Mental Health Strategies for the Justice System
Overview
The increasing incidence of people living with mental illness in the community means that justice and health agencies are experiencing significant challenges. There are increasing interactions between people with a mental illness and criminal justice agencies, and a lack of capacity to adequately respond to and manage these needs.
Justice and health agencies recognise the importance of addressing mental health issues within the criminal justice system. All have implemented initiatives that aim to improve outcomes, but significant gaps remain.
There is currently no overarching strategy or leadership for mental health and the justice system that focuses on improving outcomes for people with a mental illness. Where plans do exist, they are limited to agencies’ own areas of responsibility, or only address parts of the justice system.
While there is evidence of agencies working together, this is neither uniform nor sufficiently coordinated to address mental illness effectively.
Responsibility for coordinating the agencies is unclear, and there is a lack of accountability for the success or failure of responses across the criminal justice system. This is likely to further limit the effectiveness of coordination, collaboration and planning, as actions rely on individual agencies, their relationships and their ability to take a system-wide perspective.
Mental Health Strategies for the Justice System: Message
Ordered to be printed
VICTORIAN GOVERNMENT PRINTER October 2014
PP No 366, Session 2010–14
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
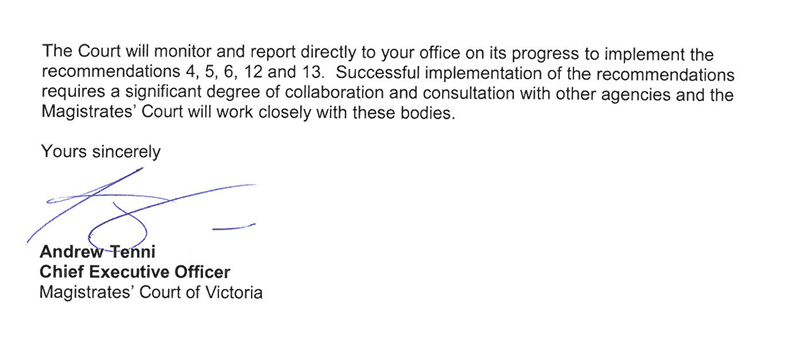
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report on the audit Mental Health Strategies for the Justice System.
This audit assessed the effectiveness of planning and coordination for mental health across Victoria's criminal justice system.
The audit found that justice and health agencies recognise the importance of addressing mental health issues within the criminal justice system. However, there is currently no overarching strategy or leadership for mental health and the justice system that focuses on improving outcomes for people with a mental illness.
While there is evidence of agencies working together, this is neither uniform nor sufficiently coordinated across the justice system to address mental illness effectively. Further collaboration and coordination would likely enhance the overall outcomes for people with a mental illness.
Yours faithfully
John Doyle
Auditor-General
15 October 2014
Auditor-General's comments
 John Doyle Auditor-General |
Audit team Chris Sheard—Engagement Leader David Cook—Team Leader Kerryn Riseley—Analyst Matthew Irons—Analyst Engagement Quality Control Reviewer Dallas Mischkulnig |
Mental illness is a significant issue for our community. About half of all people aged between 16 and 85 will experience a mental illness in their lifetime. In any year around 20 per cent of the community experience a mental illness, of which 16 per cent have a severe mental illness.
The rate of mental illness among people involved with the criminal justice system is much higher than the community generally. Around 40 per cent of prison entrants have previously been told they have a mental illness.
Recently, greater efforts have been made to understand how governments, health and human service providers can work together to improve outcomes for people with mental illness. There is recognition that services must be more integrated and coordinated, and include physical health, alcohol and drug dependency, family support, education and employment, and housing components.
In this audit I examined how the criminal justice, health and human services agencies are working together to better manage and address the needs of people with mental illness. I examined cross-agency planning and coordination to assess whether agencies are effectively working together to improve their responses to people with mental illness.
My audit found evidence of work underway to develop links between policing and mental health services, and of the continued development of specialist courts and support programs to help people with mental illness and other needs address the issues that lead to their offending. The Department of Justice is also preparing for a large increase in the number of specialised mental health beds in the prison system in 2017.
However, my audit found that there are gaps with planning, collaboration and coordination. There is no overarching leadership or strategy for mental health in the criminal justice system that could provide the basis for focusing and coordinating agencies' responses.
Addressing these gaps could improve the justice system pathways and outcomes for people with a mental illness. Agencies would be better able to prioritise development of existing initiatives to maximise outcomes for the justice system as a whole. More effective collaboration would improve links between existing services, and provide the basis for developing new services.
I have made a number of recommendations to address these issues, which pleasingly, Victoria Police, the departments of Justice, Health and Human Services, and Court Services Victoria have accepted. My recommendations reinforce the need for agencies to collaborate in planning and developing their responses to mental illness in the justice system.
It is especially pleasing that as a result of the audit, the agencies involved have already taken steps to establish a forum with the seniority required to lead a coordinated response to mental illness across the justice system.
I would like to thank the staff of Victoria Police, the departments of Justice, Health and Human Services, and Court Services Victoria for their assistance and cooperation during this audit.
I look forward to receiving updates from them in implementing the recommendations.
John Doyle
Auditor-General
October 2014
Audit Summary
Good mental health is one of the foundations of a good life and a healthy society. The World Health Organisation broadly defines mental health as 'a state of wellbeing in which every individual realises his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community'.
Almost 50 per cent of people aged 16 to 85 years will experience one or more mental illnesses—such as anxiety, mood and substance-use disorders—in their lifetime.
These illnesses can have significant impacts on individuals and their quality of life, including impairing their mental functioning and capacity to maintain relationships. They can also cause a person to come into contact with the criminal justice system. Rates of mental illness among people interacting with police, the courts and the corrections agencies are much higher than in the community generally.
A range of criminal justice agencies will often have to manage people with a mental illness:
- Victoria Police provides initial response to incidents involving people with a mental illness. It intervenes by responding to incidents, and where necessary arresting and managing people with a mental illness in police cells.
- The Magistrates' Court sentences offenders—including those with a mental illness—and aims to divert them from the criminal justice system where appropriate.
- The Department of Justice (DOJ), through Corrections Victoria and Justice Health, manages and treats prisoners with a mental illness while incarcerated, while on parole, and on corrections orders.
In addition, the Department of Health (DH) sets priorities and funds mental health services that treat and manage people in contact with the criminal justice system.
While these agencies operate independently, they rely on each other when dealing with people with a mental illness. Better practice research indicates that joint planning and coordination is required where policy issues span the responsibilities of more than one agency, where agencies' responsibilities are interdependent, or where coordinating services can reduce costs and increase quality for end users.
This audit examined the effectiveness of planning and coordination for mental health across Victoria's criminal justice system, as the foundation for effective responses to people with a mental illness.
Conclusions
The increasing incidence of people living with a mental illness in the community means that justice and health agencies are experiencing significant challenges. There are increasing interactions between people with a mental illness and agencies within the criminal justice system, and a lack of capacity to adequately respond to and manage these needs. This is particularly evident for Victoria Police and for Corrections Victoria.
Justice and health agencies recognise the importance of addressing mental health issues within the criminal justice system. All have implemented initiatives that aim to improve outcomes, but significant gaps remain. In the face of the increasing incidence of people with a mental illness interacting with the criminal justice system, a whole‑of‑system approach is required.
There is currently no overarching strategy or leadership for mental health and the justice system that focuses on improving outcomes for people with a mental illness. Where plans do exist, they are limited to agencies' own areas of responsibility, or only address parts of the justice system.
While there is evidence of agencies working together, this is neither uniform nor sufficiently coordinated across the justice system to address mental illness effectively. Further collaboration and coordination would likely enhance the overall outcomes for people with a mental illness.
Responsibility for coordinating the agencies is unclear, and there is a lack of accountability for the success or failure of responses across the criminal justice system. This is likely to further limit the effectiveness of coordination, collaboration and planning, as actions rely on individual agencies, their relationships and their ability to take a system-wide perspective.
The lack of effective planning and collaboration is inconsistent with several major strategic statements from the health and justice portfolios since 2009. These identified that justice, mental health, disability and other services such as housing, must work closely together if better outcomes are to be achieved for people with a mental illness coming into contact with the justice system.
Findings
Police response and arrest interventions
Victoria Police performs a critical role responding to people with a mental illness. Its role is at the 'front end', managing incidents caused by personal crisis, behaviour suggestive of mental disorder, or the effects of alcohol and other drugs.
The nature of Victoria Police's role in responding to people with a mental illness means that it routinely interacts with the health system, hospitals and DH. As such, both it and DH need to effectively collaborate and plan to maximise outcomes for people with a mental illness.
Until recently these agencies have focused planning in their own areas of responsibility. However, they are now working towards a joint plan to develop effective responses to mental illness. This has the potential to improve outcomes for people with a mental illness, whose interaction with mental health services results from their contact with police.
The level of inter-dependence between Victoria Police and DH necessitates effective collaboration and coordination. Since 2006, both agencies have sought to engage around mental illness, but have found it difficult to resolve issues and strategically collaborate. However, since 2012 Victoria Police and DH have both taken steps to strengthen their strategic engagement, and are working towards an agreed framework to oversee and address areas of inter-dependence.
Victoria Police and DH have longstanding mechanisms to support local communication and coordination between police, ambulance, area mental health services (AMHS) and hospital emergency departments. However, Victoria Police and DH will need to devote ongoing attention to ensure emergency services liaison committees (ESLC) are effectively maintaining local coordination.
Courts-based interventions
The Magistrates' Court hears criminal charges brought by police, makes findings in relation to guilt and makes sentencing orders. Courts may also obtain mental health assessments in considering criminal cases, particularly where an accused's mental illness may satisfy the criteria under relevant legislation.
The Magistrates' Court has successfully piloted specialist courts and programs to divert offenders with a mental illness to treatment, and address the causes of their offending. The specialist courts and programs play a key role by reducing rates of imprisonment.
However, there is no current plan guiding the development of the Magistrates' Court's specialist courts and support programs for people with a mental illness—including a framework describing the role these initiatives could play if they were extended beyond their current pilot locations to operate more widely across the Magistrates' Court's 12 major regional locations.
Prior to July 2014, DOJ provided policy, project and program management support, and led inter-agency communication around the Magistrates' Court's programs. DOJ's support enabled development of the Magistrates' Court's specialist courts and support programs for mental illness. From 1 July 2014, Court Services Victoria (CSV) has taken over responsibility for the Magistrates' Court's administrative and operating support, and management of specialist courts and support programs.
There is no agency-level forum in which DOJ, CSV, Victoria Police, DH and the Department of Human Services (DHS) are able to discuss strategic issues aimed at reducing offending and improving recovery of people with a mental illness in the criminal justice system.
Police custody and prison-based interventions
Holding offenders in custody provides an opportunity to both identify and treat mental health issues. When detained in police cells, individuals are in the legal custody of the Chief Commissioner of Police and Victoria Police provides health services as part of its custodial responsibility. Prison health services provide voluntary psychiatric consulting, nursing and inpatient treatment for prisoners with a mental illness. Under the Mental Health Act 2014 compulsory mental health treatment cannot be provided in prisons.
As offenders frequently move between police cells and prisons, effectively addressing their mental illness is complex. It requires effective collaboration between Victoria Police, DOJ, DH and other corrections service providers. However, there is no integrated plan for managing offenders with a mental illness who come into contact with these agencies. Previous plans to appoint a lead provider of health services across police, corrections and courts did not progress.
Justice Health and DH are now undertaking separate, but coordinated planning for prison mental health and wider mental health services. Justice Health is preparing for an additional 75 mental health beds for men in 2017. This planning comes as indicators of under-capacity within prison and compulsory mental health facilities have been apparent for several years and have now become extreme.
DOJ and DH have arrangements to communicate around mental health at an agency level. In particular, the agencies have well-established communication around mental health through the multi-agency Justice Health Joint Management Committee.
This coordination has helped Justice Health and DH to work closely from the inception of their inter-related planning projects. However, DOJ and DH have not clarified arrangements to ensure that decisions arising from each agency's planning are coordinated and address the current delays for prisoners with a severe mental illness requiring treatment.
Community supervision and prison transition interventions
Managing prisoners with a mental illness after release from prison, or offenders on community corrections orders, is challenging. Yet it can reduce the risk of reoffending. However, it requires the offender to actively engage in treatment or other programs, and for multiple agencies to work together.
There is, however, insufficient coordination of planning among the key agencies to support offenders with a mental illness released from prison. DOJ, DH and DHS operate and plan various support and housing programs. While the agencies are starting to work together, planning is not informed by a consistent framework of objectives, or of analysis of current and future demand.
Corrections Victoria, DH and DHS do not maintain regular agency-level contact around programs for community supervision and transition from prison. Consequently, this increases the risk that the agencies will miss opportunities to improve programs and services for people with a mental illness, or they could be unaware of changes that affect their ability to fulfil their accountabilities. This is particularly the case as Corrections Victoria, DH and DHS are involved in separate reforms that affect programs relevant to people with a mental illness.
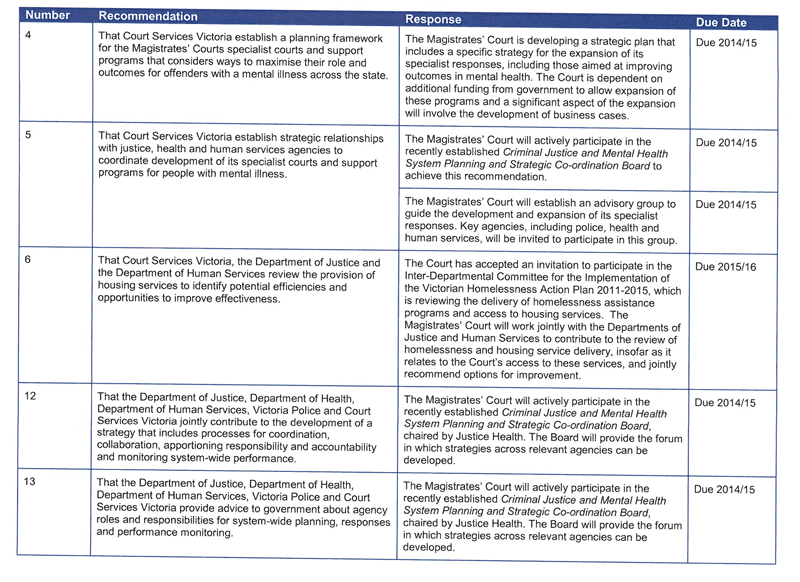
Recommendations
That Victoria Police and the Department of Health:
- enhance bilateral arrangements to improve collaboration and coordination between the two agencies
- improve governance weakness around local service coordination with the aim of improving accountability
- update their joint protocol to reflect recent legislative changes.
That Court Services Victoria:
- establishes a planning framework for the Magistrates' Court's specialist courts and support programs that considers ways to maximise their role and outcomes for offenders with a mental illness across the state
- establishes strategic relationships with justice, health and human services agencies to coordinate development of its specialist courts and support programs for people with a mental illness.
That Court Services Victoria, the Department of Justice and the Department of Human Services:
- review the provision of housing services to identify potential efficiencies and opportunities to improve effectiveness.
That the Department of Justice and the Department of Health:
- prepare a joint plan for mental health facilities inside and outside prisons to guide future funding bids.
That the Department of Justice:
- amends the terms of reference of the Justice Health Joint Management Committee to reflect its role as a forum for agency communication and coordination.
That Victoria Police:
- monitors and reports the time that prisoners with a mental illness are held in police cells before transfer to the prison system.
That the departments of Justice, Health and Human Services:
- establish arrangements to improve coordination, collaboration and planning across the three agencies
- review the range of post-release and community correction programs to identify opportunities for improved effectiveness and efficiency.
The following two recommendations do not appear in the body of the report—they are directed at the criminal justice system as a whole.
That the Department of Justice, Department of Health, Department of Human Services, Victoria Police and Court Services Victoria:
- jointly contribute to the development of a strategy that includes processes for coordination, collaboration, apportioning responsibility and accountability, and monitoring system-wide performance
- provide advice to government about agency roles and responsibilities for system-wide planning, responses and performance monitoring.
Submissions and comments received
We have professionally engaged with the Department of Justice, the Department of Health, the Department of Human Services, Victoria Police and Court Services Victoria throughout the course of the audit. In accordance with section 16(3) of the Audit Act 1994 we provided a copy of this report, or relevant extracts from the report, to those agencies and requested their submissions or comments.
We have considered those views in reaching our audit conclusions and have represented them to the extent relevant and warranted. Their full section 16(3) submissions and comments are included in Appendix B.
1 Background
1.1 Mental illness
Good mental health is one of the foundations of a good life and a healthy society. The World Health Organisation broadly defines mental health as 'a state of wellbeing in which every individual realises his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community'.
Mental illness can disrupt the capacity to plan and perform daily tasks, to maintain relationships, and to lead a fulfilling life. In Victoria, the Mental Health Act 2014 defines mental illness as a 'medical condition that is characterised by a significant disturbance of thought, mood, perception or memory'. Mental illnesses vary widely in nature and severity.
Mental illness can arise when an individual with a genetic predisposition is exposed to environmental factors such as:
- childhood trauma—including physical or sexual abuse
- sustained stress—including from financial problems, or family breakdown
- social isolation, constant negative thoughts or low self-esteem
- adult trauma—including physical or psychological violence
- alcohol and/or drug abuse.
In 2007 the Australian Bureau of Statistics conducted a national survey of mental health and wellbeing using diagnostic screening to establish the incidence of the three most common types of mental illness:
- anxiety disorders, such as panic, post-traumatic stress and obsessive compulsive disorders
- mood disorders such as depression, mania and bipolar disorder
- substance-use disorders, including drug and alcohol dependence.
The survey found that almost 50 per cent of people aged 16 to 85 years will experience one or more of these illnesses in their lifetime, and that 20 per cent—3.2 million people—experienced at least one in the preceding year. Females are more likely than males to have experienced mental illness in the preceding year—22 per cent compared to 18 per cent.
Anxiety disorders affect around 14 per cent of the population, mood disorders around 6 per cent, and substance-use disorders around 5 per cent at any one time. The incidence of co‑existing mental illnesses were also high, with 25 per cent of those suffering one mental illness in the previous year also suffering a second.
The mental state of a person with a mental illness may change over time. A range of factors—including levels of stress and adequacy of medication—may lead to deterioration in mental condition and behaviour. In serious cases symptoms may emerge rapidly, leading to immediate risk of violence, self-harm or suicide. Clinical health services use risk ratings in managing people with a mental illness. Ratings used in the Victorian prison and forensic mental health services are listed in Figure 1A.
Figure 1A
Mental health risk ratings
|
Rating level |
Mental health status |
|---|---|
|
P1 |
Serious psychiatric condition requiring intensive and/or immediate care |
|
P2 |
Significant or ongoing psychiatric condition requiring psychiatric treatment |
|
P3 |
Stable psychiatric condition requiring an appointment or continuing treatment |
|
P4 |
Suspected psychiatric condition requiring assessment |
Source: Victorian Auditor-General's Office from Department of Justice data.
Once diagnosed, there are a variety of treatments available. People are usually treated in the community, although they may also be treated as inpatients either voluntarily or involuntarily. Treatment options include medication, psychological therapy and community support programs.
Fewer than half of those experiencing mental illness access services in any year. While many people recover from mental illness without significant treatment, many serious mental illnesses are undiagnosed and untreated. People with a serious mental illness may not have the ability to access and successfully engage in treatment and rehabilitation without significant support.
1.1.1 Mental illness in the criminal justice system
Many people with a mental illness never commit offences. However, people with certain mental illnesses are more likely than members of the community as a whole to have contact with the criminal justice system. National and international evidence shows that the rate of mental illness amongst people throughout the criminal justice system is much higher than in the community generally.
A 2012 study by the Australian Institute of Health and Welfare found that nearly 40 per cent of people entering prison report having been previously told they had a mental illness—over double the rate in the community. Among prisoners the rates of the major mental illnesses, such as schizophrenia and depression, are between three and five times higher than in the community. In addition, the proportion of prisoners who had been admitted for psychiatric treatment prior to their incarceration—13.5 per cent of male, and 20 per cent of female prisoners—is far higher than for the community generally, where less than 1 per cent of the population is admitted for psychiatric treatment in any year.
People with a mental illness who come into contact with the criminal justice system may take various pathways through the criminal justice and mental health systems, as shown in Figure 1B.
Figure 1B
Pathways for people with a mental illness coming into contact with the criminal justice system
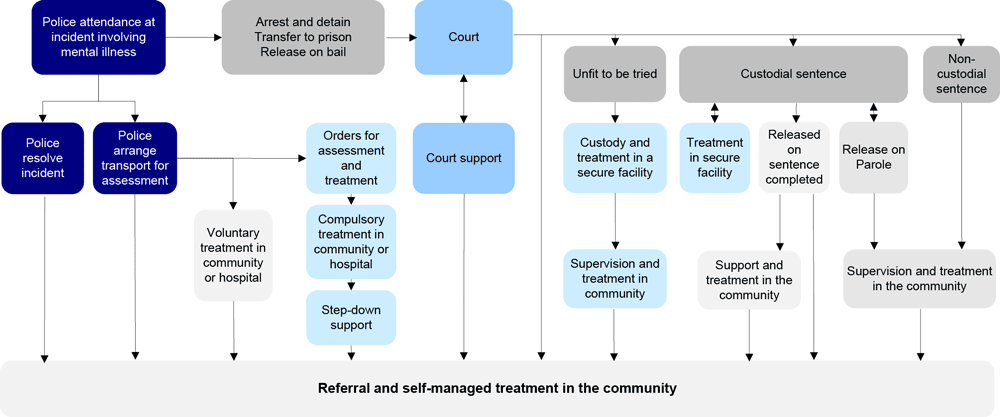
Note: The Mental Health Act 2014 came into force on 1 July 2014 replacing the Mental Health Act 1986.
Non-custodial sentences not involving supervision and treatment in the community are not shown.
Source: Victorian Auditor-General's Office.
Imprisonment represents an opportunity for offenders to receive mental health treatment. A 2012 study found that 27 per cent of prisoners reported their mental health as being 'a lot better' since imprisonment. During imprisonment:
- previously undiagnosed mental illness may be diagnosed
- prisoners' lives are regulated and orderly, and they are removed from detrimental influences in the community
- coexisting health and alcohol and other drug issues can be treated
- there is external motivation to undertake mental health treatment—for example, prisoners are aware that the parole board considers successful completion of mental health treatment in determining early release.
1.1.2 Costs
Mental illness has significant economic and social costs. In 2006, it was estimated to cost the Australian economy $20 billion annually, while the cost to the Victorian economy was estimated to be over $5 billion. These figures include costs related to premature death and disability, the provision of treatment and support services, and reduced productivity and loss of income.
Mental illness also has negative social costs. People living with a mental illness may have difficulty participating in work, maintaining relationships, and retaining stable housing. Their illness may have an impact on their families, friends, carers and the broader community.
The costs to justice and human services agencies of people with a mental illness who are involved with the justice system are particularly high. Research in NSW estimated that the lifetime costs to the state of 11 people living with a mental illness and disability, and having multiple periods of imprisonment, ranged from $0.9 million to $5.5 million per person. Of the $22 million aggregate cost of all 11 people, $14.8 million, or 64 per cent, was incurred directly by justice agencies. In particular, significant resources are required where the justice system is unable to provide non-custodial correction, as the cost of imprisonment is over 10 times that of community-based supervision.
1.2 Victorian mental health strategies
Despite the evidence of mental illness issues affecting many people in contact with the justice system, Victoria does not have a current strategy in this area. Since 2009, three strategies have been developed in relation to mental health. Of those, only one—Victoria's priorities for mental health reform 2013–15—is current. A further mental health strategy is being developed for forensic mental health.
Major strategies for mental health developed since 2009 are shown in Figure 1C.
Figure 1C
Mental health plans since 2009
|
Plan |
Lead agency |
Scope |
Status |
|---|---|---|---|
|
Because Mental Health Matters: Victorian Mental Health Reform Strategy |
Department of Health (DH) |
Mental health system |
Plan of the previous government |
|
Justice Mental Health Strategy, 2010 |
Department of Justice |
Justice system |
Plan of the previous government |
|
Victoria's priorities for mental health reform 2013–15 |
DH |
Mental health system |
Current |
|
Forensic Mental Health Services Planning Project 2014 |
DH |
Mental health facilities and services for people with offending backgrounds |
Planning |
Source: Victorian Auditor-General's Office.
Because Mental Health Matters: Victorian Mental Health Reform Strategy 2009–19 (Reform 2009–19) was the first mental health strategy to set out a whole-of-government and whole-of-community approach to mental health. It recognised that improving clients' experience would require agencies to share responsibility. Reform 2009–19 did not specifically address mental health in the justice system, but did outline the implications of its overarching objectives for justice and housing.
The Justice Mental Health Strategy (Justice Strategy) focused on the justice system, complementing Reform 2009–19. It recognised the shared responsibility of justice, mental health and disability sectors for people with a mental illness involved in the justice system. The Justice Strategy identified objectives, the contributions of justice and non-justice programs to the objectives, and continuing weaknesses for policing, court processes and corrections processes.
The Justice Strategy proposed ideas for future improvements based on extensive consultation, research and evaluations of existing programs. However, future actions were not presented in a framework for achieving its objectives, they were not linked to weaknesses or areas of unmet demand, nor were they prioritised for future funding.
DH prepared Victoria's priorities for mental health reform 2013–15 (Priorities 2013–15) as the government's statement of priorities for reform of the mental health system. Priorities 2013–15 is not based on new analysis or planning, but refines and re-prioritises the directions of Reform 2009–19. While Priorities 2013–15 states that the mental health system should work in a more integrated way with police, courts and corrections, it does not contain any specific proposals for new partnerships to achieve this.
Reform 2009–19, Justice Strategy and Priorities 2013–15 each identify areas for development and highlight the role of agency collaboration in addressing weaknesses in current approaches to people with a mental illness. However, none of the plans present a comprehensive framework for managing and improving pathways through the justice system.
In contrast to earlier plans, DH is taking a wider system view with its current Forensic Mental Health Services Planning Project (FMHSPP), which focuses on mental health services outside prison and police custodial facilities. It highlights pathways between mental health facilities and services inside and outside custodial facilities, and highlights points of inter-reliance of justice functions—police, courts, corrections—and mental health services.
1.3 Criminal justice process and responsibilities
People with a mental illness who are involved in the criminal justice system, and are sentenced to correction, pass through three phases:
- police response and arrest interventions
- courts and court-linked interventions
- police custody and corrections-based interventions.
Justice agencies are responsible for criminal legal processes at each phase. Agencies include Victoria Police, the Magistrates' Court, and the Department of Justice (DOJ) through Corrections Victoria. Justice agencies are also responsible for managing pathways between their areas of responsibility, and for ensuring those pathways effectively support continuity of clinical management, treatment, care and security of people with a mental illness. Court Services Victoria (CSV) supports the operations of the Magistrates' Court.
To meet their responsibilities towards people with a mental illness, justice agencies:
- seek the advice of mental health specialists in making decisions in relation to arresting, sentencing, imprisoning or supervising offenders with, or suspected of having, a mental illness
- draw on mental health services to obtain diagnosis, treatment, care and support services appropriate to the mental health of people within justice agencies' custody or supervision.
Figure 1D lists the justice agencies involved at each phase, and the health organisations and services that justice agencies depend on to effectively manage people with a mental illness.
Figure 1D
Justice agencies, and health and human services organisations
|
Justice agencies |
Health and human services organisations and services |
|
|---|---|---|
|
Police response and arrest interventions |
||
|
Pre-arrest and arrest |
Victoria Police |
Ambulance Victoria General practitioners, public hospitals, area mental health services including Forensic Clinical Specialist Program Mental Health Community Support Services |
|
Pre-sentence custody |
Victoria Police Corrections Victoria |
Victoria Police Custodial Health Service Prison mental health services including Forensicare inpatient and outpatient services |
|
Courts and court-linked interventions |
||
|
Court processes |
Magistrates' Court Magistrates' Court's specialised problem solving courts and mental health programs Victoria Police Community Correctional Services |
Mental Health Court Liaison Service Mental health treatment and rehabilitation services provided under contract to the Magistrates' Court General practitioners, public hospitals, area mental health services including the Forensic Clinical Specialist Program Housing and other support services |
|
Police and corrections custody interventions |
||
|
Police detention |
Victoria Police |
Victoria Police Custodial Health Service |
|
Custodial correction |
Corrections Victoria |
Prison mental health services including Forensicare inpatient and outpatient services |
|
Community supervision and prison transition interventions |
||
|
Non-custodial correction and parole |
Community Correctional Services Adult Parole Board |
General practitioners, public hospitals, area mental health services including the Forensic Clinical Specialist Program Alcohol and other drugs (AOD) treatment services Housing and other support services |
|
Post-release |
Corrections Victoria |
Public hospitals and area mental health services including the Forensic Clinical Specialist Program Forensicare Community Integration Program General practitioners AOD treatment services Housing and other support services |
Source: Victorian Auditor-General's Office.
DH sets priorities and funds mental health services that treat and manage people in contact with the criminal justice system. Mental health services supporting the justice agencies include community-based general practitioners, hospitals, and area mental health services. Justice Health, a DOJ division, is responsible for health services in prisons.
Forensicare is the state's statutory agency for forensic mental health. Forensic mental health services address the needs of people in the criminal justice system with a serious mental illness and a history of offending, or who present a serious risk of such behaviour. Forensicare provides mental health treatment in prisons and in the community, assists courts and area mental health services coordinate the management of forensic patients suffering mental illness, and operates Thomas Embling Hospital.
1.4 Audit scope and objective
The audit objective was to examine the effectiveness of planning and coordination for mental health across Victoria's criminal justice system. To assess this objective, the audit considered whether:
- effective planning guides agency action and coordination
- effective coordination supports agency actions.
The audit examined whether agencies' planning and coordination effectively supports outcomes for people with a mental illness who come into contact with, or are under the control of, the criminal justice system.
It focused on people with a diagnosed mental illness that occurs in isolation or in combination with alcohol and other drug dependency and/or brain injury, and people with undiagnosed conditions whose behaviour or symptoms suggest mental illness and justify assessment as such. The audit did not cover alcohol and drug dependence that is not accompanied by mental illness.
The audit covered people with a mental illness who:
- are involved in incidents attended by police—including offenders, victims and people receiving police assistance or guidance
- are involved in court processes
- are prisoners and offenders subject to non-custodial or parole orders
- were recently released from prison.
Agencies examined as part of the audit included DOJ, DH, Department of Human Services and Victoria Police. Each agency is responsible for statewide activities that affect people with a mental illness, planning for the effective use of significant resources, and effective coordination of services that are closely related to those of other agencies. Within DOJ, the audit covered Justice Health and Corrections Victoria.
The audit did not specifically examine the performance of CSV, as it was created on 1 July 2014. The audit did examine the role of DOJ in providing administrative and program management services to the Magistrates' Court for the period leading up to the creation of CSV, and made recommendations targeted at CSV for future action.
As required under section 16F of the Audit Act 1994, the Auditor-General has provided written information about the audit to Court Services Victoria to enable it to respond to the audit report and recommendations and, as also required, the Auditor-General has written to the Premier to notify him of this.
1.5 Audit method and cost
The audit involved:
- desktop research
- consultation with both agencies and stakeholders
- quantitative evaluation of data provided by agencies
- qualitative evaluation against best-practice principles.
The audit was performed in accordance with the Australian Auditing and Assurance Standards. Pursuant to section 20(3) of the Audit Act 1994, unless otherwise indicated, any persons named in this report are not the subject of adverse comment or opinion.
The total cost of the audit was $450 000.
1.6 Structure of the report
The report is structured in a way that represents the potential journey through the criminal justice system for a person with a mental illness. The parts are as follows:
- Part 2 discusses police interventions.
- Part 3 discusses courts and court-linked interventions.
- Part 4 discusses police custody and prisons-based interventions.
- Part 5 discusses community supervision and prison-transition interventions.
2 Police
At a glance
Background
People with a mental illness in the community come to the attention of police as a result of offending, behaviour suggestive of mental disorder, or the effects of alcohol or drugs. Victoria Police is responsible for managing such incidents, and referring people with a mental illness to health services. Emergency services liaison committees enable local police and mental health services coordination.
Conclusion
Victoria Police and the Department of Health (DH) do not have a joint plan to strategically improve the responses of police and mental health services to people with a mental illness. However, the agencies are now working towards improving collaboration between police and mental health services.
Findings
- In 2013–14 police responded to over 8500 incidents related to mental illness.
- Joint planning between Victoria Police and DH has not been effective but is starting to improve.
- Victoria Police and DH are reforming their practices around dealing with people with a mental illness to improve outcomes.
- Longstanding arrangements support local coordination and communication of police and mental health services, although more needs to be done to address variability in effectiveness of local communication and coordination.
Recommendations
That Victoria Police and the Department of Health:
- enhance bilateral arrangements to improve collaboration and coordination between the two agencies
- improve governance weaknesses around local service coordination with the aim of improving accountability
- update their joint protocol to reflect recent legislative changes.
2.1 Introduction
People with a mental illness in the community come to the attention of police as a result of offending, personal crisis or behaviour suggestive of mental disorder, or the effects of alcohol and other drugs. Victoria Police is responsible for managing such incidents.
If there is an arrest, the offender may be charged and held in police custody before being brought before the Magistrates' Court.
When police are satisfied that a person appears to have mental illness, and there is risk of suicide or harm to others, police may apprehend the person under section 351 of the Mental Health Act 2014 (the Act). The Act requires that police arrange for the person to be taken for examination, typically at public hospital emergency departments. Based on the examination, the person may be discharged to the community, or be required to undergo psychiatric assessment, and possible treatment in a hospital or in the community.
Police also carry responsibility for a large number of cases where there is neither offending, nor grounds for action under the Act. In these cases, police may seek to calm the situation, and to refer the individual to an appropriate service.
2.2 Conclusion
Victoria Police and the Department of Health (DH) each have responsibilities for addressing mental health issues. The inter-dependencies of the two agencies means that effective collaboration, coordination and planning is essential to maximise the impact of their response outcomes for people with a mental illness.
While each agency has a range of mechanisms to respond to people with a mental illness, the agencies do not effectively collaborate, coordinate and plan. This has been an historical weakness in the relationship between the two agencies. However, more positively, DH and Victoria Police are now working to maximise the outcomes for those experiencing mental health issues who come into contact with police.
2.3 Police and trends in mental illness
In 2013–14, Victoria Police attended over 8 500 incidents that involved suspected or actual mental illness. Of these 78 per cent required transfer of an individual to a hospital emergency department. The number of incidents in 2013–14 was more than three times that in 2009–10. This is shown in Figure 2A.
Victoria Police estimates the median time required to respond and, where necessary, transfer the person to a hospital, is two hours. For 2013–14 this corresponds to 16 361 hours, or 2 045 shifts, of police response capacity.
Figure 2A
Police responses to mental health incidents
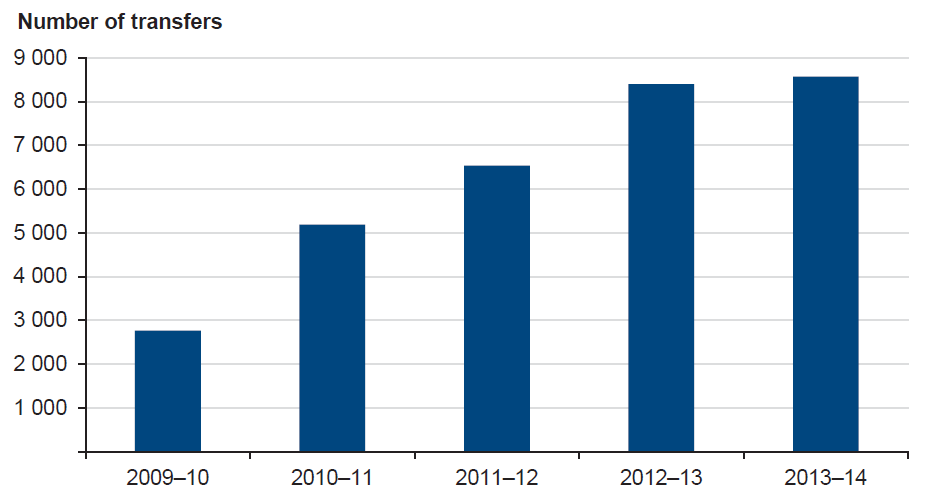
Source: Victorian Auditor-General's Office from Victoria Police data.
Figure 2B illustrates the role of Victoria Police and the police mental health collaborative service—Mental Health and Police response (MHaP)—in responding to people with a mental illness. The case study combines the experience of more than one person.
Figure 2B
Police involvement in mental illness
|
Ms G is a 63-year-old whose history of mental illness dates back to 1999 when she was admitted to a mental health service inpatient unit diagnosed with delusional disorder. She had further contacts with the mental health service in 2002 and 2004 when she was diagnosed with paranoid personality disorder. Admissions followed in 2006 and again in 2009, when Ms G was diagnosed with delusional disorder and schizophrenia. Ms G came to the attention of police in August 2009 after a series of complaints from her neighbour and from the public housing service, which owned both units. Ms G had also been making regular complaints to police about her neighbour, in writing and in person at the local police station. Unaware of her psychiatric history, police saw Ms G as a vexatious complainant, and one of a number of local 'characters'. However, as Ms G's complaints continued, police referred her case to the MHaP unit attached to the local mental health service. The MHaP team was able to bring together her history of contact with police and with mental health services. The team identified a pattern of behaviour consistent with ongoing psychotic illness. The MHaP visited Ms G's unit a number of times, but attempts to assess Ms G were difficult as she generally refused to leave the premises. Ms G then could not be contacted at all. Police attended her unit and found there were no lights on and the neighbour reported no sound. They referred the matter back to MHaP. After several unsuccessful visits, the MHaP team decided that Ms G was most probably still in the house as her hospital file contained no references to relatives or friends. Police and the MHaP team decided police would enter the house, by force if necessary, because there was a strong probability that Ms G was not caring for herself. Upon entering the unit, police found Ms G hiding. She had no fresh food. The house smelled offensive as Ms G had not flushed the toilet, for fear of making any noise. An ambulance took Ms G to hospital where she was admitted under the Mental Health Act 1986 and placed on anti-psychotic medication. After several weeks of treatment, she was allowed to go home, but placed on a supervised order requiring she undergo ongoing treatment. Ms G has contacted police only once following her discharge, requesting the return of a brooch that she alleged was taken when she was arrested. She reluctantly attends outpatient appointments with her case manager and receives her injection fortnightly. Her paranoid delusions have not resolved but are significantly diminished and her neighbour has made no further complaints. The housing service has not proceeded with its threatened foreclosure of Ms G's tenancy. |
Note: Details have been changed to protect confidentiality.
Source: Victorian Auditor-General's Office from Victoria Police data.
2.4 Planning and agency-level coordination
The nature of Victoria Police's role in dealing with people with a suspected or actual mental illness means that it is routinely involved with the health system, hospitals and DH. As such, both it and DH need to effectively collaborate and plan to maximise outcomes for people with a mental illness.
Victoria Police and DH are working towards a joint plan to develop the effectiveness of responses to mental illness requiring collaborative action of police and mental health services. Until recently the agencies have focused planning in their own areas of responsibility, limiting collaboration and coordination.
However, reforms occurring in each agency now place Victoria Police and DH in a position to strategically address collaborative operating relationships. This has the potential to improve outcomes for people with a mental illness, whose interaction with mental health services results from their contact with police.
2.4.1 Planning and initiatives
In 2006 Victoria Police nominated mental health as a priority issue, examining operating practices of police, and using the results to develop a mental health strategy—Peace of Mind— which supported development of emerging local models for collaboration between police and mental health services.
Victoria Police also undertook a number of research projects including Police Responses to the Interface with Mental Disorder (PRIMeD), which comprehensively examined policing of people with a mental illness. PRIMeD showed that mental illness is now part of everyday police business, and should be integrated into all aspects of police development, training and community engagement.
DH has undertaken planning and reform over a similar period. Because Mental Health Matters: Victorian Mental Health Reform Strategy 2009–19 identified the need for a range of improvements to mental health services and their links with emergency services and the justice system. DH has completed some of these reforms, and undertaken more concrete planning for others in its current Forensic Mental Health Services Planning Project. In addition, DH has implemented the Act, which provides for greater patient involvement in treatment and care decisions, and requires the least restriction be placed on patients consistent with their safety.
With these internal reforms, Victoria Police and DH are now in a position to jointly plan their collaborative service models, and to address areas of inter-agency risk. Victoria Police remains concerned about the demand on police resources arising from incidents involving suspected or actual mental illness, and the need for collaborative mental health service models that effectively engage people with a mental illness in treatment and recovery, and reduce crises that demand police responses.
In addition, DH wishes to ensure that demand on hospital emergency departments and mental health inpatient facilities, as well as use of restrictive interventions, are effectively managed. As Victoria Police may arrange for the transport of people with an actual or suspected mental illness for assessment at a hospital under section 351 of the Mental Health Act 2014, DH is concerned to ensure that this provision of the Act is used effectively.
Victoria Police and DH are now taking action to address these issues:
- Victoria Police and DH are collaborating to implement LEDR Mark2, a new system that incorporates a function enabling police to refer people with a mental illness to services in the community. This approach recognises the need for consistency between Victoria Police's operating support, and the mental health system's triage and intake arrangements. The collaboration will also allow services to disseminate better practice across all health regions.
- Victoria Police and DH were successful in their bid for funds to extend the Mental Health and Police Response service to all 21 health regions. The development of models for joint police and mental health responses to people with an acute mental illness, that addressed the needs of both agencies, resulted from long‑term collaboration between DH and Victoria Police.
2.4.2 Agency-level collaboration and coordination
The level of inter-dependence between Victoria Police and mental health services requires effective collaboration and coordination. Although both agencies have been engaging around mental illness since 2006, they have found it difficult to resolve issues and strategically collaborate. However, since 2012 Victoria Police and DH have taken steps to strengthen their strategic engagement. The two agencies are working towards an agreed framework to oversee and address areas of inter-dependence.
From 2006 to 2011 the agencies engaged through an inter-departmental liaison committee (IDLC) which focused on strategic issues, such as system development and service coordination. The IDLC had a diverse membership to gain a broad perspective on mental health issues. However, it tended to focus on policing issues, thus limiting its strategic effectiveness.
Current arrangements for communication between Victoria Police and DH show they intend to develop a more effective and strategic relationship. The Chief Commissioner of Police and Secretary of DH met in 2012 and 2013 to discuss matters affecting the two portfolios, including mental health. In 2013 Victoria Police and DH also established a new IDLC jointly chaired by an Assistant Commissioner of Victoria Police, and a Deputy Secretary of DH with responsibility for mental health.
Each has the authority to represent their agency heads, to address strategic issues, progress work within their respective agencies, and handle matters for decision. The IDLC is focused on matters of strategic interest to the two agencies, including management of people with a mental illness in mental health services, or coming into contact with police. The IDLC has met regularly since its formation in June 2013.
Through the IDLC the agencies have adopted the joint objective to improve joint long-term planning and opportunities for service system development by enhancing communication between emergency services and health systems, developing cross-organisational knowledge and understanding and strengthening relationships.
The IDLC objective reflects the characteristics of successful joined-up working—leadership, shared goals and strategies, and a commitment to understanding partners' constraints and cultures.
A key outcome will be the development and implementation of a joint plan to guide strategic and operational partnerships, and resource commitments. In light of their historical challenges, the adoption of a joint plan and progress towards its implementation will be required to determine whether the agencies' joint working is soundly based and effective.
2.5 Program and service-level coordination
Effective coordination has a significant impact both on the quality of outcomes for people with a mental illness coming into contact with police, and on the effective use of high-cost facilities such as hospital emergency departments.
Victoria Police and DH have long-standing mechanisms for supporting local communication and coordination between police, ambulance, area mental health services (AMHS) and hospital emergency departments. However, Victoria Police and DH will require continued attention to ensure emergency services liaison committees (ESLC) are effectively maintaining local coordination.
Operational communication and coordination for mental health is formally supported by 21 local ESLCs involving police, AMHS, ambulance and hospital emergency departments. ESLCs were established in 2004 under the Department of Health and Victoria Police Protocol for Mental Health (the Protocol). The Protocol governs interactions between police, ambulance and mental health services where incidents warrant police action under the Act. The role of the ESLCs includes establishing local protocols consistent with the Protocol, and addressing operational service issues.
In addition, the IDLC is providing the basis for DH and Victoria Police to address AMHS' difficulties in gaining consistent police responses to violent incidents involving patients with a mental illness in AMHS facilities. However, the IDLC's role does not provide for monitoring or oversight of local services' performance in responding to incidents involving mental illness involving police in the community.
The IDLC does not have lines of authority to local services. In addition, while Victoria Police may direct local Police commands, DH does not direct health services, which are independent entities under Victoria's devolved health system. The IDLC relies on minutes of ESLC's meetings, and direct communication with local representatives to monitor effectiveness of local coordination. However, it does not receive data from Victoria Police on police incidents involving mental illness.
The recent extension of funding for joint police and mental health response to all 21 health regions creates the imperative for Victoria Police and DH to introduce a framework for performance monitoring and reporting that enables them to ensure:
- police, hospitals and emergency departments are more effectively responding to people with a mental illness
- people with a mental illness assisted by police experience more effective, least restrictive responses.
Victoria Police and DH have not completed the update of their joint protocol to reflect changes arising from the new Mental Health Act 2014. DH has undertaken consultation and communication in preparation for the new Act since 2011. Victoria Police and DH are currently in consultation to clarify application of the Act to service delivery arrangements.
Recommendations
That Victoria Police and the Department of Health:
- enhance bilateral arrangements to improve collaboration and coordination between the two agencies
- improve governance weakness around local service coordination with the aim of improving accountability
- update their joint protocol to reflect recent legislative changes.
3 Courts
At a glance
Background
The Magistrates' Court of Victoria (Magistrates' Court) has specialist courts and programs to divert to treatment people whose mental illness, cognitive impairment or substance use contributes to their offending. On 1 July 2014 administration and program management resources of the Magistrates' Court were transferred from the Department of Justice (DOJ) to Court Services Victoria (CSV).
Conclusion
There is no current plan guiding development of the Magistrates' Court's specialist courts and support programs for people with a mental illness. While the Magistrates' Court maintains effective program-level coordination, it does not have strategic agency communication commensurate with its role in supporting, managing and diverting offenders with a mental illness to treatment.
Findings
- NSW research indicates approximately half of the cases coming before the NSW Magistrates' Courts are likely to involve defendants with a mental illness.
- The Magistrates' Court has developed specialist courts and court support programs to assist people with a mental illness since 2002.
- There is no current framework describing the role the Magistrates' Court's specialist courts and support programs could play if they were extended to operate more widely across the Magistrates' Court's 12 major regions.
Recommendations
- That CSV establishes a planning framework for the Magistrates' Court's specialist courts and support programs that considers ways to maximise their role and outcomes for offenders with a mental illness across the state.
- That CSV establishes strategic relationships with justice, health and human services agencies to coordinate development of its specialist courts and support programs for people with a mental illness.
- That CSV, the Department of Justice and the Department of Human Services review the provision of housing services to identify potential efficiencies and opportunities to improve effectiveness.
3.1 Introduction
The Magistrates' Court of Victoria (Magistrates' Court) hears criminal charges brought by police, makes findings in relation to guilt and makes sentencing orders. A court may obtain mental health assessments as part of its consideration of criminal cases, in particular where an accused's mental illness may satisfy the criteria of the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997.
Forensicare has statutory responsibility for mental health services for people with a serious mental illness and offending histories. As part of these responsibilities, Forensicare provides the Magistrates' Court with pre-sentence court reports, and reports to the Office for Public Prosecutions on eligibility of defences under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997. In determining a sentence, the court may consider advice that Community Correctional Services provides to determine the person's suitability for a community corrections order (CCO), and the conditions of the CCO.
The Magistrates' Court has specialised courts and support programs for people whose mental illness, cognitive impairment or substance use contributed to their offending. Accused persons may access support programs during their bail or remand period. Specialist court procedures and sentencing arrangements provide for offenders to engage with treatment and support under supervision of a magistrate over four to 24 months. Such engagement is not possible within the court's normal procedures.
The Assessment and Referral Court (ARC) List and Drug Court were introduced through amendment to the Magistrates' Court Act 1989. They use the authority of the court together with mental health and addiction assessment and treatment to give people an opportunity to take responsibility for their offending, and to address the personal issues that led them to offend.
The Magistrates' Court support programs provide services to help accused people address the causes of their offending. The support programs are the Court Integrated Services Program (CISP), CISP Remand Outreach Program, and Court Referral and Evaluation for Drug Intervention and Treatment/Bail Support program (CREDIT/Bail).
Until 30 June 2014, the Department of Justice (DOJ) provided administrative and operating support, and policy, program development and program management functions for the Magistrates' Court. With the creation of Court Services Victoria (CSV) on 1 July 2014, administrative and operating support, and program management functions were transferred from DOJ to CSV. Legislative policy remains with DOJ, and the program development continues to be jointly undertaken by DOJ and CSV.
3.2 Conclusion
The Magistrates' Court in conjunction with DOJ has successfully developed specialist courts and support programs to divert offenders with a mental illness to treatment, and address the causes of their offending. The specialist courts and support programs play a key role by reducing rates of imprisonment. However, the Magistrates' Court does not have a current plan for their future development. With the recent establishment of CSV, effort is required to develop the coordination with justice, health and human services agencies required to support development of the Magistrates' Courts initiatives for mental illness.
3.3 Courts and trends in mental illness
The Magistrates' Court does not record the role played by mental illness in offending for all criminal cases. However, a New South Wales study found that approximately 55 per cent of defendants in that state's magistrates' courts had a mental illness. While not directly comparable, this suggests that a similar proportion of cases initiated in the Victorian Magistrates' Court in 2012–13 potentially involved people with some form of mental illness.
Figure 3A shows the number of people accepted for the Magistrates' Court specialist mental health list, the ARC List, and support programs CISP and CREDIT/Bail for 2009–10 to 2013–14.
People accepted to the ARC List generally have a mental illness or mental impairment and history of offending. Offenders regularly appear before a magistrate in informal meetings to monitor their progress. Offenders receive support and treatment throughout their time on the ARC List.
CREDIT/Bail provides support and accommodation to increase the likelihood of accused persons with substance abuse issues, and other needs being granted bail. CISP provides similar assistance for accused people with a range of needs, including mental illness, before they are sentenced.
Figure 3A
Clients accepted to the Magistrates' Court's main programs for people with drug and alcohol issues, a mental illness and other needs
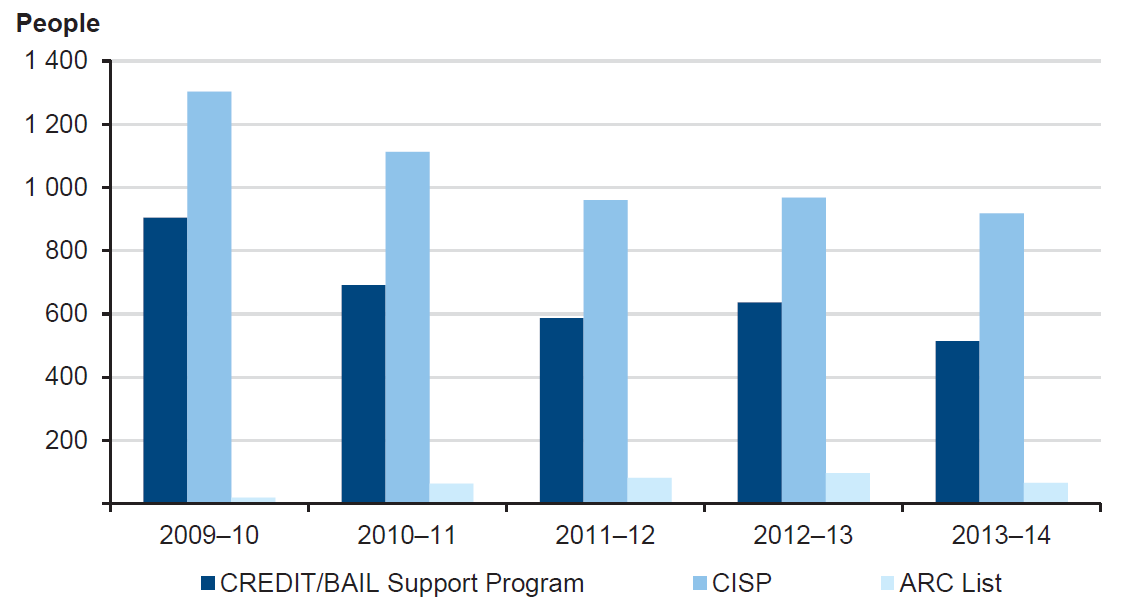
Note: ARC List commenced operating in 2010.
Source: Victorian Auditor-General's Office from Magistrates' Court of Victoria data.
Of the Magistrates' Court's programs, CISP provides the largest number of support places for people with a mental illness and other needs. Of the 2 044 cases referred to CISP in 2012–13, substance abuse and mental health issues were the two most common reasons for referral—with 669 referrals for mental health support.
The number of clients accepted to CISP and CREDIT/Bail has declined over the period 2009–10 to 2013–14. A steady increase in the complexity of cases means the Magistrates' Court must devote more time to achieve outcomes for each client. With steady staff numbers, this limits the number of cases the court programs can accept.
Figure 3B shows the availability of specialist courts and support programs across the Magistrates' Court's 12 regions. As part of a 12-month trial, the Magistrates' Court also provides CISP in four prisons—Dame Phyllis Frost Centre, Metropolitan Remand Centre, Melbourne Assessment Prison and Port Phillip Prison.
Figure 3B
Magistrates' Court's specialist courts and support programs relevant to people with a mental illness
|
Court region |
Program |
|---|---|
|
Barwon South West |
CREDIT/Bail (Geelong) |
|
Broadmeadows |
CREDIT/Bail (Broadmeadows) |
|
Dandenong |
CREDIT/Bail (Dandenong) |
|
Frankston |
CREDIT/Bail (Moorabbin, Frankston) |
|
Gippsland |
CISP (Latrobe) |
|
Grampians |
CREDIT/Bail (Ballarat) |
|
Heidelberg |
CREDIT/Bail (Heidelberg) |
|
Hume |
|
|
Loddon-Mallee |
|
|
Melbourne |
CISP (Melbourne) |
|
Ringwood |
CREDIT/Bail (Ringwood) |
|
Sunshine |
CISP (Sunshine) |
Source: Victorian Auditor-General's Office from Magistrates' Court data.
Figure 3C illustrates how the ARC List assists people with a mental illness to address the causes of their offending. The case combines the experience of more than one person.
Figure 3C
Assessment and Referral Court List
|
Ms M is a 32-year-old woman who lives alone. She has a fractured relationship with her family, and is currently single, although reports having a same-sex partner irregularly for some years. Ms M makes her main social connections on the internet. Ms M reported excessive drinking from the age of 15. She has continued to abuse alcohol, as well as a variety of drugs including heroin and cannabis, for most of her adult life. She had her first admission to an adolescent mental health facility when she was 15. Ms M has multiple diagnoses including borderline personality disorder, obsessive compulsive disorder, substance-use disorder and an acquired brain injury. Ms M has a criminal history dating back to her adolescence, with most of her charges being minor assaults. Ms M's current charges included hindering police, assaulting police on duty, unlawful assault, intentionally causing injury, and recklessly causing injury. Ms M's legal representative referred her to the ARC List due to her history of offending, ongoing substance use, and her limited sources of social support. Upon being accepted to the ARC List, a case manager organised a meeting to plan for Ms M's time under supervision of the ARC List Magistrate. Ms M, her case manager, representatives from an area mental health service, Victoria Police, hospital staff and the Office of the Public Advocate attended. The outcomes of the meeting were that the area mental health service would develop a treatment plan in consultation with Ms M's GP, Victoria Police would develop a response plan and Ms M's ARC List case manager would refer Ms M to treatment specialists. Ms M was involved in deciding on the arrangements. The ARC List requires offenders to appear before the magistrate each month accompanied by their case manager. Police also attend the meetings. At each meeting, the magistrate asked Ms M to talk about her progress, and to explain any occasions where she had not complied with her treatment plan, offended or come into contact with police. While initially defensive and aggressive, Ms M gradually became more confident, admitting mistakes and volunteering information about her successes. Over her 12 months on the ARC List, Ms M completed drug and alcohol treatment, regularly met her case manager from the area mental health service, and significantly reduced her contact with the local police. By the end of her time on the ARC List, Ms M felt she understood herself better, and was able to take more responsibility for her actions. Ms M also had a plan to help her cope better when she experienced a crisis. After 12 months Ms M had successfully completed the requirements of the ARC List . |
Note: Details have been changed to protect confidentiality.
Source: Victorian Auditor-General's Office from Magistrates' Court data.
3.4 Planning and agency-level coordination
There is no current plan guiding development of the Magistrates' Court's specialist courts and support programs for people with a mental illness. While the Magistrates' Court maintains effective program-level coordination, it does not have agency-level communication commensurate with its role in supporting, managing, and diverting to treatment offenders with a mental illness.
Between 2002 and June 2014, DOJ provided policy, project and program management support to assist the Magistrates' Court develop specialised problem-solving courts, support programs and services. The specialist courts and support programs aim to divert offenders from prison into treatment and recovery, and to reduce the reoffending risk of people with a mental illness or substantial Alcohol and other Drug (AOD) dependency.
Figure 3D shows Magistrates' Court's specialist courts and support programs for people with a mental illness, their locations and stage of development.
Figure 3D
Development of specialised courts and programs for mental health in the Magistrates' Court
|
Program |
Locations |
Stage of development |
|---|---|---|
|
Drug Court |
One Magistrates' Court (Dandenong) |
Established 2002 |
|
CREDIT/Bail Support |
Eight Magistrates' Courts (refer to Figure 3B) |
Established 2004 |
|
CISP |
Three Magistrates' Courts (refer to Figure 3B) |
Established 2006 |
|
ARC List |
One Magistrates' Court (Melbourne) |
Established 2010 |
|
CISP Remand Outreach Program |
Dame Phyllis Frost Centre |
Established as 12-month pilot in 2014 |
Note: The Department of Health funds the Mental Health Court Liaison Service at six metropolitan courts, and CSV at one metropolitan court. CISP evaluation undertaken over 2007–08.
Source: Victorian Auditor-General's Office from Magistrates' Court of Victoria data.
There is no current framework describing the role these initiatives could play if they were extended from their current, pilot locations to operate more widely across the Magistrates' Court's 12 major regions.
DOJ developed plans for the Magistrates' Court in 2010 and 2011 that proposed options for expanding the specialist courts and support programs beyond their limited locations, in line with need in the community. The 2010 business case, Next Generation Courts, was not submitted for consideration as part of the annual State Budget. Next Generation Courts proposed to expand the Magistrates' Court's specialist courts and support programs to address crime arising from disadvantage broadly, rather than mental health in particular. The business case showed economic benefits in reduced reoffending and increased offender compliance with orders resulting in reduced court, policing and prison costs. A more limited version of the business case led to ongoing funding for the Courts Integrated Services Program at three sites.
The 2011 strategic plan Integrating Courts Programs Framework (ICPF) proposed a framework for extending the specialist courts and support programs. While based on extensive planning and consultation, the ICPF did not comprehensively outline the inter-dependency between courts, other justice agencies and mental health services, or the role of forensic mental health services such as the Mental Health Court Liaison Service (MHCLS), in improving the Magistrates' Court's operations. ICPF did not become a plan of the government or an ongoing plan of the Magistrates' Court.
As a result, there is no current statement of the potential role of the Magistrates' Court in diverting offenders with a mental illness from custodial correction into treatment and support, reducing their reoffending, and reducing demand on police, courts and correctional services. Such a plan would establish whether the specialist courts and support programs and the links with mental health and other services required for effective outcomes should have a role across all Magistrates' Courts'.
The need for a fully developed plan for the Magistrates' Court and its role in the wider justice system was recently highlighted when the government's Budget and Expenditure Review Committee (BERC) requested that the Minister for Corrections and Attorney-General provide options for reducing demand on prison capacity. Initial advice to BERC showed that the government was considering the Magistrates' Court's CISP program as a key mechanism for reducing imprisonment and demand on prisons.
3.4.1 Agency-level communication and coordination
CSV—now responsible for providing administrative and operating support for the Magistrates' Court—does not have arrangements for agency-level communication commensurate with the central role of its specialist courts and support programs in supporting, managing, and diverting offenders with a mental illness to treatment.
Prior to the establishment of CSV in July 2014, DOJ provided policy, project and program management support, and led inter-agency communication. DOJ's support enabled development of Magistrates' Courts' specialist courts and support programs for mental illness. Of functions previously within DOJ, only the Magistrates' Court's administration and operating support, and program management transferred to CSV. DOJ and CSV will now undertake program development jointly.
However, there is no agency-level forum in which DOJ, CSV, Victoria Police, DH and the Department of Human Services (DHS) are able to discuss strategic issues around reducing offending and improving recovery of people with a mental illness in the criminal justice system.
The Magistrates' Court's broader role is evident in its commitment to specialist courts and support programs for diverting people with a mental illness into treatment and recovery. These are reliant on the programs and services of other agencies including AOD and mental health treatment services, and housing services required for offenders who participate in CISP, ARC List or Drug Court programs.
An agency-level forum would consider, develop and monitor models for diverting people with a mental illness into treatment and recovery, and the collaborative service relationships between police, the Magistrates' Court, mental health and other services required to achieve this.
The Magistrates' Court has in the past established groups to consider development of its specialist courts and support programs, and their role in reducing reoffending. For example, the Mainstreaming Working Group was formed in 2011 to advise the Attorney-General on, among other things, options for adopting the Magistrates' Court's specialist courts and support programs more broadly. The group included members of the judiciary, court administrators and representatives of DOJ.
A more senior committee—the Criminal Justice System Steering Committee—brings together judicial leaders of all criminal jurisdictions, including the Magistrates' Court, with the Secretary of DOJ and representatives of Victoria Police and other relevant agencies. While the committee considers all aspects of the criminal justice system, over the period 2009 to 2013 it discussed mental health on only one occasion.
DOJ provided support to the Magistrates' Court in developing the Drug Court, CISP, and the ARC List, and in planning Next Generation Courts and ICPF. With the formation of CSV, DOJ and the Magistrates' Court have not yet clarified how these functions will occur.
3.5 Program and service-level coordination
3.5.1 Specialist courts and support programs
The Magistrates' Court maintains effective program-level communication and coordination for the operation of its specialist courts and support programs.
The Magistrates' Court's specialist courts and support programs—the ARC List, Drug Court, CISP and CREDIT/Bail—each have effective program-level mechanisms to communicate and coordinate with justice agencies. These are listed in Figure 3E.
Figure 3E
Program-level coordination of Magistrates' Court's specialist courts and support programs
|
Coordination group |
Role |
Membership |
|---|---|---|
|
ARC List Management Committee |
Oversees development of the ARC List and service model, manages communication with stakeholders |
Magistrates, DOJ Courts Policy |
|
ARC List Court Processes Working Group |
Coordinates ARC List operations |
Magistrates, DOJ Courts Policy, Victoria Police, Victorian Legal Aid, mental health organisations |
|
Drug Court team meeting |
Coordinates Drug Court Services |
Drug Court Program, Corrections Victoria, Victoria Police, housing services |
|
CISP Monitoring Committee |
CISP and CREDIT/Bail Support program monitoring and coordination |
Magistrates, CISP Program, DOJ, Koori representative |
Source: Victorian Auditor-General's Office.
Services and coordination required by the ARC List, Drug Court and support programs CISP and CREDIT/Bail, are secured through memoranda of understanding. The Magistrates' Court has memoranda of understanding with:
- Victoria Police for police prosecutors located with the ARC List and Drug Court
- DH for drug treatment services at the Drug Court, and for CISP and CREDIT/Bail
- DHS to secure transitional housing and support services used by Drug Court, CISP, and CREDIT/Bail clients.
The Magistrates' Court is strengthening its management of the range of service providers to its specialist courts and support programs.
The Magistrates' Court reports that it engages up to 100 general practitioners at any time. Many of the Magistrates' Court's clients with a mental illness have a history of offending, and may have complex needs including AOD dependency and cognitive impairment. Effective management of these clients may require clinicians with relevant expertise and an interest in clients whose mental illness is associated with offending. Some health services and general practitioners' are unwilling to accept forensic clients with a mental illness who may exhibit difficult behaviours.
The Magistrates' Court experiences challenges in managing transitional housing for clients of its specialist courts and support programs. Stable, safe accommodation is required if people with a mental illness, or other significant needs, are to successfully engage with treatment or support programs.
The Magistrates' Court commits funds to secure the availability of 80 properties, which are used to provide transitional accommodation for Drug Court, CISP and CREDIT/Bail clients, some of whom require accommodation at short notice. However, the property management model has resulted in tenants staying beyond the term for transitional support, leading to insufficient places being available for new clients.
The Magistrates' Court meets regularly with DHS, housing service providers, and Corrections Victoria, which is currently undertaking planning for housing of released prisoners. While the housing programs of the Magistrates' Court and Corrections Victoria address the needs of similar clients, the Magistrates' Court and Corrections Victoria are not coordinating their planning. The absence of such coordination means it is unlikely that the agencies will be in a position to identify any opportunities for jointly improving their housing services.
3.5.2 Liaison with mental health services
Arrangements for the MHCLS do not adequately reflect its role in operation of the Magistrates' Courts.
DH directly funds most of the MHCLS, with the service at one metropolitan court being funded by CSV under agreement with DH. MHCLS places Forensicare's mental health clinicians in seven Magistrates' Courts to facilitate the referral of people with a mental illness appearing before the courts to mental health services. MHCLS clinicians identify people with a mental illness nearing their court dates, obtain mental health histories, prepare care plans, and conduct mental health assessments to ensure that accused people with a mental illness are able to appear before the court.
Courts note that the MHCLS is valuable and effective. An effectively operating MHCLS, such as the service at Dandenong Magistrates' Court, can significantly reduce the need for specialised psychiatric reports, and consequent delays to court proceedings. MHCLS clinicians can play a central role in liaising with area mental health services, prison health services, and Thomas Embling Hospital to manage accused people with a mental illness.
While under consideration, DH's Forensic Mental Health Services Planning Project includes a draft recommendation to significantly increase availability of MHCLS across the Magistrates' Court's metropolitan locations, subject to an evaluation. MHCLS is also available in some non-metropolitan areas. Consistent with this, DH notes that the MHCLS positions are to be reviewed. DH should work with CSV and DOJ to ensure the clinical role of MHCLS—together with its impact on the Magistrates' Court's operations, and links with other parts of the mental health and justice systems—are recognised in future arrangements.
Recommendations
That Court Services Victoria:
- establishes a planning framework for the Magistrates' Court's specialist courts and support programs that considers ways to maximise their role and outcomes for offenders with a mental illness across the state
- establishes strategic relationships with justice, health and human services agencies to coordinate development of its specialist courts and support programs for people with a mental illness.
That Court Services Victoria, the Department of Justice and the Department of Human Services:
- review the provision of housing services to identify potential efficiencies and opportunities to improve effectiveness.
4 Custody
At a glance
Background
Victoria Police holds in custody people who are arrested and charged until their release on bail, or their transfer to prison. Imprisoned people with a mental illness receive voluntary treatment within prisons. Prisoners may only receive compulsory treatment outside prisons under custody of the Secretary of the Department of Health (DH).
Conclusion
Victoria Police, the Department of Justice (DOJ) and DH are responsible for mental health services for people with a mental illness held in custody, but are not guided by a current plan. Effective collaboration of DOJ and DH is supporting the discussions on future investment in mental health facilities and services inside and outside prisons. Victoria Police has improved health services for people held in police custody.
Findings
- Mental health beds in prisons and Thomas Embling Hospital have not kept pace with the number of prisoners requiring treatment, and waiting times have increased very significantly.
- There is no current plan integrating mental health across police cells, prisons, and mental health facilities and services for people with offending backgrounds in the community.
- DOJ and DH have not clarified how they will coordinate decisions to address delays in prisoners accessing compulsory mental health treatment.
- Victoria Police does not centrally report the time people with a mental illness in its custody are held before transfer to prison.
Recommendations
- That DOJ and DH prepare a joint plan for mental health facilities inside and outside prisons to guide future funding bids.
- That DOJ amends the terms of the Justice Health Joint Management Committee to reflect its role as a forum for agency communication and coordination.
- That Victoria Police monitors and reports the time that prisoners with a mental illness are held in police cells before transfer to the prison system.
4.1 Introduction
Victoria Police holds in custody people who are charged and arrested until they are transferred to the prison system, or released on bail. Individuals may also be transferred from the prison system to police cells to attend court. When detained in police cells, individuals are in the legal custody of the Chief Commissioner of Police and Victoria Police provides health services as part of its custodial responsibility.
Once transferred to the prison system, prisoners are in the legal custody of the Secretary of the Department of Justice (DOJ), and specifically Corrections Victoria and Justice Health.
Corrections Victoria is responsible for operating public prisons, and provides a range of programs within these prisons to help prisoners address the causes of their offending, and to prepare for their return to the community. This includes programs to address mental illness. Justice Health is responsible for health services in prisons, including health services policy and quality standards, and compliance monitoring across all prisons.
Prison health services provide psychiatric consulting, nursing and inpatient treatment for prisoners with a mental illness. Under the Mental Health Act 2014 (the Act), compulsory mental health treatment cannot be provided in prisons. For a prisoner to be transferred for compulsory treatment, a psychiatrist must first be satisfied that criteria for compulsory treatment under the Act apply. The mental health service to receive the patient must also be satisfied that the prisoner meets the criteria, and that the mental health service is able to detain and treat the prisoner. The Secretary of DOJ may then make an order for the prisoner to be transferred to the mental health service to undergo compulsory treatment.
Patients under an order that requires compulsory treatment are under the care of the Chief Psychiatrist and are the responsibility of the Secretary of Department of Health (DH). Prisoners receive compulsory treatment at Thomas Embling Hospital, which has appropriate security. Thomas Embling also provides compulsory treatment for civil patients, and long-term secure care for people with a mental illness who are judged unfit to be tried under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997. Thomas Embling Hospital is operated by Forensicare.
4.2 Conclusion
DOJ and DH are responsible for mental health services for people with a mental illness held in their custody. Mental health facilities in prisons and for compulsory care outside prisons have not kept pace with demand, although new prison facilities are planned to be available in 2017. While DOJ and DH are not guided by a current joint plan, their strong collaboration is supporting their discussions of future mental health facilities and services inside prisons, and options for facilities and services outside prisons. Victoria Police has improved health services for people held in police custody.
Victoria Police health services are not included in current planning for prison health services or mental health services for people with offending backgrounds in the community. Victoria Police has made improvements to its Custodial Health Service since 2012, and is now reviewing these improvements. Victoria Police does not centrally report the time that people with a mental illness are held in police custody before transfer to prison.
4.3 Police cells, prisons and trends in mental illness
Figure 4A shows the number of people in police custody rose sharply between early 2012 and late 2013, peaking at 372 in November 2013, and most recently at 354 in March 2014. At 30 June 2014 there were 233 people held in police custody.
Figure 4A
Daily number of prisoners in police custody
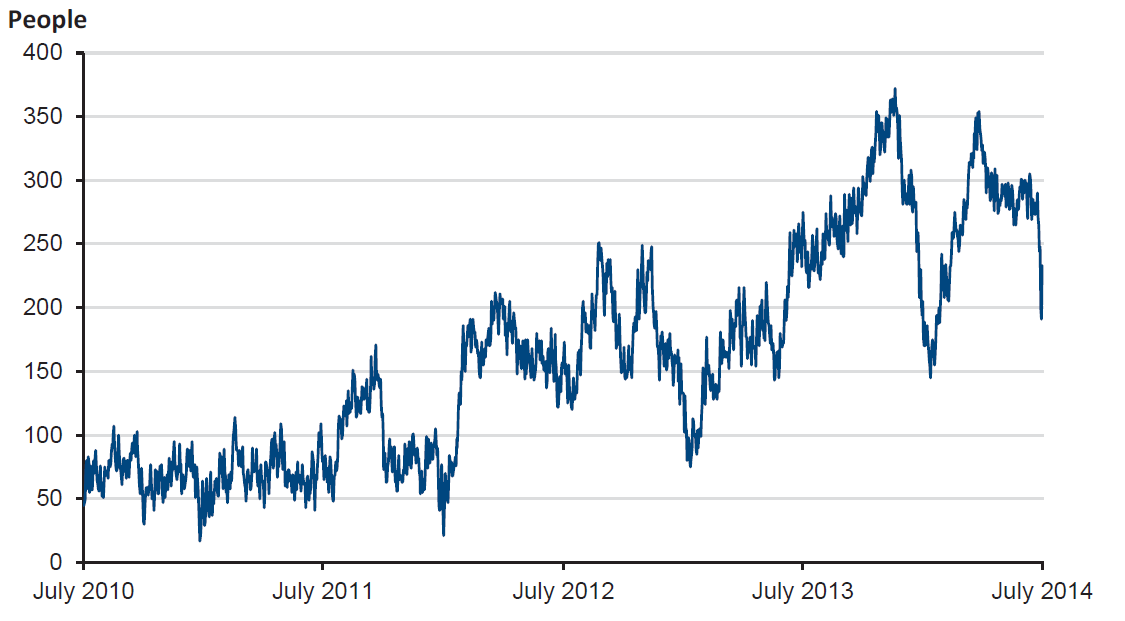
Source: Victorian Auditor-General's Office from Department of Justice data.
Figure 4B shows the rates of mental illness among people in police custody compared with rates in the general community. The rates of mental illness among people in police custody were identified in a 2010 study of 150 people held at two busy metropolitan police stations. The study found indicators of mental illness to be significantly higher than in the general community.
Figure 4B
Rates of mental illness of people in police custody and the general population
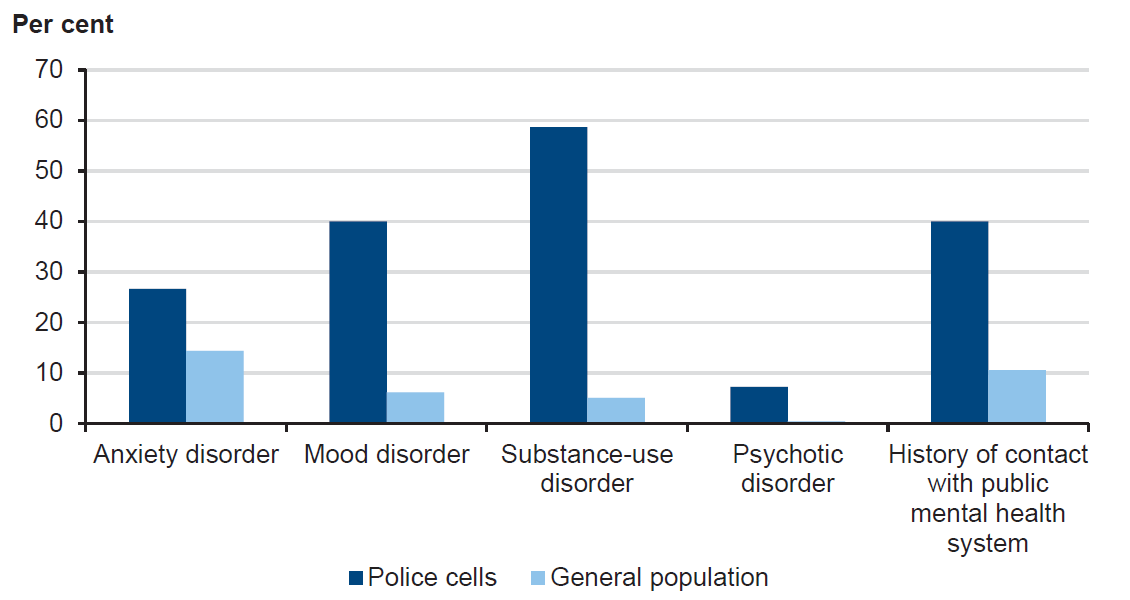
Source: Victorian Auditor-General's Office.
Figure 4C shows the monthly average number of males held in prisons with risk ratings for mental illness. A rating of P1 indicates a serious psychiatric condition requiring intensive and/or immediate care, P2 indicates significant or ongoing psychiatric condition requiring psychiatric treatment, and P3 a stable psychiatric condition requiring an appointment or continuing treatment.
Figure 4C
Male prisoners with risk ratings for mental illness
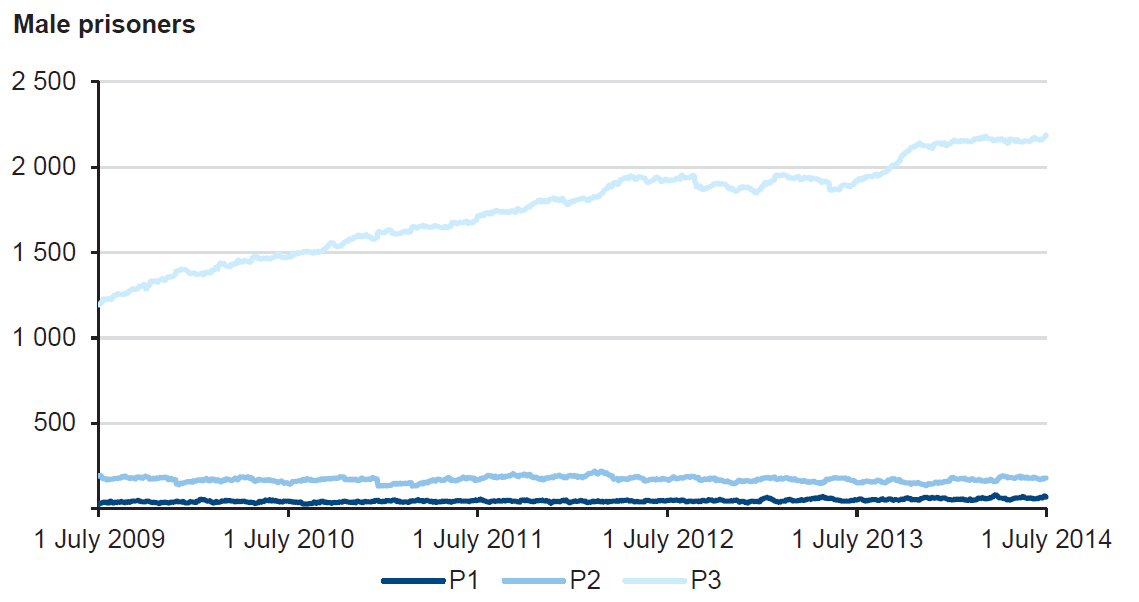
Source: Victorian Auditor-General's Office from Department of Justice data.
The combined total of male prisoners with P1 or P2 risk ratings has remained relatively constant at an annual daily average of between 211 and 223 from 2009–10 to 2013–14. The number of female prisoners with risk ratings of P1 and P2 was also relatively constant at an annual daily average of 19 to 23 prisoners from 2009–10 to 2013–14. Prisoners with P1 and P2 risk ratings can only be held at Melbourne Assessment Prison, Dame Phyllis Frost Centre, or the Melbourne Remand Centre.
The number of male prisoners with P3 risk rating, indicating a stable psychiatric condition that requires assessment or continuing treatment, has risen sharply from an annual average of 1 372 in 2009–10 to 2 104 in 2013–14, an increase of 53 per cent. This compares with an increase in the annual average male prisoner population of approximately 29 per cent over the same period. It indicates that an increasing proportion of the growing prisoner population requires ongoing psychiatric treatment, and, should their condition deteriorate, may also require inpatient care in prison, or at Thomas Embling Hospital.
Figure 4D shows mental health inpatient facilities in the prison system, and facilities for compulsory treatment of prisoners under the Act.
Figure 4D
Mental health inpatient facilities in prisons and for compulsory treatment
|
Prison |
Patient cohort |
Beds |
|---|---|---|
|
Melbourne Assessment Prison, Acute Assessment Unit (AAU) |
Male, voluntary care |
16 |
|
Port Phillip Prison, St Paul's Psycho-social Rehabilitation Unit |
Male, voluntary care |
33 |
|
Dame Phyllis Frost Centre, Marrmak Unit |
Female, voluntary care |
20 |
|
Thomas Embling Hospital |
Male and female prisoners, |
25 at |
Note: Under the Act compulsory treatment can only be provided in Thomas Embling Hospital. Beds available for prisoners in Thomas Embling Hospital depends on demand from patients who cannot be managed in mental health services and require compulsory treatment in a secure facility, and patients held under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997.
Source: Victorian Auditor-General's Office.
Over the past five years prisoner numbers have increased 29 per cent from a daily average of 4 492 in 2009–10 to 5 800 in 2013–14, but there has been no increase in the number of prison mental health beds. This has affected male prisoners particularly with the number of male prisoners per mental health bed rising from 85 in 2009–10 to 110 in 2013–14. The number of female prisoners per mental health bed was 20 in 2013–14.
Prison mental health services have increased, and new services and resources have been added to meet demand from increased prisoner numbers and incidence of mental illness. For example, over the period 2009–10 to 2013–14 psychiatric nursing consultations to prisoners held outside of the AAU at Melbourne Assessment Prison, the St Paul's Unit at Port Phillip Prison, and the Marrmak Unit for women at Dame Phyllis Frost Centre has increased by over 110 per cent.
Figure 4E shows the annual average bed utilisation in prison mental health inpatient units for male and female prisoners. Utilisation of male inpatient facilities has continued to rise and is close to 100 per cent at the AAU and St Pauls Unit. Utilisation of the Marrmak Unit for women at Dame Phyllis Frost Centre was lower, averaging around 80 per cent in 2013–14.
Figure 4E
Average utilisation of prison mental health beds
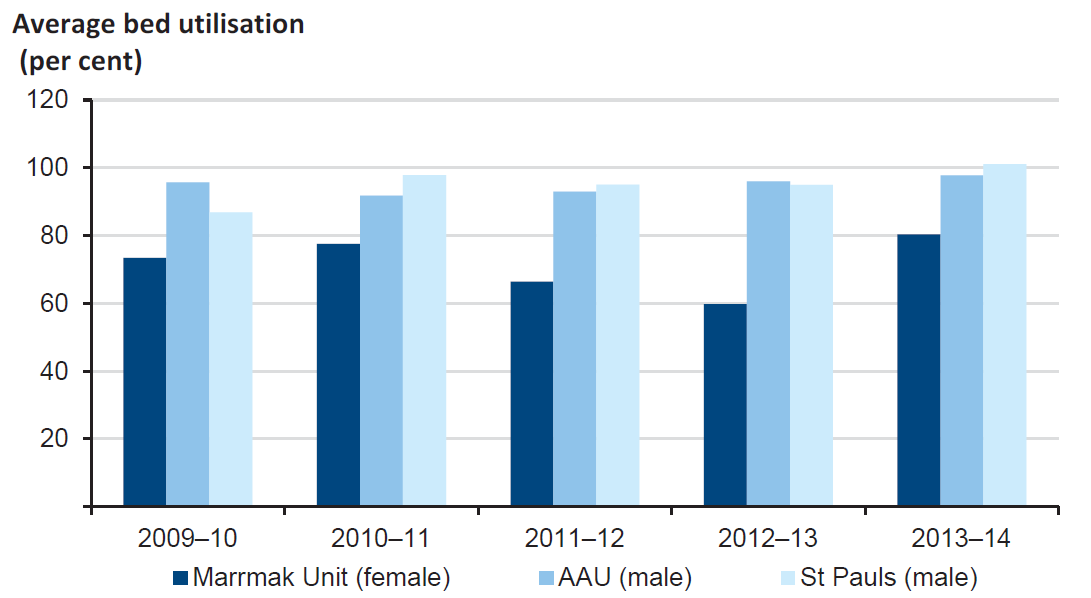
Note: AAU bed occupancy taken daily at midnight. Beds unoccupied overnight are counted as vacancies. Forensicare records AAU bed utilisation as effectively 100 per cent.
Source: Victorian Auditor-General's Office from Department of Justice data.
Under the Act a prisoner with a mental illness may be taken to Thomas Embling Hospital, detained and treated. Such action requires that all the criteria set out at section 276 of the Act apply. The criteria include that treatment is required to prevent serious deterioration in a prisoner's mental or physical health, or to prevent serious harm to the prisoner or to another person. Patients are returned to prison when the criteria of section 276 of the Act no longer apply.
The number of beds available for prisoner patients at Thomas Embling Hospital has steadily reduced as the number of patients held under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 has increased. The number of patients held as unfit to be tried has increased from 52 at 30 June 2005 to 77 at 30 June 2014. There were 25 beds allocated to prisoner patients at 30 June 2014. Total bed numbers at Thomas Embling Hospital increased from 100 to 118 in 2007 and were reduced to 116 in 2010.
As a result of high demand for beds at Thomas Embling Hospital, the average time that prisoners in the AAU wait to be admitted for compulsory treatment has increased significantly from 5.3 days in 2009–10, to 22.2 days in 2013–14.
4.4 Planning and agency-level coordination
When offenders are held in custody there are opportunities to identify mental health issues and start actions to manage them. People who are charged and facing court, move between police cells and prisons. Effectively addressing their mental illness requires effective collaboration between Victoria Police, DOJ, courts and mental health services.
There is no current plan that integrates mental health across police cells, prisons, and mental health facilities, and services for people with offending backgrounds in the community. Justice Health is planning for an additional 75 mental health beds expected to be available at Ravenhall Prison in 2017 and DH is planning facilities and services for people with a mental illness and offending backgrounds outside prisons. However, indicators of under-capacity in prison facilities and compulsory mental health facilities outside prisons have been apparent for several years.
4.4.1 Planning for police cells
Victoria Police's Custodial Health Service is not within the scope of either Justice Health's Prison Health Services Project, or DH's Forensic Mental Health Service Planning Project, indicating the agencies are not planning to include health services in police cells in future health services procurement.
However, Custodial Health Service was included in Justice Health's 2010 planning for prison health services that aimed to commission a single lead provider of health services for police, corrections and courts. As the proposal was not successful, prison health services were recommissioned in accordance with the arrangements in place prior to 2011, and Victoria Police continued to provide health services for people in police custody.
The continued separation of Victoria Police and prison health services increases the importance of the two health services maintaining effective coordination around prisoners with a mental illness.
Victoria Police undertook planning for Custodial Health Service in 2011. Victoria Police identified it was at risk of not meeting demand for custodial health care, of adverse outcomes including deaths in cells, and of the need to manage prisoners drawing too many police resources away from police operations. Victoria Police has strengthened its Custodial Health Service since 2012, and is now reviewing its improvements.
4.4.2 Planning for prisons
Justice Health and DH are currently undertaking planning for prison mental health services, and mental health facilities and services for people with offending backgrounds in the community. Prison mental health service planning covers existing facilities and 75 additional mental health beds expected to be available at Ravenhall Prison in 2017. However, DOJ and DH have not clarified their decision-making arrangements to ensure that decisions arising from each agency's planning are coordinated and address the current delays for prisoners with a severe mental illness requiring treatment. Indicators of under-capacity within prison and compulsory mental health facilities have become extreme.
Justice Health is currently undertaking comprehensive planning for prison health services for 2017–27. It is reviewing the efficiency and effectiveness of the current prison health system and developing options for improvement. While Justice Health has not completed planning for mental health, its planning is taking into account new specialist mental health facilities and services to be based at Ravenhall Prison, increasing prisoner numbers, increasing levels of mental illness, and potential changes to treatment times and patient management arising from patient involvement in treatment decisions under the Act.
DH's Forensic Mental Health Services Planning Project (FMHSPP) will make recommendations for future mental health service capacity and physical configuration, as well as pathways between prison mental health services, compulsory inpatient facilities, and community mental health services for people with offending backgrounds. FMHSPP is a comprehensive review based on thorough research and analysis. It is considering compulsory inpatient services, prison secondary and tertiary mental health services, programs linking the justice and mental health systems, and programs in the community to support people with a mental illness and offending backgrounds. FMHSPP will consider demand to 2028.
FMHSPP has identified factors that are delaying prisoners' access to Thomas Embling Hospital for compulsory treatment. Compulsory care at Thomas Embling Hospital is able to assist prisoners where criteria of section 276 of the Act are satisfied. Under the Act compulsory care may only be provided at certain hospitals. Of those, Thomas Embling is the only hospital with security sufficient to admit prisoners.
The Thomas Embling Hospital has 116 beds—of which 25 are allocated for prisoner patients—but capacity for prisoners requiring short‑term treatment is increasingly limited as the number of patients held for long periods under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 has increased from 52 at 30 June 2005, to 77 at 30 June 2014.
This has limited the number of beds available for prisoners requiring compulsory care. As a result, prisoners are being held for considerable periods at the Melbourne Assessment Prison's AAU. At June 2014 over 50 per cent of patients in the AAU were waiting for admission to Thomas Embling Hospital. The average number of days between prisoners being certified for compulsory treatment and their admission to Thomas Embling Hospital has increased from 5.3 in 2009–10 to 22.2 in 2013–14.
While DOJ is adding 75 mental health beds at Ravenhall Prison in 2017, without an investment in compulsory care facilities outside prisons, severely ill prisoners will continue to wait in prisons for access to the compulsory treatment they require.
4.4.3 Agency-level communication and coordination
DOJ and DH have arrangements to communicate around forensic health at an agency level. In particular, the agencies have well-established communication around mental health through the Justice Health Joint Management Committee (JMC)—a permanent committee chaired by the Deputy Secretary for Corrections with membership of Victoria Police, Corrections Victoria, Justice Health, and DH—DH's Director of Mental Health is a member.
The JMC establishes and receives advice from groups involving DOJ, DH, Victoria Police and health services. A Clinical Advisory Committee—including DH, Victoria Police, and health experts—advises JMC on standards and policies for prison health services and facilities. A working group on mental health and alcohol and other drugs in the justice system is alternately hosted and chaired by Justice Health and DH and includes Corrections Victoria and DOJ's Courts Policy group. Regular communication at this level provides the basis for effective communication and coordination around formal planning activities.
This coordination has helped Justice Health and DH to work closely from the inception of their inter-related planning projects—Justice Health's Prison Health Services Planning Project and DH's FMHSPP. Each agency has sound oversight arrangements that provide for cross-agency coordination.
However, the agencies have not clarified leadership of decisions around the balance of investment in the mental health systems inside and outside of prisons arising from their current planning activity. The agencies have separate accountability around decisions on investment in mental health facilities and services for people with a mental illness involved in the justice system.
The Secretary of DOJ's custodial responsibility to prisoners requires that DOJ directly control prison health services. Funding for Forensicare, which operates the state's secure mental health hospital, Thomas Embling Hospital, is at the discretion of the Minister for Mental Health. However, JMC terms of reference state that JMC is a cross‑portfolio governance arrangement that is to ensure integration of forensic health services. In addition, the terms state that JMC is to direct and support joint funding submissions.
While JMC helps DOJ and DH identify potential issues around their inter‑dependent responsibilities at an early stage of their planning, it cannot govern the agencies' decisions, nor can it direct joint funding bids. As a result, DH and Justice Health's planning may not be effective in improving outcomes for people with a mental illness in the justice system.
4.5 Program and service-level coordination
Victoria Police's responsibility for managing offenders in its custody requires that it effectively collaborates with other agencies and service providers. While collaboration does occur, there are gaps that limit the effectiveness of the management of offenders with a mental illness.
4.5.1 Coordination of police health services
The effectiveness of Victoria Police in managing people with a mental illness in police custody is dependent on its Custodial Health Services, and on the timely transfer of prisoners to Melbourne Custody Centre and Melbourne Assessment Prison where they can receive a higher level of care.
Victoria Police has procedures and guidelines in place to locally manage prisoners with a mental illness, and coordinate with health services. Police managing custody units are responsible for managing prisoners with a mental illness, identifying risk, and accessing health services in accordance with detailed requirements relating to observation, and obtaining medical assistance, among other things.
Victoria Police's Custodial Health Service provides nursing, medical and pharmacy services and assistance to police custody managers in monitoring police prisoners prior to their transfer to the prison system. This includes nursing visits to metropolitan police stations, daily contact with rural police stations, and 24-hour health advice. Police managers of custody units remain responsible for obtaining and acting on advice in the absence of nursing staff.
The Custodial Health Service provides health assistance suitable for relatively short periods of custody in police cells. Victoria Police has procedures for moving prisoners with a mental illness from regional areas to large metropolitan stations, or to Victoria Police's Melbourne Custody Centre, where they can receive 24‑hour health care. However, Victoria Police's effectiveness in managing prisoners with a mental illness also depends on their timely transfer to prison where they can receive more comprehensive care than possible in police cells.
4.5.2 Coordination of transfers between police detention and prisons
Victoria Police and Corrections Victoria have procedures for managing transfer of prisoners between police cells and prisons. However, there are weaknesses in coordination between Victoria Police and Corrections Victoria for the transfer of prisoners with a mental illness. Justice Health is now reviewing processes for health‑related communication between Victoria Police's Custodial Health Service and prison health services to ensure these are effective. Victoria Police does not centrally monitor, for system management purposes, the time that prisoners with a mental illness are held in police cells before being transferred to prison.
Custodial Health Service and the reception prisons, the Melbourne Assessment Prison and Dame Phyllis Frost Centre constantly exchange information on prisoners' mental health, as they do not have access to a common prisoner health records system. Custodial Health Service maintains its own health records database to record details of prisoners' behaviour and health since arrest.
Justice Health has commenced a review of the processes for transferring health information and prisoner medication between health service providers at prisons, the Victoria Police custody centre and police cells. The review is to identify and address any weaknesses in these processes. Justice Health's electronic prisoner health record system is expected to include Victoria Police's Custodial Health Service, as well as all prison health services, and will remove the need for information exchange between Victoria Police and prison health services.
Victoria Police and Corrections Victoria have processes to manage the transfer of prisoners between police cells and prisons each day. This includes managing requests from the Custodial Health Service to give priority to prisoners with a mental illness who need treatment at Melbourne Assessment Prison's AAU. However, Victoria Police does not centrally monitor trends in the average time that such prisoners wait for transfer. This contrasts with Justice Health's reporting on the waiting time for prisoners requiring access to the AAU and Thomas Embling Hospital. Such monitoring would assist Victoria Police and Corrections Victoria to identify and manage issues affecting processes for transferring prisoners with a mental illness.
Recommendations
- That the Department of Justice and the Department of Health prepare a joint plan for mental health facilities inside and outside prisons to guide future funding bids.
- That the Department of Justice amends the terms of reference of the Justice Health Joint Management Committee to reflect its role as a forum for agency communication and coordination.
- That Victoria Police monitors and reports the time that prisoners with a mental illness are held in police cells before transfer to the prison system.
5 Community
At a glance
Background
Corrections Victoria (CV), Justice Health and Department of Human Services (DHS) help prisoners with a mental illness preparing to return to the community at the end of their prison sentences. Community Correctional Services supervises offenders sentenced to community correction, and refers offenders with a mental illness to general practitioners and mental health services.
Conclusion
CV, Department of Health (DH) and DHS plan and operate support and housing programs for released prisoners, but planning is not informed by a consistent framework of objectives, or current and future demand. CV does not maintain regular agency-level communication with DH and DHS.
Findings
- Offenders commencing community supervision with the highest risk rating for mental illness has increased 168 per cent between 2009–10 and 2012–13. For those completing prison sentences, it has increased by 46 per cent between 2009–10 and 2012–13.
- The Department of Justice, DH and DHS are not effectively coordinating planning for the justice system of programs to support released offenders with a mental illness.
- CV, DH and DHS do not maintain regular agency-level contact around community supervision and prisoner release support programs.
- CV and DHS do not effectively coordinate support and housing services for prisoners of varying levels of need who are nearing release from prison.
Recommendations
That the departments of Justice, Health and Human Services:
- establish arrangements to improve coordination, collaboration and planning across the three agencies
- review the range of post-release and community correction programs to identify opportunities for improved effectiveness and efficiency.
5.1 Introduction
Community Correctional Services, part of Corrections Victoria, is responsible for supervising offenders subject to community correction orders, and parolees. Community correction orders were introduced in January 2012 under the Sentencing Amendment (Community Correction Reform) Act 2011. The Act provides for a court to attach conditions to community correction orders, including the requirement for an offender to undergo mental health treatment.
Corrections Victoria helps prisoners preparing to return to the community at the end of their sentence. This includes providing prisoners with information and advice before their release, and providing more intensive support to selected prisoners after their release.
Since 2012, released prisoners with the most serious mental health needs have received intensive support to engage with their local mental health service. People with a mental illness, cognitive impairment and alcohol and other drug dependency may also be supported by the Department of Human Services (DHS) upon release from prison.
5.2 Conclusion
Addressing the mental health of offenders after release from prison, and while on community correction orders presents opportunities to reduce the rates of reoffending. Maximising these opportunities requires the key agencies involved at this part of the criminal justice system to work effectively together.
Corrections Victoria, Department of Health (DH) and DHS plan and operate support and housing programs for released prisoners and prisoners on correction orders, but planning is not informed by a consistent framework of objectives, or a clear understanding of current and future demand. Corrections Victoria does not maintain the regular agency-level communication with DH and DHS that could support improved effectiveness of programs for released prisoners.
Therefore there are significant opportunities to improve the combined effectiveness and efficiency of the programs to improve outcomes for offenders with a mental illness.
5.3 Community supervision and support, and trends in mental illness
Offenders sentenced to correction in the community, or released from prison on parole, are supervised by Community Correctional Services. Community Correctional Services refers offenders and parolees with a mental illness to mental health treatment based on their assessed needs.
Figure 5A shows for 2009–10 to 2013–14 the number of male and female offenders and parolees with risk ratings for mental illness commencing a period of Community Correctional Services' supervision. Between 2009–10 and 2012–13, the number of offenders commencing community correction orders and parole with P1 risk rating increased 168 per cent from 28 to 75, with P2 risk rating remained steady, and with P3 increased by 64 per cent to 1 106. The number of offenders under Community Correctional Services supervision with risk ratings for mental illness declined in 2013–14 due to a 43 per cent reduction in those commencing parole in the previous year, and a 13 per cent reduction in those commencing a community correction order.
A rating of P1 indicates a serious psychiatric condition requiring intensive and/or immediate care, P2 indicates significant or ongoing psychiatric condition requiring psychiatric treatment, and P3 a stable psychiatric condition requiring an appointment or continuing treatment.
Figure 5A
Male and female offenders commencing community correction orders or parole with risk rating for mental illness
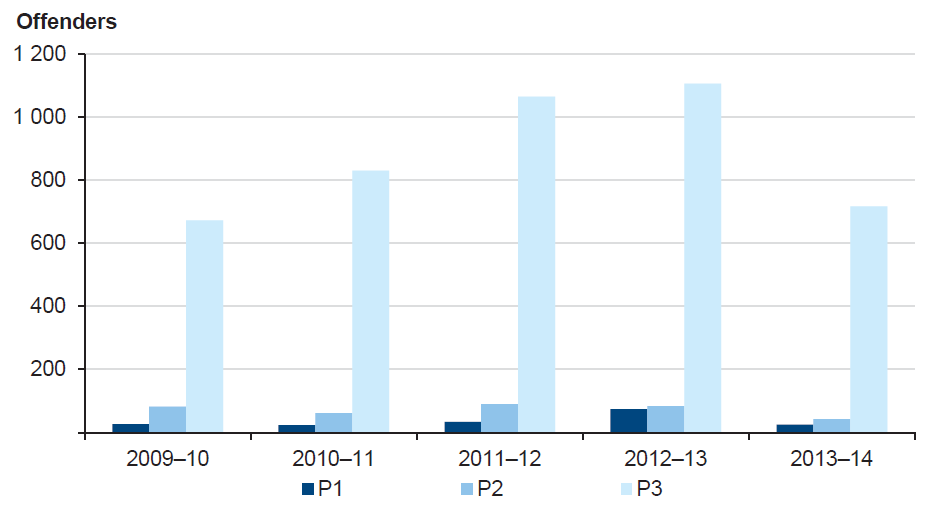
Source: Victorian Auditor-General's Office from Department of Justice data.
Released prisoners with a mental illness may be supported through Correction Victoria's Intensive Transitional Support Program (ITSP). Some released prisoners may also receive assistance through Justice Health's Community Integration Program (CIP), which assists prisoners with a serious mental illness engage with area mental health services after release. DHS's Multiple and Complex Needs Initiative (MACNI) assists complex clients, who exhibit violent or dangerous behaviour, and require intensive support. Approximately 80 per cent of people referred to MACNI have a mental illness.
Figure 5B shows for 2009–10 to 2013–14 the number of prisoners released with risk ratings for mental illness at completion of their sentences. The number of prisoners released annually with P1 risk rating has increased 46 per cent from 46 in 2009–10 to 67 in 2013–14, with P2 declining slightly to 119, and P3 increasing by 39 per cent to 1 300.
Figure 5B
Male and female prisoners released at completion of prison sentence with risk rating for mental illness
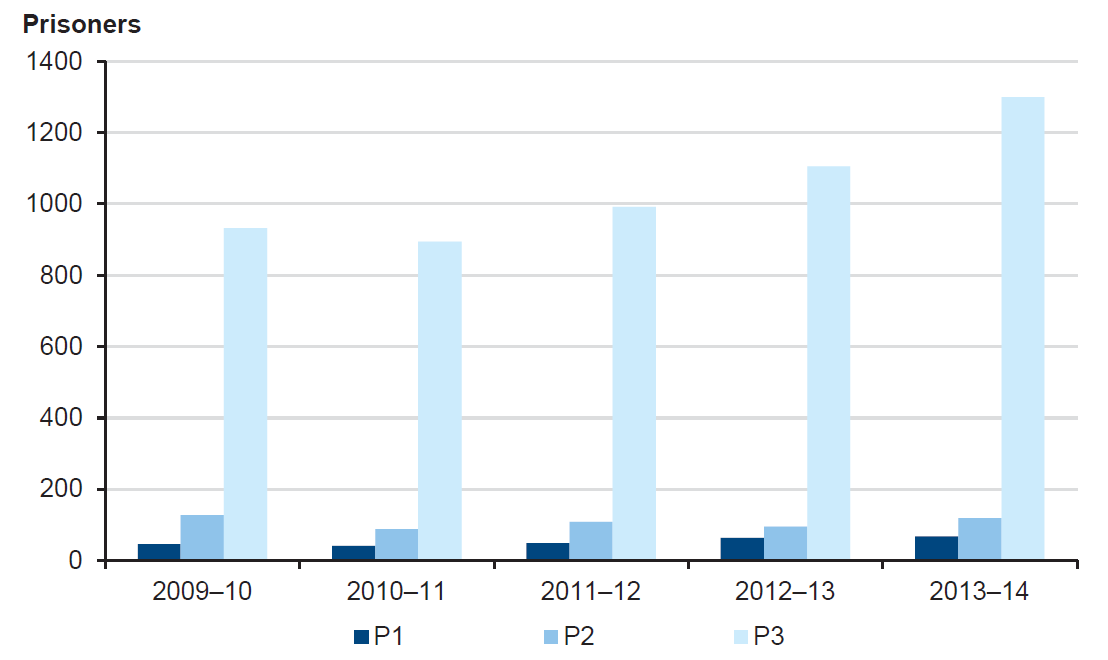
Source: Victorian Auditor-General's Office from Department of Justice data.
The capacity of support programs is shown in Figure 5C. Support programs are designed for released prisoners with a range of needs including mental illness. Not all released prisoners with a mental illness require such support.
CIP provides support for around 40 prisoners released from Melbourne Assessment Prison (MAP) or Dame Phyllis Frost Centre (DPFC) with a serious mental illness each year. This represents around 20 per cent of prisoners released each year with P1 or P2 risk ratings for mental illness. ITSP provided 655 client support packages each year. This represents around 50 per cent of prisoners released each year with P3 risk rating for mental illness.
ITSP will be replaced with the Corrections Victoria Reintegration Program (CVRP) in January 2015. Corrections Victoria has undertaken significant planning to ensure that CVRP better addresses prisoner transition needs, with the aim of successfully reintegrating them back into the community. Prisoner mental health is one of seven priority areas for the program, along with housing, employment, education and training, independent living skills, alcohol and drugs issues, and family and community connectedness.
Figure 5C
Support programs available to released prisoners with a mental illness and other complex needs
|
Program |
Eligibility |
Approximate client numbers |
|---|---|---|
|
ITSP |
Multiple needs and moderate to high reoffending risk |
Up to 655 clients for 2011–12 to 2013–14 for pre- and post-release support of between one and 12 months |
|
CIP |
Leaving MAP or DPFC with severe mental illness and high reoffending risk |
Average of 40 clients each year for transitional support of 12 weeks |
|
Multiple and Complex Needs Initiative |
Violent behaviour and at least two of:
|
Average of 30 clients at any time for program of 12 to 36 months |
Note: ITSP will be replaced with CVRP in January 2015.
Source: Victorian Auditor-General's Office.
Figure 5D illustrates the experience of people released from prison with a serious mental illness and the support work of mental health services. The case combines the experience of more than one person.
Figure 5D
Transition to the community
|
Mr G is a 29-year-old man diagnosed with schizophrenia and multiple substance abuse. He has been homeless since his early teens. He has a long history of offending with charges including assault, threats to kill, breaching intervention orders, and theft- and drugs‑related charges. He has had numerous prison sentences and intervention orders. It has been suggested that Mr G has an antisocial personality disorder but this has not been formally diagnosed. Mr G was transferred to Thomas Embling Hospital from MAP where he was serving a sentence for theft, threats to kill, assaults and resisting police. He was admitted because his psychotic symptoms relapsed. He remained at Thomas Embling Hospital for five months and was referred to the CIP as his parole eligibility approached, and was accepted into the program. Mr G was granted parole and discharged from Thomas Embling Hospital. He was placed on a community treatment order supervised by the area mental health service (AMHS). AMHS had him managed by the local mental health crisis team until his support needs could be assessed. On discharge Mr G struggled to cope with the demands of living in the community and he disappeared to regional Victoria for a few days. As a result Mr G's parole was cancelled and he was returned to prison. During this period it was apparent that the AMHS' assessment of Mr G's risk level was too high, and that the support was causing him difficulties. The AMHS assessment of Mr G's risk was higher than that of the CIP and Thomas Embling Hospital. A further risk assessment was carried out with Mr G that showed his history indicated a moderate risk of future violent offending, but this was reduced by his current clinical presentation and would be further moderated with consistent treatment of his drug and alcohol issues and his mental health. The report was shared with the clinical team, and discussed with the AMHS. The team decided that they would assess Mr G in prison to follow up on the risk assessment, and agreed with the recommendation that Mr G receive assertive case management upon release. The CIP and AMHS planned support for Mr G before his release. The CIP arranged a temporary house for Mr G. Having accommodation would mean Mr G would remain in the AMHS catchment, and would have stable housing for the first time in his adult life. When released from prison Mr G was allocated a case manager and a psychologist to work on drug and alcohol issues. On the last visit, Mr G told his clinician that 'I never thought things could be this good'. He has not reoffended or used drugs since his discharge from hospital and reports being very proud of this achievement. He has consistent treatment for his mental health and drug and alcohol use, stable housing, community support, and is currently looking for a job. |
Note: Details of this case have been changed to protect confidentiality.
Source: Victorian Auditor-General's Office from Forensicare data.
5.4 Planning and agency-level coordination
Managing prisoners with a mental illness after release from prison, or on community correction orders, is a challenging responsibility. Done effectively, it can reduce the risk of reoffending. Not only does it require the offender to actively engage in treatment or other programs, but it also involves multiple agencies working together.
There is, however, insufficient coordination of planning among the key agencies to support mentally ill convicted offenders released from prison. Despite the Department of Justice (DOJ), DH and DHS operating and planning various support and housing programs, there is no evidence that planning is informed by a consistent framework of objectives, or of analysis of current and future demand.
Figure 5E outlines the current support and housing programs of DOJ, DHS, and DH for people with a mental illness adjusting to life in the community after involvement in the justice system.
Figure 5E
Support and housing programs relevant to people with a mental illness released from prison
|
Program |
Agency |
Eligibility |
Support |
Housing |
|---|---|---|---|---|
|
Moderate mental illness or multiple needs |
||||
|
ITSP and Corrections Victoria Housing Program |
DOJ / Corrections Victoria |
Moderate/high reoffending risk and multiple needs |
Assessment, case planning and coordination, support and monitoring |
9–12 months |
|
Corrections Housing Pathway Initiative |
DHS |
Supported under ITSP |
Tenancy management and support |
Transitional |
|
Severe mental illness or multiple needs |
||||
|
CIP |
DOJ / Forensicare |
Leaving MAP or DPFC with severe mental illness and high reoffending risk |
Short-term support and link to AMHS |
As per needs of client |
|
Forensics Pathway Initiative |
DHS |
Leaving MAP with high risk of homelessness |
Housing information and referral |
As per needs of client |
|
Multiple, high-level needs |
||||
|
MACNI |
DHS, DH, DOJ |
Violent behaviour and at least two of:
|
Individual support planning and coordination |
As per needs of client |
Source: Victorian Auditor-General's Office.
Corrections Victoria's ITSP provides graded support packages with case management for released prisoners with multiple needs, including a mental illness, and supported housing through the Corrections Victoria Housing Program. DHS provides housing and other support services accessible to prisoners as part of its public and social housing programs.
Justice Health funds Forensicare to operate the CIP for released prisoners leaving the MAP and DPFC, with a severe mental illness and high risk of reoffending. This program provides short‑term support to link released prisoners with a local AMHS. DH's Forensic Mental Health Services Planning Project (FMHSPP) has proposed a model, currently under consideration, to complement the CIP by providing longer‑term non‑clinical support for this cohort of released prisoners.
DHS operates MACNI for released prisoners with a mental illness, cognitive disability and AOD dependency whose recovery cannot be supported through normal support services. This program provides intensive and coordinated support to clients, including some released prisoners. DH and DOJ are partners of the MACNI program.
Corrections Victoria has undertaken significant planning for its new CVRP. However, there is no common framework of objectives to guide allocation of places across the agencies' programs so that released prisoners at various levels of need, including with mental illness, are effectively supported to reduce their reoffending.
In addition, planning for the programs across agencies is not informed by a single model of future demand at various levels of need, and geographic regions. As a result, the combined outcomes of agencies' current programs, and proposed programs under consideration, may not effectively cover the spectrum of need and reoffending risk among released prisoners with a mental illness. Agencies will be unable to prioritise future investment to most effectively reduce reoffending.
5.4.1 Agency-level communication and coordination
Corrections Victoria, DH and DHS do not maintain regular agency-level contact around programs for community supervision and transition from prison. The absence of regular agency-level contact increases the risk that the agencies will miss opportunities to improve programs and services for people with a mental illness, or be unaware of changes that affect agencies' ability to fulfil their accountabilities. This is particularly the case as Corrections Victoria, DH and DHS are involved in separate reforms that affect programs relevant to people with a mental illness.
Corrections Victoria and DHS are working together as part of Corrections Victoria's review of prisoner transition programs. The agencies are jointly assessing opportunities to improve housing and other support services for released prisoners with multiple needs, and have discussed opportunities to integrate prisoner transition programs with Services Connect, DHS's client-focused model for improving human service delivery. These discussions are at an early stage. However, the agencies' engagement recognises that current reforms to human services and homelessness strategy and reforms to Corrections Victoria's transition programs may provide opportunities for both agencies to improve outcomes in their areas of responsibility.
Conversely, there is an absence of regular exchange between Corrections Victoria and DH at the central‑agency level. As a result, Corrections Victoria may miss opportunities to better adapt mental health and related services to the needs of clients leaving prison, or on community correction orders. Previous and current examples are:
- Community Correctional Services and DH did not effectively communicate around impending changes to DH's community mental health services, and the introduction of catchment-based assessment, planning and referral of clients to mental health services. The changes simplify Community Correctional Services' management of client referrals.
- DH's initiatives, funded by Corrections Victoria under sentencing reforms, to provide targeted AOD, behavioural and mental health services to people primarily with AOD dependency, but also with a mental illness or acquired brain injury on community correction orders.
- DH and DHS' development of their work plan for dual disability services. Dual disability describes conditions involving both mental impairment and mental illness, which affects many people in the justice system. Corrections Victoria is a significant user of mental health, AOD and disability services.
Corrections Victoria's lack of regular engagement with planning and development in the health and human services sector suggests the agency is not comprehensively focused on the contribution these programs and services make to reducing rates of reoffending, for which Corrections Victoria is accountable.
5.5 Program and service-level coordination
5.5.1 Community correction
Since 2010, Community Correctional Services has considerably strengthened its ability to effectively supervise offenders on community correction orders and prisoners on parole. However, Community Correctional Services with DH needs to continually monitor local coordination with health services to manage risks and improve outcomes of offenders with a mental illness.
Community Correctional Services refers offenders to a range of services depending on offenders' needs and the conditions of their orders. Community Correctional Services refers offenders with a mental illness to general practitioners (GP), psychiatric services delivered in the community, or AMHS inpatient services for serious or acute mental illness. Offenders with a mental illness may also be referred to treatment for AOD dependency, acquired brain injury and cognitive deficit, or behaviour management.
GPs are able to address the mental health requirements of most offenders on community correction orders, and are able to refer offenders to one of two Commonwealth-funded mental health programs. These programs provide for the GP to prepare a mental health treatment plan.
Community Correctional Services has mechanisms in place to manage the quality of its supervision of offenders and parolees. This includes:
- guidance for staff responsible for identifying offenders' mental health risks, supervising offenders, and engaging with health services
- processes for monitoring the quality of supervision, including timely referral of offenders to health services, and monitoring offenders' compliance
- standard information for health services, and requirements for health treatment plans.
In some areas of the state, Community Correctional Services experiences problems in accessing GPs who will accept patients with forensic backgrounds, or are attending under legal supervision. However, Community Correctional Services' ongoing interaction with health services, and case monitoring, reduce the risk of offenders not gaining timely access to appropriate treatment.
Justice and health agencies need to continually monitor coordination around managing patients with offending backgrounds.
Community Correctional Services and DH have a protocol to guide communication between community correction officers and AMHS. The protocol is to ensure that AMHS receive full and timely information of offenders' history of violence prior to their being admitted to an inpatient unit, or receiving services in the community. DH reports that AMHS have not reported widespread problems in communication with Community Correctional Services, but DH continues to monitor such issues through its regular meetings with AMHS.
5.5.2 Support on release from prison
There is insufficient coordination across agencies allocating support and housing to prisoners of varying levels of need nearing release from prison. Processes for allocating places are not coordinated across the programs or regions, meaning agencies are unable to show that prisoners nearing release with the most significant multiple needs and mental illness are receiving places.
Processes for accepting clients to MACNI, CIP, ITSP and the Corrections Housing Pathway Initiative are separate:
- MACNI—local area committees determine eligibility for the case planning and coordination of care that MACNI clients receive. The committee comprises program managers and specialist practitioners of DHS, DH and DOJ.
- CIP—Forensicare in consultation with prison assessment staff determines the allocation of places. Eligibility requires that clients are leaving the MAP or DPFC with a major mental illness, and have a high risk of serious reoffending.
- ITSP—staff located at each prison allocate places to prisoners who are nearing release. Eligibility requires that prisoners have a moderate or high risk of reoffending as determined by Corrections Victoria's risk assessment tool, multiple and complex needs that may include mental illness, and a willingness to participate voluntarily.
- Corrections Housing Pathway Initiative—staff of community organisations contracted by DHS visit prisons to provide a range of housing and other support services to prisoners nearing release who require assistance.
Prisons have assessment processes for identifying prisoners' needs and referring prisoners to appropriate programs. However, the separate processes for accepting clients to programs create the risk that the combined programs are not as effective as they could be. There is no confirmation that support of the various programs is effectively targeted to prisoners nearing release of differing levels of need, and reoffending risk. For example, it is not possible to determine whether prisoners nearing release who are ineligible for one level of support become eligible for support through a second agency.
While released prisoners' participation in ITSP is voluntary, there is no confirmation of whether support allocated across regions is targeting those released prisoners with highest needs, and greatest risk of reoffending. Corrections Victoria identified that its ITSP program had inadequate criteria and guidance for allocating places, no central listing of allocations of support packages, and that its ITSP and Corrections Victoria Housing Program databases were separate. While Corrections Victoria notes that it has significantly improved arrangements for managing the new CVRP, this will only be demonstrated when the program commences in 2015.
Corrections Victoria has undertaken significant work to implement new programs to support released prisoners. However, this work is not part of a coordinated suite of agency programs of support to released prisoners with a mental illness. The lack of coordination across these programs presents significant opportunities to target and improve service delivery, and ultimately improve prisoner outcomes.
Recommendations
That the departments of Justice, Health and Human Services:
- establish arrangements to improve coordination, collaboration and planning across the three agencies
- review the range of post-release and community correction programs to identify opportunities for improved effectiveness and efficiency.
Appendix A. Definition of terms
AAU
Acute Assessment Unit—mental health inpatient unit at Melbourne Assessment Prison.
AMHS
Area mental health service—area-based services providing a range of inpatient and outpatient mental health services.
AOD
Alcohol and other drugs.
ARC List
Assessment and Referral Court List—a specialist court list of the Magistrates' Court of Victoria aimed at meeting the needs of accused persons who have a mental illness and/or a cognitive impairment.
CCO
Community correction order—a court order requiring an offender complete a sentence while under supervision in the community.
CHS
Custodial Health Service—a division of Victoria Police with responsibility for health services for people detained in police cells.
CIP
Community Integration Program—a program operated by Forensicare that assists people with a serious mental illness leaving Melbourne Assessment Prison or Thomas Embling Hospital link with mental health services in the community. Justice Health funds these services for released prisoners.
CISP
Court Integrated Services Program—a program of the Magistrates' Court of Victoria that provides accused with support and services to reduce their risk of reoffending.
CISP Remand Outreach Pilot
A pilot program of the Magistrates' Court of Victoria that provides pre-sentencing support services to accused people held on remand.
CVRP
Corrections Victoria Reintegration Program—a program of Corrections Victoria to support released prisoners and reduce their risk of reoffending. Commences 2015.
CREDIT/Bail program
A program of the Magistrates' Court of Victoria that aims to increase the likelihood of an accused person being granted bail and successfully completing a bail period by assisting them with accommodation, alcohol and drug treatment, support services and material aid.
Criminal Justice System Steering Committee
A committee of senior leaders in the criminal justice system, chaired by the Secretary of Department of Justice and including representatives of all Victorian Court Jurisdictions, Victoria Police, the Director of Public Prosecutions, Victoria Legal Aid and the Department of Justice.
CVHP
Corrections Victoria Housing Program—a housing program for released prisoners.
Department of Health and Victoria Police Protocol for Mental Health
A protocol to guide police and clinicians on their respective roles and responsibilities when working together to respond to the needs of people with a mental illness.
DPFC
Dame Phyllis Frost Centre—Victoria's prison for women and the location of the Marrmak Unit—an inpatient unit for female prisoners with a serious mental illness.
Drug Court
A division of the Magistrates' Court of Victoria responsible for sentencing, monitoring and supervising the treatment of offenders with drug or alcohol dependency, who have committed an offence under the influence of drugs or alcohol or to support a drug or alcohol habit. The Drug Court operates at Dandenong Magistrates' Court.
ESLC
Emergency service liaison committees—local committees in each of the 21 health service regions established under the Department of Health and Victoria Police Protocol for Mental Health. Committees comprise local representatives of Victoria Police, area mental health services, Ambulance Victoria, and hospital emergency departments.
FMHSPP
Forensic Mental Health Services Planning Project—a planning project of the Department of Health's Mental Health, Drugs and Regions Division.
ICPF
Integrating Courts Programs Framework—a 2011 plan of the Magistrates' Court intended to guide wider integration in the Magistrates' Court of problem solving, therapeutic justice, and community engagement over a 10-year period. ICPF is no longer current.
IDLC
Interdepartmental liaison committee.
ITSP
Intensive Transition Support Program—a program of Corrections Victoria to support released prisoners and reduce their risk of reoffending. Concludes 2014.
Joint Management Committee
A Department of Justice committee for coordinating prison health services, with representation of Department of Health, Justice Health, Corrections Victoria and Victoria Police.
Justice Mental Health Strategy
A 2010 strategy of the Department of Justice that outlined criminal justice interventions addressing the needs of adult offenders with a mental illness, victims, witnesses, and people in need of assistance. The Justice Mental Health Strategy is no longer current.
LEDR Mark 2
Victoria Police system that includes function for managing referrals of members of the public to health and support services. LEDR Mark 2 commences operating in 2014.
MACNI
Multiple and Complex Needs Initiative—a program of the Department of Human Services to provide specialist interventions for people over 16 years with multiple needs who have displayed violent or dangerous behaviours.
Mainstreaming Working Group
A working group formed in 2012 to advise the Attorney-General on broader adoption of the Magistrates' Court of Victoria's neighbourhood Justice Centre, Court Integrated Services program, ARC List, Drug Court, and Koori Court.
MAP
Melbourne Assessment Prison—the reception point for the Victorian male prison system, and location of the Acute Assessment Unit for male prisoners with a serious mental illness.
MHCLS
Mental Health Court Liaison Service—a program of the Department of Health that operates in seven Magistrates' Courts and provides mental health assessment and liaison between justice and mental health services.
Peace of mind
Victoria Police's 2007 strategy for policing and mental health.
PRIMeD
Police Responses to the Interface with Mental Disorder—a 2007–2011 research project undertaken by Monash University and Forensicare in collaboration with Victoria Police and funded by the Australian Research Council to investigate current Victoria Police practices, policies and procedures for dealing with people with a mental illness, and interactions with mental health services.
Prison Health Services Planning Project
Justice Health's project to develop a prison health system model for the delivery of primary health, secondary and tertiary health, mental health and alcohol and other drug programs and services from 2017.
Thomas Embling Hospital
Victoria's mental health hospital for people with offending backgrounds.
Victorian health policy and funding guidelines
Performance and financial framework within which health entities funded by the state operate.
Victoria's priorities for mental health reform 2013–15
Department of Health's 2013 statement on priorities for mental health reform.
Appendix B. Audit Act 1994 section 16—submissions and comments
Introduction
In accordance with section 16(3) of the Audit Act 1994, a copy of this report, or part of this report, was provided to the Department of Justice, the Department of Health, the Department of Human Services, Victoria Police and Court Services Victoria.
The submissions and comments provided are not subject to audit nor the evidentiary standards required to reach an audit conclusion. Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
- Department of Justice
- Department of Health
- Department of Human Services
- Victoria Police
- Magistrates' Court of Victoria, incorporating Court Services Victoria's response
RESPONSE provided by the Secretary, Department of Justice
RESPONSE provided by the Secretary, Department of Health
RESPONSE provided by the Secretary, Department of Human Services
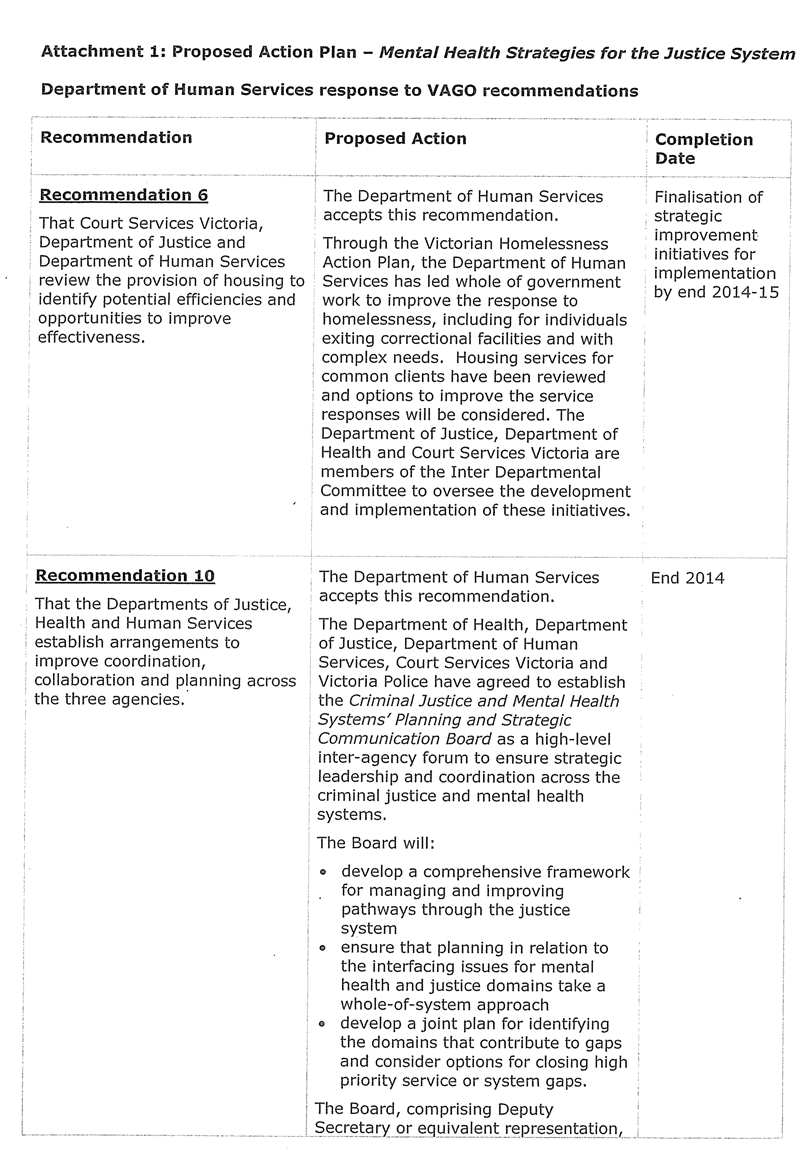
RESPONSE provided by the Chief Commissioner, Victoria Police
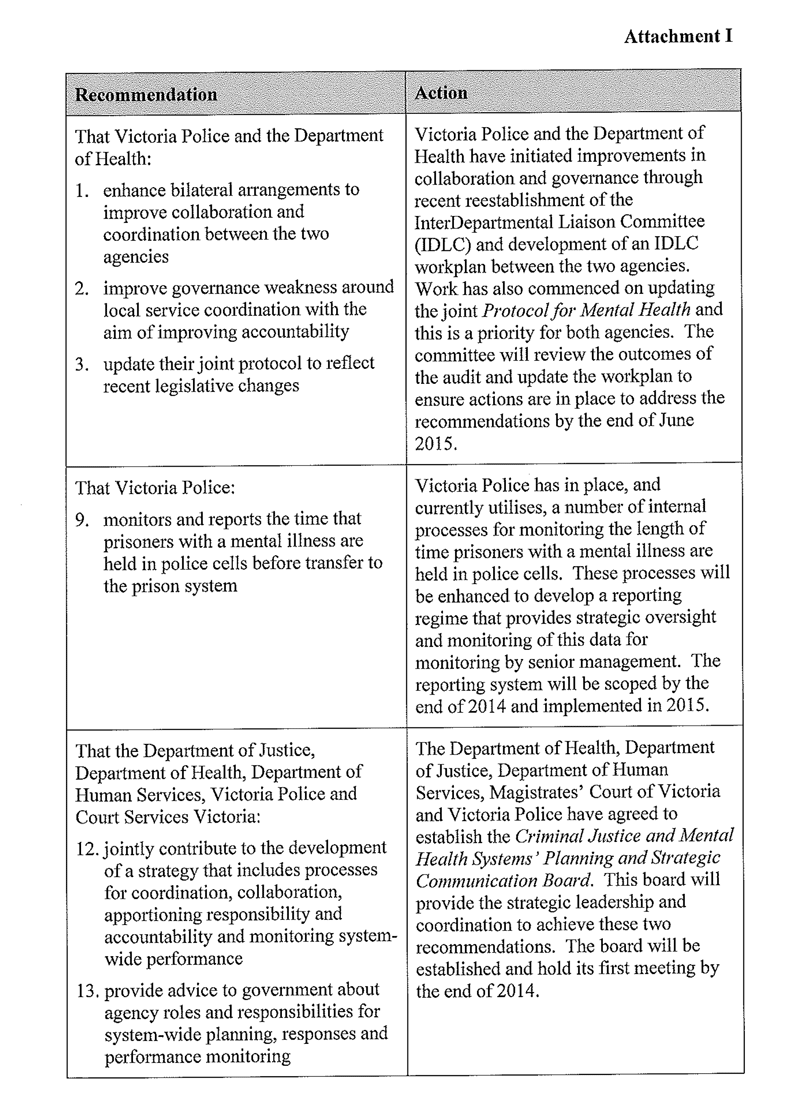
RESPONSE provided by the Chief Executive Officer, Magistrates' Court of Victoria, incorporating Court Services Victoria's response