans, such as flood, pandemic and heatwave, rely on a risk assessment, with higher rated risks triggering the requirement for a sub-plan.
While there is a quality control process in place, through municipal emergency management planning committees, and an assurance mechanism, through SES audits of the MEMP every three years, there is a lack of risk management expertise and quality assurance at the local level. The SES audit process does not examine sub‑plans—such as for heatwaves—or the quality of plans.
Review of the 2013 legislation provides an opportunity for Emergency Management Victoria to clarify the role of municipal councils and to consider a quality assurance mechanism over municipal emergency management planning arrangements. The 1986 legislation includes the requirements for municipal emergency management plans, planning committees and the auditing of plans. Given the intent of the emergency management reform agenda to build community resilience, arming community leaders with sufficient expertise to build collective knowledge needs to be a consideration in any review of the existing arrangements. Collaborating across councils or having a specialist emergency management leader work across councils to improve the planning process would also be beneficial.
Evaluation of the Heatwave Plan for Victoria and Heatwave Planning Guide
The Heatwave Plan for Victoria and the Heatwave Planning Guide have not been updated since they were examined as part of an external evaluation of the Department of Health's heatwave framework in 2011. In that evaluation, 14 recommendations were made to improve the Heatwave Plan for Victoria, and three recommendations were made to improve the Heatwave Planning Guide.
An examination of the recommendations directed at improving the Heatwave Plan for Victoria, found that a number were merely suggestions and some are now obsolete. Recommendations not implemented included:
- clarity around the roles and responsibilities for control of a heatwave response, and the role of the regional office
- clarification of the trigger for activation of a heatwave plan
- broader stakeholder consultation to inform the heatwave plan
- distribution of communication resources from a single point
- inclusion of a communications strategy and stakeholder list.
The Heatwave Planning Guide recommendations were largely targeted at support tools and information provision to councils that did not require amendment to the guide. These recommendations have been implemented.
3.4 Surge capacity and capability planning
Sufficient and appropriate resources are not always available across all agencies to respond to heatwaves. Reduced staffing over the summer months affected some agencies' ability to respond effectively during both the 2009 and 2014 heatwaves.
SERP requires agencies to deploy resources to counter the effects of, or threat from, an emergency event. The audit assessed whether agencies had planned for sufficient and appropriate resources to respond to a heatwave.
3.4.1 Surge capacity
Heatwaves generally occur over summer when people take leave and there are increased numbers of visitors or tourists in Melbourne and surrounding areas. Reduced staffing affected the ability of some agencies to respond effectively during the 2009 and 2014 heatwaves.
All agencies reported difficulty in identifying which summer events were being held to enable them to plan for the additional demand that might be placed on service provision. Despite most events requiring a permit, there is no central database of events to assist agencies to plan for the influx of people, including information on where crowds are congregating. Instead, agencies spend time trying to source information on when and where events are occurring, often from each other, to plan for sufficient resources and maintain business continuity.
Municipal councils had to recall staff from holidays to make contact with vulnerable members of the community, whereas health services reduce their schedules over summer and were able to open up extra wards to accommodate the more vulnerable.
Demand for ambulance services
To meet the significant demand on its resources, Ambulance Victoria needed to bring in additional resources to be able to respond to demand during the January 2014 heatwave.
During that heatwave, the Triple Zero call-taker—Emergency Services Telecommunications Authority—responded to the highest ever number of calls for ambulance services. The record was set on Thursday 16 January, and then eclipsed the following day, on Friday 17 January.
Ambulance Victoria plans its resource needs a year in advance using a request and allocation process to inform their 'Resource Model'. The emergency operations area of Ambulance Victoria bids for resources as part of this process. For example, during the 2014 heatwave, Ambulance Victoria's Emergency Operations Centre had to request the provision of two additional paramedics to service the Ballarat region. This allocation was taken from the budgeted allowance in the resource model.
For additional resources, the Emergency Operations Centre has to organise additional vehicles and staff, usually by recalling staff from leave or through partnering arrangements with other emergency services. Additionally, Ambulance Victoria vehicles were recalled from scheduled maintenance to meet demand, which included movement of these resources across the state.
On 14 January 2014, heat health alerts had been issued for the whole of Victoria and were predicted to last until Friday 17 January in most districts. On this day—the second day of the heat health alerts being issued—the consequential impact of the heatwave on resources was already evident, not only on Ambulance Victoria but on other state emergency services. For example, bottled water was delivered to hydrate paramedics, fire-related road blockages hampered ambulance access to locations and additional crews were called to respond to firefighters suffering the effects of the heat.
While many of the activities highlighted are planned to address the risks associated with extreme heat conditions, they test the surge capacity of responding services, particularly when the community struggles to adapt to the conditions.
Ambulance Victoria has recognised that streamlining resource requests will improve the management of increased surge in an emergency and is currently developing an appropriate system to better address this.
3.4.2 Capability to respond
The state has yet to be fully tested on its ability to respond effectively to a prolonged heatwave. While training and emergency incident exercises are regularly provided for other incidents, there is insufficient recognition that the impact of extreme heat extends beyond public health and can drain available resources early.
Because the state has not developed a state level heatwave plan, the response to a heatwave emergency has not been tested or assessed.
All audited health services and municipal councils provided emergency management training to staff, usually through municipal emergency management planning committees and Victorian hospitals' emergency management committees. However, training is not integrated, with agencies organising training exercises through their respective planning and response committees in isolation from each other. Because of the lack of integrated training, more innovative and well-developed training exercises are not shared in a systematic way.
None of the audited councils had participated in an emergency management exercise with a heatwave component. However, one of the health services had conducted exercises that included a heatwave component linked to the failure of critical infrastructure. This is better practice given that critical infrastructure failure is a key risk to health services during a heatwave.
Figure 3B is taken from Exercise Devine which was conducted in November 2013, organised by one of the municipal emergency management planning committees, and involved all agencies in the region. This exercise, which includes extreme heat as a risk, could be applied to any incident where one of the consequences is power failure.
Figure 3B
Exercise Devine – A hypothetical power outage, 2013
|
For the past three days the temperature has been hovering around 38 degrees, with overnight temperatures in the low- to mid-twenties. At 4.16 am there was a major state disaster which has affected the State of Victoria. For the purpose of this exercise, the power outage has been caused by a significant disruption on the electricity transmission and/or distribution network. While this disaster is affecting other parts of the state, this exercise focuses on three municipalities in the western suburbs and the impacts of a localised hypothetical power outage across these three neighbouring municipalities. Initial assessments indicate repair activities for the state will take around three weeks. The electricity company will be required to source, transport and install transportable and temporary replacement power equipment to support the three municipalities. The electricity provider will experience significant delays to tie this equipment into the existing system given the nature and impacted areas of the disaster. It is anticipated that it will take approximately 72 hours to achieve full restoration. Restoration has commenced and, in the best case scenario, be available in three days. |
Source: Victorian Auditor-Generals Office, using Exercise Devine information.
In Exercise Devine, participants were asked to review their emergency management plans and determine how they would respond, and identify their key dependencies and the implications for business continuity.
A more proactive approach should be taken to heatwave preparedness by ensuring training covers a prolonged heatwave scenario. Training activities should test agency plans for such an event. Such a process will inform and improve the quality of agency planning.
Recommendations
That Emergency Management Victoria:
- facilitates the development and implementation of coordinated whole-of-government heatwave arrangements
- facilitates the development of guidelines, including minimum standards for content in state-level sub-plans of the State Emergency Response Plan
- in developing the new emergency management planning legislation, clarifies the role of municipal councils and includes a quality assurance mechanism for municipal emergency management planning.
That the Department of Health:
- assures itself that public health services are well prepared to manage the risk of critical infrastructure failure during a heatwave.
4 Activation and response to heatwaves
At a glance
Background
Public health messages and activation of heatwave plans by councils and community organisations that support vulnerable communities are two key actions taken to mitigate the risk that heatwaves present to public health.
Conclusion
The Department of Health's heatwave framework is sound and its Heat Health Information Surveillance System has improved understanding of the impact of extreme heat on public health in Victoria. However, its effectiveness is reduced because it is being applied selectively by agencies. Failure to provide sufficient and appropriate education, information and messages denies the community the opportunity to build resilience to manage extreme heat events and thereby reduce reliance on government intervention.
Findings
- Heat health alerts are not always clear or timely.
- The Heat Health Alert System does not follow the Victorian Warning Protocol and issue warnings using a phased approach.
- There is insufficient public education on the impact of extreme heat on public health—especially compared to other extreme weather events.
- Heatwave surveillance information does not sufficiently inform agency planning activities.
Recommendations
- That the Department of Health:
- develops a communication strategy for heatwaves that includes public awareness and education activities
- implements a phased approach to heat health alert warning categories in line with the Victorian Warning Protocol
- reviews the purpose and effectiveness of the Heat Health Information Surveillance System during a heatwave.
4.1 Introduction
In February 2014, the government released Emergency Risks in Victoria – Report Of The 2012–13 State Emergency Risk Assessment, which identified two key actions to mitigate the risk that heatwaves present to public health—public health messages and activation of heatwave plans by councils and community organisations that support vulnerable communities. Activation refers to the circumstances under which an agency applies its heatwave plan.
The Department of Health's (the department) heatwave framework, which aims to reduce the impact of extreme heat on public health, consists of the Heatwave Plan for Victoria, the Heatwave Planning Guide – Development of heatwave plans in local councils in Victoria for municipal councils, the Heat Health Alert System (HHAS), the Heat Health Information Surveillance System (HHISS) and communication resources. The audit assessed whether agencies had effectively applied the framework by examining whether:
- public health messages were appropriate—for example, clear, timely and well‑targeted
- heatwave plans were appropriately activated, monitored and reported
- the impact of extreme heat on public health had improved since 2009.
4.2 Conclusion
While the department's heatwave framework is consistent with international better practice, its effectiveness is reduced because its elements are being applied selectively by agencies. Lack of widespread understanding of the impact of extreme heat on public health means that public messaging needs to be targeting the whole community and not only the most vulnerable, who are less able to respond effectively without support. The ability of the community to adapt and build resilience to manage extreme heat events, and so reduce reliance on government intervention, depends on being able to access and understand the necessary information.
4.3 Public health messages
Public health messages are not always appropriate or well-targeted. This is because HHAS is not well understood and fails to target the whole community. Unlike other extreme weather events, extreme heat does not receive widespread media attention or advice about the potentially significant risks to health and how to prepare for and manage these risks. By contrast, 'sheep graziers alerts' are included on the Bureau of Meteorology website and on news channels during winter.
The department's communication resources and HHAS are the two key mechanisms in place to educate the community on the impact of extreme heat on public health and to warn about impending extreme heat conditions. This Part looks at the appropriateness of heat health alerts and whether public health messages meet the needs of the community.
4.3.1 Are heat health alerts clear and timely?
Heat health alerts are not always clear or timely. The HHAS, while soundly based, is applied selectively by the department and recipients. HHAS is intended to notify councils, departmental program areas, hospitals, and health and community service providers of forecast heatwave conditions likely to impact on human health, three to four days prior to the day of extreme heat. The Chief Health Officer authorises a heat health alert, which is emailed to key stakeholders.
The State Emergency Response Plan details 12 nationally recognised principles to be followed in providing warnings to the community. Figure 4A shows the extent to which the HHAS reflects these principles.
Figure 4A
Community warning principles and Heat Health Alert System
|
Community warning principles |
Heat Health Alert System |
|---|---|
|
Coordinated—warning system should avoid duplication of effort and support a shared understanding |
✔ |
|
Authoritative and accountable—warnings should be disseminated on the decision of an authorised person |
✔ |
|
Consistent/Standards-based—information content should be coordinated and consistent across all warning mechanisms |
✔ |
|
Complete—the message should include all relevant details, be easily understood and target the entire community |
✘ |
|
Multi-modal—the use of a variety of delivery mechanism should be complementary and allow maximum reach to the affected community |
✘ |
|
All hazards based—should be capable of providing warning for any type of emergency |
N/A |
|
Targeted—messages should be targeted to those 'at risk' to reduce complacency from 'over warning' |
✔ |
|
Interoperable—coordinated delivery methods should be capable of operation across jurisdictional borders |
✔ |
|
Accessible and responsive—warning systems should be developed with capability to respond to, and deliver warnings in, an environment of demographic, social and technological change |
✔ |
|
Verifiable—the warning is able to be verified by the community, to reduce accidental activations and prevent malicious attempts to issue false alerts |
✔ |
|
Underpinned by education and awareness raising activities—agencies should be active in the community to raise awareness and educate people regarding emergency warning systems/mechanisms and the language used in warnings for particular emergencies |
✘ |
|
Compatible—the warning system should be compatible with existing telecommunications networks and infrastructure to avoid adverse impacts on their functional integrity |
✔ |
Note: N/A refers to a principle that is not relevant to the system under examination.
Source: Victorian Auditor-General's Office based on the Victorian Warning Protocol.
The principles are included in the Victorian Warning Protocol, which was established to provide emergency response agencies with coordinated and consistent direction on advice and/or warnings. Figure 4A shows several key elements that are absent in the HHAS, including the completeness of the warning and the 'all hazards' approach.
Timeliness of alerts
Alerts are not always timely. In the January 2014 heatwave, around 36 per cent of alerts were not issued within three to four days prior to the day of extreme heat. The department monitors a selection of weather stations throughout the state. Specific stations within each weather forecast district have been identified in consultation with the Bureau of Meteorology as the trigger stations for issuing an alert. This means that areas within a district may be forecast to exceed the heat health temperature threshold but receive no warning if the trigger location is not forecast to meet or exceed the threshold.
Figure 4B shows the number of days warning provided before the forecast heatwave. In some cases, the temperature is only forecast to meet or exceed the threshold one to two days prior. For example, an alert was issued for East Gippsland on 16 January for 17 January, because the threshold was only forecast to be exceeded the day before. However, the alert issued for the Northern Country on 13 January for 15 January was forecast to be exceeded as early as 9 January. Alerts may also be delayed because the department does not assess forecast data or issue alerts on weekends. A lower number indicates a shorter warning time being provided.
Figure 4B
Number of days warning provided – 2014
|
Forecast district |
13 Jan |
14 Jan |
15 Jan |
16 Jan |
17 Jan |
18 Jan |
|---|---|---|---|---|---|---|
|
Central |
N/R |
5 |
2 |
3 |
2 |
N/R |
|
East Gippsland |
N/R |
4 |
N/R |
N/R |
1 |
N/R |
|
Mallee |
4 |
5 |
2 |
3 |
N/R |
N/R |
|
North Central |
4 |
5 |
2 |
3 |
4 |
N/R |
|
North East |
N/R |
5 |
2 |
3 |
4 |
2 |
|
Northern Country |
NA |
5 |
2 |
3 |
2 |
N/R |
|
South West |
N/R |
1 |
2 |
3 |
N/R |
N/R |
|
West and South Gippsland |
N/R |
4 |
0 |
N/R |
2 |
N/R |
|
Wimmera |
N/R |
5 |
2 |
3 |
N/R |
N/R |
Note: N/R means that an alert was not required for that location for that date.
NA means that although the temperature was identified to meet or exceed the threshold, no alert was issued.
Source: Victorian Auditor-General's Office based on the Department of Health heat health alert workings, using forecast temperatures and heat health alerts issued in 2014.
Figure 4B shows that in some cases, such as West and South Gippsland on 15 January, there was no early warning, with the alert being issued on the same day as the temperature was forecast to meet or exceed the heat health threshold. In some cases the department did not issue an alert when the trigger location was forecast to meet or exceed the threshold until a number of days after first identified. By applying the framework selectively, the timeliness of alerts is reduced.
Case study: Central Weather District
The Central Weather District covers 40 individual municipal councils—50 per cent of all councils—including Ballarat City Council, Melbourne City Council, Greater Geelong City Council and Mornington Peninsula Shire Council. Figure 4C shows the varying mean temperatures across a sample of weather stations in this district. The threshold for the central forecast district is 30ºC. As Figure 4C shows, some locations reached the threshold and some did not.
Figure 4C
Central weather forecast district temperature comparison, 2014
|
Date |
Mornington Peninsula City Council |
Ballarat City Council |
Brimbank City Council (based on Essendon) |
Bass Coast Shire Council (based on Wonthaggi) |
Casey City Council (based on Cranbourne) |
Geelong City Council |
|---|---|---|---|---|---|---|
|
14 Jan |
33.10ºC |
32.05ºC |
36.10ºC |
31.65ºC |
34.15ºC |
35.10ºC |
|
15 Jan |
30.50ºC |
29.90ºC |
33.65ºC |
29.95ºC |
30.35ºC |
30.10ºC |
|
16 Jan |
32.85ºC |
30.65ºC |
33.10ºC |
28.95ºC |
29.05ºC |
31.20ºC |
|
17 Jan |
28.75ºC |
29.25ºC |
32.30ºC |
30.60ºC |
29.80ºC |
32.05ºC |
Source: Victorian Auditor-General's Office, using Bureau of Meteorology data.
The temperature variability shown in Figure 4C—with variance being as much as 4ºC —highlights the importance of monitoring local conditions to determine what strategies need to be adopted. For example, councils may need to decide whether to continue home visits to the elderly or to conduct welfare checks by phone. Differences in mean temperatures may require different responses in locations within the same district in order to protect vulnerable communities.
Clarity of alerts
Alerts are not always clear and are not consistent or interoperable with warning systems used for other emergency incidents. The content of alerts in 2014 did not always change as the heatwave progressed.
On the day after the last heat health alert in both the 2009 and 2014 heatwaves, ambulance services, health services and the Coroner were still experiencing high demand. The department needs to assess the purpose of the alert system and determine how a phased approach might enable agencies to remain alert to the continuing impact and risk of heat on public health after the heatwave has ended.
Other jurisdictions' heatwave plans, and other extreme weather alerts, adopt a phased approach. Under the Victorian Warnings Protocol 2013, it is recommended that agencies identify the warning category for alerts—advice, watch and act, and emergency warning—to inform communities of an impending or current threat and to promote appropriate actions.
All audited councils had developed extreme heat policies to manage the impact of heat on staff. Councils also forwarded the heat health alert internally to staff responsible for Home and Community Care (HACC) programs, which provide services such as the delivery of meals, domestic cleaning, home maintenance and social support to the elderly.
Figure 4D is an example of how a heat health alert is disseminated by councils. The audit found that there was no consistent method adopted, although the sampled councils all advised their HACC teams.
Figure 4D
Dissemination of a heat health alert by councils
Source: Victorian Auditor-General's Office based on information provided by councils.
The subjectivity attached to the issuing of heat health alerts, the variable approaches by councils in responding to these alerts, and the lack of consistent language in warning systems, present a risk to the community—particularly the most vulnerable—and to agencies that are unable to adequately determine how critical the warnings are.
4.3.2 Do messages meet the needs of the community?
Public health messages do not meet the needs of the community. They are not easily understood and do not target the whole community. While messages are primarily targeted to the most at risk—the aged and infirm—they need to be more broadly disseminated and sufficiently detailed so that the community fully understands the significance of the impact of extreme heat on public health. Building community resilience in this way will help reduce reliance on government intervention, particularly on Ambulance Victoria as the first port of call for a heat-related condition emergency.
The department has conducted Regional Health and Ageing Summer Preparedness forums throughout regional Victoria and in Melbourne for a number of years. These forums target agency staff and service providers. The department also provides information on how to develop heatwave plans and which activities should be conducted to support the plan—such as staff training.
Information for people vulnerable to extreme heat
Information is not always clear to the targeted groups. During the 2014 heatwave, multiple emergency incidents were in progress—including fires, the threat of power failure and heatwave conditions. Despite joint media conferences by emergency management leaders, stakeholders still reported hearing contradictory messages about fire awareness, energy consumption and keeping cool. For example, stakeholders reported that elderly Victorians, who are among the most vulnerable to extreme heat, were restricting the use of air conditioners because of advice to conserve power.
HACC teams in the audited councils had developed heatwave vulnerability lists to identify clients who were at increased risk in extreme heat. During the 2014 heatwave, councils contacted people on this list when a heat health alert was received. However, councils are only aware of people who are accessing their services, which means that not all vulnerable people are being contacted. This highlights the need for public information to be widely available prior to and during a heatwave.
In 2014, it was not until 16 January that the first print media advertisements on heat health were placed in newspapers. Yet by 15 January 2014, the department had identified through its surveillance information that heat-coded ambulance dispatch callouts were 11 times higher than normal and NURSE-ON-CALL heat-related calls were double the average.
Figure 4E illustrates the increase in the number of the department's Better Health Channel website resources viewed or downloaded as members of the public sought more information.
Figure 4E
Comparison of website hits for Better Health Channel factsheets
|
Better Health Channel factsheets |
6–12 January 2014 |
13–18 January 2014 |
Increase (per cent) |
|---|---|---|---|
|
Child safety – hot weather |
405 |
2 170 |
435 |
|
Heat stress – preventing heat stroke |
167 |
552 |
230 |
|
Heat stress and heat related illness |
2 381 |
7 848 |
229 |
|
Heat stress and the elderly |
125 |
544 |
335 |
Source: Victorian Auditor-General's Office based on Department of Health's evaluation report January 2014 Heatwave Communications.
The Better Health Channel website reported increased traffic between 13 and 18 January 2014, compared to the previous week. The biggest increase was for information on child safety in hot weather, which increased by 435 per cent.
Thirty per cent of heat health calls to NURSE-ON-CALL in 2014 were related to children.
However, while multi-modal forms of messaging are required, not all people vulnerable to heatwave have access to the internet or would understand where to find relevant information. Therefore, it is important for information to be broad based so that family and friends can support those who may be at risk—including young children, pregnant women and people on certain medications. Public health requires a whole of community response.
There is insufficient education and public information on the impact of extreme heat to assist the general public in preparing for heatwaves and to build resilience within the community.
Unlike Total Fire Ban alerts, and despite improved coverage in 2014, heatwave conditions receive minimal media coverage. Despite the higher level of estimated mortality from heatwaves in Victoria, there is inadequate focus on the risks associated with extreme heat and ways to manage these risks.
Communities are not being given sufficient information to make informed decisions, including modifying their behaviour, in the heat. For example, in the 2014 heatwave, Ambulance Victoria reported attending 60 cases of children being locked in hot cars. This occurred despite the Better Health Channel website's advice never to leave babies or young children in a car, a similar reminder in a department media release, a public announcement on the ABC, and information being relayed through NURSE-ON-CALL. Without a public education campaign that includes advice on adapting to, preparing for and coping with, the impact of extreme heat, the premature death of Victorians during these types of emergency events is likely to continue.
Communication resources
All audited health services and municipal councils reported that the department's communication resources contain appropriate heatwave messages but identified opportunities to improve how well they distribute the department's information in their communities.
Brochures and information booklets on heat stress and the elderly, young children and heat, preventing heat stroke, heat-related illness, and heat stress and sport can be downloaded from the department's Better Health Channel website.
Figure 4F is an example of a brochure available online.
Figure 4F
Staying healthy in the heat
Source: Department of Health's website, www.health.vic.gov.au.
These resources provide a consistent set of messages and are readily available. One of the key principles of community warnings is that the community should be able to verify the message. However, no resources included information on how to calculate the heat health threshold or the importance of the heat health alert. This information is important for agencies and individuals who need to seek advice or check on relatives.
A 2011 evaluation of the heatwave framework made recommendations aimed at improving communication resources, including:
- consideration of the use of social media
- targeting resources to other vulnerable groups—including children, people with a disability, and culturally and linguistically diverse communities
- making the presentation of resources more visually accessible to the elderly.
4.4 Activation of heatwave plans
Activation of agency heatwave plans is not consistent, monitored or reported. Because there are no clearly outlined expectations about what actions will be activated as an incident progresses, different approaches have been applied. This has resulted in an inconsistent understanding of what activation of a heatwave plan means.
To determine whether the activation of heatwave plans was effective, we examined whether activation was monitored and whether issues were reported and addressed.
4.4.1 Is activation consistently applied?
Unlike other jurisdictional state-level heatwave plans, the Heatwave Plan for Victoria – Protecting health and reducing harm from heatwaves does not specify a phased approach using the prevention, preparedness, response and recovery approach, and lacks clear expectations of agency actions. This means that activation in 2014 was interpreted as anything from sending out a summer newsletter, or forwarding a heat health alert, to establishing an incident control centre. Audited councils that had a phased approach in their heatwave plans had a better understanding of activation and could clearly demonstrate at what phase they would move to response activities.
The department, through regional emergency management teams, requested councils to confirm activation of their heatwave plan, including what strategies they had implemented. Not all councils responded and the responses varied. Reported strategies included:
- extending swimming pool hours
- providing water at cool places such as libraries
- organising transport home from cool places for the elderly
- adjusting outside play time at children services
- shopping for clients
- modifying Meals–on-Wheels delivery
- implementing staff policies on working in hot weather.
In late January a second spike in extreme heat occurred. The department surveyed councils on 30 January 2014. The survey did not ask councils whether they had activated their heatwave plans, rather, which strategies from a predetermined list of 12 they had implemented.
Figure 4G shows the strategies implemented by councils to manage the impact of heatwaves on their communities within the forecast weather districts.
Figure 4G
Heatwave strategies implemented by councils within weather forecast district, 30 January 2014
|
Strategy |
C |
NE |
EG |
NCY |
SW |
WSG |
M |
NC |
W |
Total |
|---|---|---|---|---|---|---|---|---|---|---|
|
Number of councils |
37 |
7 |
1 |
6 |
8 |
4 |
4 |
4 |
5 |
76 |
|
Promote heatwave awareness |
37 |
7 |
1 |
6 |
8 |
4 |
3 |
4 |
4 |
74 |
|
Disseminate heatwave materials |
37 |
7 |
1 |
6 |
8 |
4 |
3 |
4 |
4 |
74 |
|
Brief staff and key agencies about heatwave plan responsibilities |
34 |
7 |
1 |
6 |
7 |
4 |
2 |
4 |
5 |
70 |
|
Encourage family and friends to contact vulnerable people |
32 |
7 |
1 |
5 |
6 |
4 |
3 |
4 |
4 |
66 |
|
Notify service providers of vulnerable population groups of impending heatwaves |
31 |
7 |
1 |
5 |
5 |
3 |
3 |
4 |
5 |
64 |
|
Increase outreach to vulnerable population groups |
31 |
5 |
0 |
3 |
7 |
2 |
4 |
4 |
4 |
60 |
|
Promote NURSE-ON-CALL |
21 |
7 |
1 |
4 |
4 |
4 |
3 |
4 |
3 |
51 |
|
Identify and promote safe, cool, public places |
24 |
7 |
0 |
5 |
2 |
0 |
2 |
3 |
3 |
46 |
|
Extend hours of air conditioned council buildings |
14 |
6 |
1 |
6 |
1 |
1 |
1 |
3 |
3 |
36 |
|
Prompt institutions accommodating vulnerable populations to implement heatwave plans |
17 |
0 |
0 |
1 |
4 |
1 |
2 |
0 |
3 |
28 |
|
Implement cancellation policy for outdoor sport |
17 |
0 |
0 |
0 |
1 |
0 |
0 |
2 |
1 |
21 |
|
Establish cooling centres |
5 |
0 |
0 |
1 |
1 |
0 |
0 |
0 |
1 |
8 |
Note: C=Central, NE = North East, EG = East Gippsland, NCY = Northern Country, SW = South West, WSG = West & South Gippsland, M = Mallee, NC = North Central, W = Wimmera.
Note: 76 out of 79 councils responded
Source: Victorian Auditor-General's Office based on Department of Health council survey responses.
Figure 4G shows that the least implemented strategies were establishing cooling centres and the implementation of a cancellation policy for sport and recreation events. The most commonly implemented strategies were to promote heat awareness and disseminate heatwave awareness material. Only five of the surveyed councils did not implement these two strategies.
The survey asked whether councils had notified service providers with vulnerable clients to activate their plans. To this question, 80 per cent of councils responded positively.
It was only within the department's Hume region that all councils in the region reported that they had notified providers who were responsible for vulnerable population groups of the impending heatwave. This departmental region includes councils in multiple weather forecast districts, including North East, North Central and Northern Country.
The wide variety of strategies used by councils highlights the need for a more consistent approach to the activation of heatwave plans at the municipal level. Even for strategies that are fundamental to an adequate response—such as promoting heatwave awareness, disseminating heatwave materials, briefing staff and key agencies about responsibilities, and notifying services providers of vulnerable population groups regarding the impending extreme heat—there was not active engagement in these strategies.
4.4.2 Is activation monitored and reported?
Monitoring and reporting of activation is variable. Because roles and responsibilities for managing the response to heatwaves are not clear, oversight of response activities is done through functional levels and is not part of a systematic assessment of actions.
Health services
In the 2014 heatwave, the department monitored the activation of heatwave plans by health services appropriately, although acknowledged it would not normally do this under the devolved governance model. Through its role as Health Command, the department contacted health services, advising them of the extreme heat conditions and asked them to confirm:
- the key contact person
- that they had an alternate power source and had checked its operation
- that their heat health operation plan was in place for staff and patients
- that they had capacity to increase staffing to meet demand.
Heat health action plans were also completed and provided by regional office staff to monitor whether health, community health or aged care providers had ceased providing services. This level of monitoring was timely and appropriate.
Councils
It is not clear who is responsible for monitoring activation of council heatwave plans—the department as the support agency for managing the impact of extreme heat on public health, Victoria Police as the control agency for heatwave emergencies, or another agency altogether.
None of the audited councils activated their municipal emergency coordination centre. Councils also reported that a heatwave alone would be unlikely to activate the centre.
The department's survey of councils in 2014 is a good initiative, but there is no clear guidance around which strategies have proven to be most effective with which groups of people. This represents a missed opportunity to collect data around better practice and develop a more consistent approach to heatwave plan activation at the local level.
4.4.3 The Heat Health Information Surveillance System
The HHISS has contributed to a better understanding of the impact of extreme heat on Victorians, providing the evidence-base to further improve the state's response to heatwaves in a targeted and comprehensive manner at all levels of government.
The heatwave framework aims to reduce the impact of extreme heat on public health. To monitor achievement of this outcome, the department developed the HHISS. Information from this system has been used to produce two reports on the impact of the 2009 and 2014 heatwaves on public health.
The system accesses data on temperature, health service activity and mortality to generate a surveillance report used to assess public health risk from heat and to support emergency planning. HHISS reports are produced weekly from November to March, and daily during an extreme heat event. However, the HHISS only uses metropolitan data, primarily from the central weather forecast district. While HHISS data was assessed on a daily basis during the January 2014 heatwave, significant lags were experienced from some data sources, which affected the capacity of the system to provide real-time surveillance information.
The HHISS is unable to confirm causality between the department's heatwave framework and a reduction in mortality during the 2014 heatwave. However, as there was no heatwave framework in place during the 2009 heatwave, the development of the current framework elements should be acknowledged as important steps in the right direction.
The 2011 evaluation of the heatwave framework recommended a formal evaluation of the HHISS. This would assist the department to identify the cost benefits of the continued use of the HHISS and potential opportunities for leveraging the current data.
4.4.4 Impact on public health
While there was a reduction in the estimated number of deaths during the 2014 heatwave, the department is not able to clearly attribute this outcome to the implementation of its framework. However, in 2009 there was no heatwave framework in place. This means that the framework and collective efforts of all agencies have had an impact on the reduction in excess deaths in 2014.
The heatwave framework includes many of the elements accepted by leading international health and meteorological organisations as being essential to respond to the significant health risks associated with heatwaves. The fact that the department has implemented an evidence-based approach to the management of heatwaves in Victoria is a sound step.
However, further refinement of the framework—including addressing the gaps identified in this audit and in the 2011 heatwave evaluation—is needed in order to improve the state's capacity to prepare for and respond to more frequent and more prolonged extreme heat events in the future.
Recommendations
That the Department of Health:
- develops a communication strategy for heatwaves that includes public awareness and education activities
- implements a phased approach to heat health alert warning categories in line with the Victorian Warning Protocol
- reviews the purpose and effectiveness of the Heat Health Information Surveillance System during a heatwave.
Appendix A. Audit Act 1994 section 16—submissions and comments
Introduction
In accordance with section 16(3) of the Audit Act 1994, a copy of this report, or part of this report, was provided to the Department of Health, the Department of Human Services, the Department of Justice—which includes Emergency Management Victoria— Ambulance Victoria, Victoria Police and the three audited councils and three audited health services
The submissions and comments provided are not subject to audit nor the evidentiary standards required to reach an audit conclusion. Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
Further audit comment:
RESPONSE provided by the Secretary, Department of Health
RESPONSE provided by the Secretary, Department of Justice
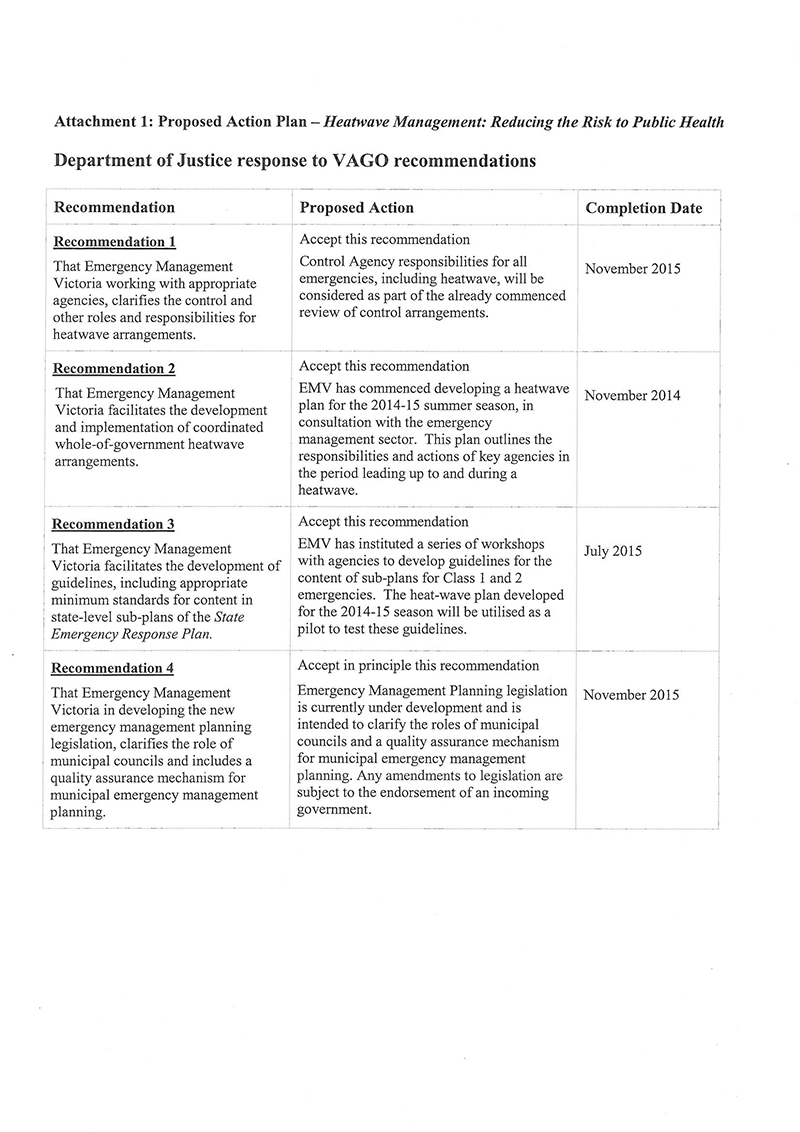
RESPONSE provided by the Chief Executive Officer, Ambulance Victoria
RESPONSE provided by the Chief Commissioner, Victoria Police
Auditor-General’s response to Victoria Police
Victoria Police has indicated that: ‘The report appears to be critical of the focus on the response to bushfires during the period of the 2014 heatwave, but does not provide any constructive commentary on how bushfire agencies could more effectively integrate the heatwave response into the response for bushfires’.
Our report does not suggest that the focus on bushfires should have been reduced—rather it makes the point—pages ix, 17 and 18—that there should have been a commensurate focus on the impact of heatwaves. There was no statewide, strategic view of the combined impact of the different emergencies. VAGO has not examined the bushfire management arrangements as part of this audit. But, it is open to agencies responsible for the management and response to heatwaves to consider how they might integrate these arrangements with those already existing for bushfires, as Victoria Police has suggested.
Further, Victoria Police has stated that the ‘strategic approach’ adopted by Victoria Police with the Department of Health ’has not been fully recognised in the report’. Our report—page 17—lists some of the strategic responsibilities of a control agency under the emergency management arrangements. These include managing all response activities, leading multi-agency response planning, and collecting, analysing and disseminating information regarding the emergency. Victoria Police did not assume these responsibilities in the 2014 heatwave. Even where Victoria Police took leadership actions—for example, in some regions—these were not strategic, systematic or sustained. The ‘strategic approach’ referred to by Victoria Police consisted of an informal arrangement that DH would lead the health response in a heatwave. However, this ‘strategic’ approach involved one agency, not all support agencies, and focused on health only, and not the full range of potential hazards and risks.
