Victorian Public Hospital Operating Theatre Efficiency
Overview
Demand for surgery is rising in response to a growing and ageing population. Health services need to run their operating theatres as efficiently as possible if they are to meet this rising demand, and reduce waiting lists, with their current resources. They also need to balance competing demands from elective surgery and emergency surgery for limited theatre resources.
The Department of Health and Human Services (DHHS) oversees and funds health services to deliver surgery and other treatment. DHHS leads health system planning, including capital investment and funding allocation to hospitals.
In this audit, we examined whether Victoria’s operating theatres are being used efficiently and whether DHHS’s leadership of the health system is driving efficiency. We audited DHHS and four health services—Alfred Health, Austin Health, Melbourne Health and St Vincent’s Hospital Melbourne.
In the course of this audit, we compiled a new dataset that enabled new performance analysis and benchmarking not previously available in Victoria. We also examined policy and reporting documentation used by the health services and DHHS.
We made 11 recommendations in this audit—10 for DHHS and one for health services.
Transmittal letter
Ordered to be printed
VICTORIAN GOVERNMENT PRINTER October 2017
PP No 336, Session 2014–17
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report Victorian Public Hospital Operating Theatre Efficiency.
Yours faithfully
Andrew Greaves
Auditor-General
18 October 2017
Acronyms
| ABF | Activity-based funding |
| AIHW | Australian Institute of Health and Welfare |
| DHHS | Department of Health and Human Services |
| ENT | Ear, nose and throat |
| ESIS | Elective Surgery Information System |
| GP | General practitioner |
| HSA | Health Services Act 1988 |
| IT | Information technology |
| KPI | Key performance indicator |
| SOP | Statement of Priorities |
| SVHM | St Vincent’s Hospital Melbourne |
| VAED | Victorian Admitted Episodes Dataset |
| VAGO | Victorian Auditor-General’s Office |
| VCDC | Victorian Cost Data Collection |
| VEMD | Victorian Emergency Minimum Dataset |
| VINAH | Victorian Integrated Non-Admitted Health |
| WIES | Weighted Inlier Equivalent Separation |
Audit overview
Demand for surgery is rising in response to a growing and ageing population. Health services need to run their operating theatres as efficiently as possible if they are to meet this rising demand, and reduce waiting lists, with their current resources. They also need to balance competing demands from elective surgery and emergency surgery for limited theatre resources.
According to data from 23 health services recorded in Victoria's Elective Surgery Information System (ESIS), demand for elective surgery has increased by 12 per cent over the five years to 2015–16.
The Department of Health and Human Services (DHHS) oversees and funds health services to deliver surgery and other treatment. DHHS leads health system planning, including capital investment and funding allocation to hospitals. DHHS has significant influence on health services' performance as it determines their targets and budgets, and controls infrastructure development.
In this audit, we examined whether Victoria's operating theatres are being used efficiently and whether DHHS's leadership of the health system is driving efficiency. We audited DHHS and four health services—Alfred Health, Austin Health, Melbourne Health and St Vincent's Hospital Melbourne (SVHM). We chose to audit four tertiary hospitals—offering specialist care and catering for complex health needs—because they form a cohort with similar characteristics, which enabled us to compare their practices.
In the course of this audit, we compiled a new dataset that enabled new performance analysis and benchmarking not previously available in Victoria. We also examined policy and reporting documentation used by the health services and DHHS.
Conclusion
Operating theatres are an under-utilised resource across the system. As a result, the costs of surgery are higher than they need to be. More could be done with existing resources, to achieve reduced elective surgery wait times and shorter waiting lists.
Operating theatres are sitting idle for significant periods of time within planned surgical sessions because of late starts and early finishes. Health services need to focus more management attention on factors within their control and collect better performance data.
Current funding arrangements and patient preferences present barriers to health services optimising their operating theatre efficiency. DHHS, as system manager of the health sector, needs to reconsider how it funds health services to ensure that hospitals are encouraged to fully utilise operating theatres.
There are opportunities for DHHS and health services to improve operating theatre efficiency and access to surgery for patients.
Findings
The productive efficiency of operating theatres
We collected operating theatre data from 23 health services from 1 July 2014 to 31 December 2016, which we collated into a new dataset so we could evaluate efficiency across a range of measures. We found that, although the state average is generally good, there is significant variation between health services, as shown in Figure A.
Figure A
Variation in efficiency between health services
|
Health service |
Utilisation rate(a) |
Unused capacity(b) |
Salary cost per hour of surgery |
|---|---|---|---|
|
Top five health services |
87% |
2.5% |
$1 672 |
|
Bottom five health services |
75% |
22% |
$2 282 |
(a) Utilisation rate is based on anaesthetic start to anaesthetic stop timestamps for elective surgery conducted from 1 July 2014 to 31 December 2016.
(b) Unused capacity is for 1 July 2016 to 31 December 2016.
Source: VAGO, based on health services' data.
There are opportunities for improvement across a range of underlying measures that test the efficiency of health services' practices. Each health service could improve efficiency in at least one area. During the time period we looked at, we noted in particular that across Victoria:
- 55 per cent of elective surgical sessions began more than 20 minutes late
- 10 per cent of elective surgical sessions finished more than 90 minutes early.
Despite health services demonstrably trying to improve their productive efficiency, inefficiencies still persist. Health services have attempted to address the problem of surgical sessions starting late by redesigning processes and providing feedback to staff. However, improvements have only been maintained while management keeps focusing on these specific issues.
Health services are using theatres on 90.5 per cent of business days. There is limited spare theatre capacity in metropolitan hospitals, with most spare capacity available in regional hospitals. Health services operating at high capacity will need to use their theatres more efficiently if they are to meet rising demand.
Monitoring operating theatre efficiency
DHHS has set the efficient use of resources as a goal for itself and for health services. However, DHHS cannot evaluate Victoria's operating theatre efficiency because it lacks the required data. It also lacks suitable performance targets for evaluating operating theatre performance.
Health services use varying measures of theatre efficiency, which makes evaluation and comparison difficult. Health services' information technology (IT) systems and processes for capturing data also vary significantly, which affects their ability to report accurately on theatre performance.
As a result, the health sector is limiting its own efforts to improve efficiency, because it cannot systematically identify efficient practice. Without a centralised dataset, benchmarks and monitoring, DHHS and health services are unable to effectively assess how each health service performs compared to its peers and the state average. DHHS and health services are therefore missing opportunities to identify poor and better practice, and to use that information to improve access to surgery in Victoria.
Sharing better practice
We found examples of better practice that, if evaluated and disseminated, could help other health services improve the efficiency of their operating theatres. However, there is no structured forum for health services to share information on better practice initiatives. Information exchange is currently ad hoc and primarily due to staff of different health services sharing information through their professional relationships.
Allocating theatre resources
Health services' resource allocation models
To allocate resources effectively, health services need to evaluate historical data and forecast demand for emergency surgery and non-surgical admissions. They also need to plan elective surgery to meet performance targets for their waiting list and access to surgery.
We found that health services use a significant amount of data when allocating their theatre resources and have developed individualised reporting to understand their business. However, the policies they use to underpin decision‑making provide limited guidance on important aspects of resource distribution, such as allocating resources between surgery types. Consequently, health services rely heavily on their managers' knowledge and experience to allocate resources efficiently. Without documented policies, health services cannot effectively evaluate the quality of this decision-making and risk losing corporate knowledge as staff change.
Victoria's health services manage their operating theatres using different resource allocation models, due to variations in their infrastructure, case load, staff profile and historical precedent. In particular, health services vary significantly in how they manage the competition for resources between emergency and elective surgery. Among the audited health services, Alfred Health and Austin Health have the infrastructure to physically separate emergency and elective streams, which correlates with lower overrun sessions across both surgery streams.
We found minimal benchmarking and limited evidence of health services evaluating how their chosen model for allocating resources affects outcomes. This increases the risk that health services are using historical resource allocation models that do not maximise access to surgery.
DHHS's resource allocation model
DHHS is responsible for ensuring that the health system has sufficient operating theatre capacity and funding to enable timely access for Victorians to surgery. DHHS policies also list the efficient operation of the health system as a key goal.
We found that DHHS does not have a dataset to identify theatre capacity usage or theatre efficiency, which inhibits its understanding of Victoria's operating theatre performance. As a result, DHHS is unable to provide targeted support to health services to improve efficiency or reallocate the health budget to better use existing capacity.
DHHS measures the number of people waiting for public hospital elective surgery and the proportion of patients who receive treatment within clinically recommended time frames to evaluate whether the 'right' amount of elective surgery is available to the Victorian public. However, the data DHHS uses to forecast demand and plan delivery is incomplete as it does not include people waiting for surgery at small regional health services who represent 15 per cent of all elective surgery patients. It also does not account for how the waiting list for specialist appointments across the health system affects the elective surgery waiting list. DHHS therefore risks misallocating resources as it increases theatre capacity and allocates budgets to health services.
Due to current funding levels, the elective surgery waiting list remains relatively constant each year. However, Victoria is not meeting its access targets for patients waiting for semi-urgent and non-urgent elective surgery.
DHHS began recording emergency surgery start times in 2016–17 and provided some performance information to health services. As yet, there are no timeliness or access targets for emergency surgery nor public reporting. DHHS's analysis does not clearly identify how resource allocation between emergency and elective surgery affects Victorians' access to surgery. This increases the risk that Victorians will wait longer than the clinically recommended time frames for surgery.
We found significant variation between health services:
- Access by clinical need varies significantly between health services and fluctuates throughout the year. Figure B shows how the highest and lowest access rates changed over 2016–17.
- Access to each type of surgery varies between health services, with the median waiting time being up to twice as long for the same surgery at different health services.
- There is no measure for access to emergency surgery that categorises patients' access within clinically recommended time frames.
Figure B
Category 2 (semi-urgent) elective surgery patients treated within 90 days in 2016–17
Source: VAGO, compiled from DHHS performance data.
To achieve DHHS's efficiency objective, the funding model needs to encourage health services to use their resources efficiently.
Health services' internal reporting focuses strongly on meeting DHHS targets and delivering activity levels that will maximise the amount of funding they can receive.
DHHS funds health services up to 104 per cent of their final activity cap. In 2015–16, 19 of the 23 health services delivered activity at 99–105 per cent of their initial cap. The other four finished at 95–98 per cent of their initial cap. While capping funding controls spending on health, it also reduces the incentive for health services to be more productively efficient because they cannot increase their revenue above the cap.
Recommendations
We recommend that the Department of Health and Human Services, in collaboration with health services:
- implement an agreed suite of definitions, measures and targets for theatre efficiency that target the underlying causes of inefficiency (see Section 4.3)
- issue mandatory data quality standards for operating theatre data to ensure consistency in the data captured by health services (see Section 4.3)
- develop a centralised dataset for operating theatre data, to inform decision‑making at the Department of Health and Human Services (see Section 4.3)
- disseminate operating theatre data to health services in a form that enables them to evaluate and benchmark their performance and identify sector best practice (see Section 4.3)
- establish a regular sector-led, multidisciplinary forum focused on sharing information and practices that improve the efficiency of operating theatres (see Section 4.3)
- work with the sector to improve productive efficiency at the theatre level, particularly to reduce late starts and underruns (see Section 4.3)
- develop and implement emergency surgery access measures (see Section 4.2)
- analyse and forecast the impact of budget allocations on category 2 and 3 surgery access indicators (see Section 4.3)
- review the current process for setting funding caps, to ensure caps are based on a comprehensive assessment of demand, capacity and performance measures (see Section 4.3)
- review current operating theatre management guidance provided to health services to incorporate better practice, to drive theatre efficiency (see Section 4.3).
We recommend that the audited health services:
- 11. formalise governance policies to guide decision-makers when allocating theatre resources between emergency and elective surgery and between surgical specialities (see Section 3.2).
Responses to recommendations
We have consulted with DHHS, Alfred Health, Austin Health, Melbourne Health and SVHM, and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report to those agencies and asked for their submissions and comments. We also provided a copy of the report to the Department of Premier and Cabinet.
The following is a summary of those responses. The full responses are included in Appendix A.
DHHS agrees with the findings in the report focusing on the importance of benchmarking data to drive performance. DHHS has accepted nine of the 10 recommendations directed at it, and accepted recommendation 3 in principle. DHHS will explore options for responding to recommendation 3.
Alfred Health plans to review its policies in line with recommendation 11 and looks forward to working with DHHS on the other recommendations.
Austin Health is undertaking an improvement project focused on theatre efficiency and utilisation, including reviewing governance structures and policies. It is also looking forward to working with DHHS on the recommendations in this report.
Melbourne Health and SVHM did not provide a formal response for inclusion in this report.
1 Audit context
The Health Services Act 1988 (HSA) establishes Victoria's public health services as independent legal entities that operate at 'arm's length' from DHHS.
In this system of devolved governance, boards appointed by the Minister for Health are responsible for the efficient and effective management of health services. DHHS's role is to fund, monitor and evaluate healthcare delivery. DHHS also retains responsibility for the sector's ongoing capital investment, including building new operating theatres.
While DHHS sets health services' budgets and targets, the boards are responsible for achieving the targets. This includes providing elective and emergency surgery, allocating resources and employing staff. The devolved system therefore allows health services to make 'local decisions for local needs', including on how best to manage their operating theatres.
In 2016–17, 60 health services delivered surgery in 295 operating theatres. In 2015–16, 17 per cent of all hospital admissions involved surgery, as outlined in Figure 1A.
Figure 1A
Healthcare provided by Victorian public hospitals in 2015–16
|
Healthcare |
Number |
Percentage of admissions |
|---|---|---|
|
Elective admissions involving surgery |
217 203 |
13% |
|
Emergency admissions involving surgery |
68 262 |
4% |
|
Admissions not involving surgery |
1 384 097 |
83% |
|
Total number of patients treated (surgical and other) |
1 669 562 |
100% |
Source: VAGO, based on Australian Institute of Health and Welfare, Admitted patient care 2015−16: Australian hospital statistics.
Operating theatres are part of a hospital's infrastructure, along with specialist clinics, emergency departments, intensive care units and hospital wards. Clinical staff—including surgeons, anaesthetists, nurses and technicians—and other support teams deliver surgical services. These components must be available and coordinated for a theatre to run efficiently, so it is important to consider the hospital holistically when assessing operating theatre performance. In this audit, we have focused on fully equipped operating theatres only, and we have not reported on the use of procedure rooms.
Figure 1B shows the paths patients take through a health service, depending on whether they need elective or emergency surgery.
Figure 1B
Flowchart of surgical services
Note: 'Emergency direct' refers to an emergency patient who is transferred from a lower to higher acuity hospital.
Source: VAGO, based on DHHS, A guide to surgical services redesign: measures for improvement.
The Australian Institute of Health and Welfare (AIHW) defines the two streams:
- Elective surgery—planned surgery that can be booked in advance as a result of a specialist clinical assessment resulting in placement on an elective surgery waiting list.
- Emergency surgery—surgery to treat trauma or acute illness following an emergency presentation. The patient may require immediate surgery or may present for surgery at a later time following this unplanned presentation. This includes instances where a patient leaves hospital and returns for a subsequent admission. Emergency surgery includes unplanned surgery for admitted patients and unplanned surgery for patients already awaiting an elective surgery procedure—for example, in cases of acute deterioration of an existing condition.
1.1 Surgery targets and access in Victoria
Each year DHHS negotiates a Statement of Priorities (SOP) with each health service. SOPs outline budgets, waiting list targets, access measures, and safety and quality indicators for each health service.
DHHS sets targets for elective surgery waiting list numbers and access to treatment within clinically recommended time frames. Figure 1C shows DHHS's key performance indicators (KPI) for elective surgery 'access and timeliness'. Health services and DHHS report performance against these targets in their annual reports.
Figure 1C
Elective surgery access and timeliness KPIs in health services' 2016–17 SOPs
|
KPI |
Description |
Target |
|---|---|---|
|
Category 1 admit |
Percentage of category 1 (urgent) elective surgery patients admitted within 30 days |
100% |
|
Category 1, 2 and 3 admit |
Percentage of category 1 (urgent), 2 (semi-urgent) and 3 (non-urgent) elective surgery patients admitted within clinically recommended time frame |
94% |
|
Longest waiting elective surgery patients |
20 per cent longest waiting urgency category 2 and 20 per cent longest waiting category 3 patient removals from the elective surgery waiting list |
100% |
|
Elective surgery waiting list |
Number of patients on the elective surgery waiting list |
Specific to individual health services |
|
Hospital-initiated postponements |
Number of hospital-initiated postponements per 100 scheduled elective surgery admissions |
Less than 8 out of 100 |
|
Admissions |
Number of patients admitted from the elective surgery waiting list |
Specific to individual health services |
Note: Surgery categories 1, 2 and 3 are defined in Figure 1F.
Source: VAGO, compiled from health services' statement of priorities 2016–17.
DHHS uses the elective surgery waiting list to monitor the demand for elective surgery in Victoria. It collates the state waiting list from data provided by the 23 health services that report to DHHS's Elective Surgery Information System (ESIS). The 37 health services not included in the ESIS dataset are small regional health services. DHHS excludes these health services, which represent 15 per cent of elective surgery cases, to release them from the administrative burden that reporting would place on them.
Figure 1D shows the 23 ESIS health services, the number of theatres that each health service runs, and their elective surgery access results for 2015–16.
Figure 1D
Map of health services across Victoria
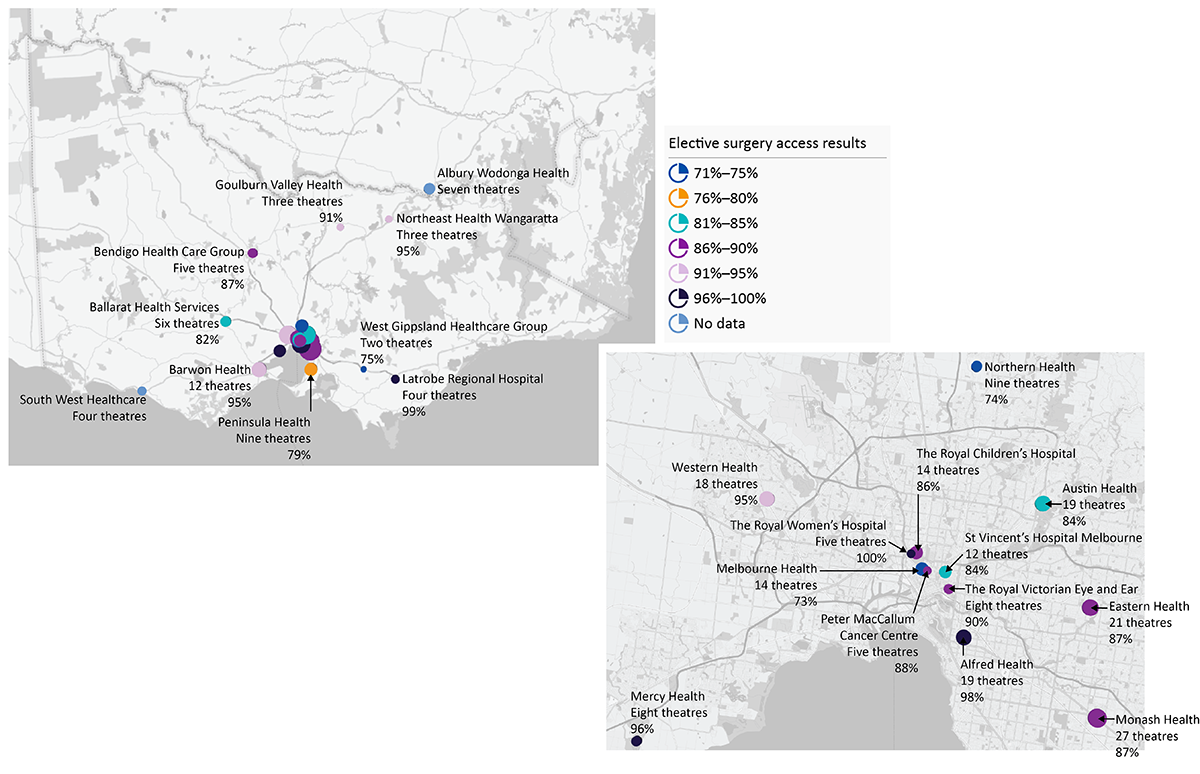
Note: In 2016–17, Albury Wodonga Health Service and South West Healthcare joined ESIS.
Source: Complied by VAGO. Theatre numbers are based on DHHS data. Access levels are compiled from health services' 2015–16 annual reports.
The number of people on the elective surgery waiting list increases or decreases based on additions—surgical registrations—and removals, as well as the number of health services contributing their data to ESIS. Removals occur for various reasons, mainly due to patients receiving elective surgery.
Figure 1E shows elective surgery waiting list numbers over time and highlights the relationship between additions and removals. The waiting list target for 2016−17 was 38 498.
Figure 1E
Elective surgery registrations and removals from the waiting list
Note: The waiting list at 30 June 2012 was not reported in the former Department of Health's annual report for 2011–12, so there is no comparable data for this period.
Source: VAGO, based on DHHS data.
Elective surgery patients are categorised by clinical urgency, as shown in Figure 1F. These categories are consistent nationally and indicate the recommended time frame in which health services should treat patients. Health services report their results, and Victoria's performance overall is reported at state and federal levels.
Figure 1F
Elective surgery clinical categorisation definitions
|
Clinical category |
Recommended time frame in which treatment should occur |
|---|---|
|
Category 1 (urgent) |
30 days |
|
Category 2 (semi-urgent) |
90 days |
|
Category 3 (non-urgent) |
365 days |
Source: VAGO, based on DHHS elective surgery access policy.
In 2015–16, Victoria met its category 1 target of 100 per cent, although Victoria's performance lags behind comparable states for category 2 and category 3 patients, as shown in Figure 1G.
Figure 1G
Proportion of patients treated within clinically recommended time frames
Source: VAGO, based on AIHW, Elective surgery waiting times 2015–16: Australian hospital statistics.
AIHW collects data from each state and territory to report on health services' performance nationally. Figure 1H shows that Victoria's performance is comparable when considering the wait time for patients at the 50th and 90th percentiles. AIHW does not report on access to emergency surgery, as there are no nationally agreed measures.
Figure 1H
Elective surgery, time to admission (days), 2015–16
Source: VAGO, based on AIHW, Elective surgery waiting times 2015–16: Australian hospital statistics.
1.2 Funding surgery
The Victorian State Budget allocated $11.8 billion to acute health services in 2016–17 and $13.1 billion in 2017–18. Figure 1I shows that the acute health services' budget has grown significantly from 2011–12 to 2015–16.
Figure 1I
Victoria's budget allocation for acute health services
Source: VAGO, based on State Budget papers and DHHS ESIS data.
Funding for surgery is included within the budget for acute health services—there is no budget specifically allocated to surgery. However, the Victorian Government regularly funds budget initiatives to increase the delivery of elective surgery, as shown in Figure 1J.
Figure 1J
State Budgets' priority focus on elective surgery
|
Budget year |
Name of initiative |
Funding promise |
|---|---|---|
|
2012–13 |
Sustaining hospital performance—maintaining elective surgery capacity |
$44 million |
|
Sustaining hospital performance—ongoing elective surgery |
$149.8 million over four years |
|
|
2013–14 |
Securing Victoria's health system—elective surgery |
$420.6 million over four years |
|
2014–15 |
Boosting elective surgery capacity |
$190.1 million over four years |
|
2015–16 |
Elective surgery boost |
$60 million |
|
2016–17 |
Improving access to elective surgery |
$335.2 million over five years |
Source: VAGO, based on State Budget papers.
DHHS funding is a combination of state and Commonwealth money, as shown in Figure 1K.
Figure 1K
Commonwealth and state funding for health services
Source: VAGO, based on DHHS, Policy and funding guidelines, 2016.
Activity-based funding
DHHS provides activity-based funding (ABF) and fixed funding to health services.
ABF funds health services for the treatment—or 'activity'—they deliver. There are multiple streams—including acute admitted care, which funds most elective and emergency surgery.
In setting the budget for acute admitted care, DHHS considers:
- the state's elective surgery waiting list target
- its overall financial constraints
- the sector's previous performance
- capacity changes, such as new operating theatres
- forecast growth in demand
- its responsibilities in other areas of healthcare.
Health services receive a Weighted Inlier Equivalent Separation (WIES) payment for each patient treated or 'separated' from the hospital. A 'separation' refers to the patient's journey from admission to discharge. The WIES number of units paid for a patient is adjusted—or 'weighted'—according to a patient's condition, treatment and length of stay. DHHS pays a set price for each WIES unit, which was $4 640 in 2016–17. DHHS resets the WIES price and its weightings annually to reflect changing hospital costs.
Capping activity-based funding levels
A health service's WIES cap is the maximum amount of WIES units DHHS agrees to fund. There are multiple categories of WIES, and each category attracts a different payment. The two main categories are:
- WIES public—for patients who are using only the public system
- WIES private—a lower payment for patients who use their private health insurance for their treatment in a public hospital.
The WIES cap influences the numbers of patients health services are funded to treat. DHHS funds activity delivered within a health service's cap at the full WIES price, and funds activity between 100 and 104 per cent of the cap at 50 per cent of the WIES price. Any further activity is unfunded unless DHHS adjusts the health service's WIES cap during the year.
In 2015–16, surgical separations consumed 54 per cent of the ESIS health services' WIES public and private funding allocation. The amount varied by peer group, as shown in Figure 1L. This is due to health services managing varying case loads. The remainder of the cap was used on patients requiring treatment other than surgery.
Figure 1L
Percentage of WIES public and private cap attributed to surgical separations, 2015–16
Note: Data was calculated by comparing total WIES public and private units funded for surgical separations from the Victorian Admitted Episodes Dataset (VAED) compared to the total WIES public and private funding caps identified in health services' annual reports.
Source: VAGO, based on DHHS VAED data and health services' 2015–16 annual reports.
1.3 Why this audit is important
Victoria's health system faces rising demand for surgical services from a growing and ageing population, which is increasing pressure on health services and the State Budget to maintain or improve access. Victoria's health system needs to use its resources—including operating theatres—efficiently to maintain or improve standards as demand rises.
This audit builds on our previous hospital efficiency audits, particularly the Efficiency and Effectiveness of Hospital Performance: Emergency Care and the Hospital Performance: Length of Stay audits in 2016. It continues our theme of examining hospital-level efficiency and how DHHS fulfils its role as system manager.
Recent audits of operating theatre efficiency in New South Wales, Western Australia and Queensland have all identified barriers to the efficient use of operating theatres. In this audit, we examine these barriers and the measures of efficiency in Victoria.
1.4 What this audit examined and how
The objective of the audit was to determine whether Victoria's public hospitals optimise their use of operating theatres to undertake surgery.
To address this objective we examined:
- the use of data to assess efficient performance
- the allocation of theatre resources between competing priorities
- how management and funding of the system encourage efficient performance.
The audited entities were DHHS and four health services—Alfred Health, Austin Health, Melbourne Health and SVHM. We chose to audit four tertiary hospitals—offering specialist care and catering for complex health needs—because they form a cohort with similar characteristics. This enabled us to compare their performance and practices.
We obtained operating theatre data from the 23 Victorian health services in ESIS to create a new dataset to measure theatre efficiency. In many of the report's charts, we have used anonymous letters to refer to the health services not included in the audit but from whom we obtained data. We added elements of DHHS's datasets and the health services' financial data to the operating theatre data to conduct the analysis in this report. We collected operating theatre data for 2014–15, 2015–16 and the first half of 2016–17 from health services. DHHS's data and health services' financial data covered 2014–15 and 2015–16.
In collating the data, we conducted detailed analysis to link the data accurately and remove identifiable errors.
Using the new dataset, we were able to create a dashboard to analyse health system performance in multiple ways not previously undertaken in Victoria. The dashboard enables users to analyse the efficiency of the healthcare system, health services, hospitals, theatres, specialities and surgeons.
We reviewed available legislation, policy guidance and industry standards for operating theatre efficiency in Victoria and other Australian jurisdictions.
We carried out this audit in accordance with section 15 of the Audit Act 1994 and the Australian Auditing and Assurance Standards. The total cost of the audit was $955 000.
1.5 Definitions
Throughout the audit, we used two definitions of efficiency—productive efficiency and allocative efficiency—derived from AIHW and the Productivity Commission. We identified various measurements, as shown in Figure 1M.
Figure 1M
Measures and definitions of efficiency for operating theatres
|
Measure |
Description |
|
|---|---|---|
|
Productive efficiency |
||
|
Utilisation rate |
The proportion of time surgery is performed during a planned surgical session |
|
|
Cost per hour |
The average salary cost of performing an hour of surgery |
|
|
Length of surgery |
The relative length of an operation occurring at different health services |
|
|
Unused capacity |
The number of business days on which an operating theatre is closed |
|
|
Allocative efficiency |
||
|
Access between types of surgery |
Comparative access to different types of surgery in Victoria |
|
|
Access between health services |
Comparative access to surgery at different health services |
|
Source: VAGO, based on AIHW and Productivity Commission definitions.
Productive efficiency requires health services to use their theatre resources to perform the most surgery possible. Allocative efficiency ensures timely access to surgery for patients across a range of factors, including:
- resource levels to meet demand for surgery
- theatre resources balanced between elective and emergency streams
- equity between patients for different types of surgery with similar clinical urgency, regardless of the health service where they seek treatment.
DHHS analyses the effect of different resource levels on surgery numbers. The government then uses this analysis, along with other relevant information, to set the health budget at a level it considers will enable allocative efficiency.
DHHS allocates funding to health services to deliver the state's surgery targets—elective surgery waiting list numbers and access targets. DHHS's success in allocating the right amount of resources is measured by changes to the elective surgery waiting list and the proportion of patients who receive treatment within clinically recommended time frames. The state does not have explicit targets for emergency surgery efficiency, but does forecast growth in demand for emergency surgery.
1.6 Report structure
The remainder of this report is structured as follows:
- Part 2 looks at the productive and allocative efficiency of operating theatres in Victoria's public hospitals, with a key focus on data analysis
- Part 3 looks at whether the management practices of health services lead to the efficient use of operating theatre resources
- Part 4 looks at how system design at the health service and health system levels contribute to the efficient use of Victoria's operating theatres.
2 Current performance levels
In this part of the report, we analyse the productive efficiency of operating theatres in Victoria's public hospitals. For this purpose, we have identified various measures of productive efficiency, as shown in Figure 2A.
Figure 2A
Measures of productive efficiency for operating theatres
|
Measure |
Description |
|---|---|
|
Utilisation rate |
The proportion of time surgery is performed during a planned surgical session |
|
Cost per hour |
The average salary cost of performing an hour of surgery |
|
Length of surgery |
The relative length of an operation occurring at different health services |
|
Unused capacity |
The number of business days on which an operating theatre is closed |
Source: VAGO.
Theatre resource inputs include:
- physical assets—operating theatres and equipment
- surgical consumables—such as prostheses and pharmaceuticals
- clinical staff—surgeons, anaesthetists, nurses and technicians
- management overheads—such as executive staff involved in surgical planning.
2.1 Conclusion
Health services are hindered by practices and system features that inhibit productivity gains. Health services can improve their productive efficiency by minimising idle time during surgical sessions and by maximising the time that their theatres are available for surgery. This would reduce their average cost of surgery and is likely to reduce elective surgery wait times and waiting lists.
Late starts and underruns contribute most to inefficient practice at health services. Both can be reduced by more focused management attention, including providing individuals with targeted feedback on their performance backed by reliable data.
More effective system-wide management of the health system is also needed. There are no mandatory standardised data definitions or efficiency performance targets and, therefore, no valid benchmarking. There is also no central oversight of unused theatre capacity or of theatre utilisation rates, and the current funding model does not provide incentives for health services to use their unused capacity.
2.2 Utilisation rate
The utilisation rate is the proportion of time in a surgical session that the operations—anaesthetic processes and surgery—are actually occurring.
A surgical session is the rostered time when surgeons, anaesthetists, nurses and other staff are in the theatre and available to perform surgery. Staff are rostered in either part-day or full-day sessions.
Higher utilisation rates generally result in more operations being performed within a surgical session for the same salary costs—as staff are paid whether they are performing surgery or not—and reduced waiting lists and wait times for surgery.
Current utilisation performance
Health services have developed their own methods for collecting performance data and have different performance measures and IT systems. We have factored these differences into our analysis and, where necessary, have excluded some health services if we could not link their data consistently with that of the others.
Due to variations in practice, we report two elective surgery utilisation rates for Victoria to enable comparisons, as described in Figure 2B. We calculated Victoria's public hospital operating theatre utilisation rate as 74 per cent—if measured from 'anaesthetic start to surgery stop'—or 80 per cent—if measured from 'anaesthetic start to anaesthetic stop'.
Figure 2B
Theatre utilisation—elective surgery session performance for Victoria
|
Utilisation measure |
Description |
Utilisation rate |
|---|---|---|
|
Anaesthetic start to surgery stop(a) |
From when the anaesthetist starts working on the patient until the surgeon finishes the operation. All health services provided data to enable this measurement. |
74% |
|
Anaesthetic start to anaesthetic stop |
From when the anaesthetist starts working on the patient until he or she releases control of the patient after surgery. Not all health services provided an 'anaesthetic stop' timestamp. |
80% |
(a) This measure under-reports the actual utilisation rate as it excludes the anaesthetists' work that occurs after surgery in theatre.
Source: VAGO.
When disaggregated, we observe variations in utilisation rates between peer groups, shown in Figure 2C, and between individual health services, shown in Figure 2D.
Figure 2C
Utilisation rate for elective surgery sessions, by peer group, 1 July 2014 to 31 December 2016
Note: A peer group comprises health services of similar size, location and capability.
Source: VAGO.
Figure 2D
Utilisation rate for elective surgery sessions, by health service, 1 July 2014 to 31 December 2016
Note: All health services provided a 'procedure stop' timestamp, although not all provided the 'anaesthetic stop' timestamp. Austin Health collect an 'out of room' timestamp to measure the end of a procedure, however this was not included in the dataset we compiled.
Note: Some operating theatres at Melbourne Health and Alfred Health do not have anaesthetic bays attached, which lowers utilisation rate because a patient cannot begin the anaesthetic process while the previous surgery is underway.
Source: VAGO, based on health services' operating theatre data.
We have excluded emergency surgery and non-business day elective sessions from our calculations for several reasons:
- Health services must provide access to emergency surgery based on need. Access and utilisation rates are correlated with each other and driven by the amount of theatre resources health services dedicate to emergency surgery—a high resource allocation will improve access but reduce utilisation rate.
- Health services deliver different amounts of emergency surgery, so performance cannot be reliably compared when emergency sessions are included.
- The efficiency of an elective surgery session is within the control of the health service, whereas the efficiency of an emergency surgery session is not. Assessing performance against elective sessions is a more reliable gauge of theatre management.
- Scheduling elective surgery sessions on a non-business day—such as a weekend—is irregular and health services perform different amounts. We excluded these sessions to improve comparability.
Factors that drive utilisation rates
Victorian hospitals have a range of different theatre infrastructure. A health service's infrastructure influences its theatre utilisation rate—particularly if its operating theatres have separate anaesthetic rooms. These enable anaesthetists to begin working on patients while earlier surgery sessions are still underway.
Other key issues that affect utilisation rates are:
- the first case of a session not starting on time
- unreasonably long turnaround times between surgeries
- a session underrunning its allocated time because the final case finishes before the session's closing time
- a session overrunning its scheduled finishing time.
If health services improve their performance against these factors, they increase their capacity to provide more surgery within existing resources, as they pay staff for an entire surgical session regardless of their productivity.
Figure 2E shows that late starts and underruns are the two key drivers of idle capacity—more than 75 per cent start more than 15 minutes late at the positioning and preparation stage, and 55 per cent of sessions underrun by an average of half an hour.
Figure 2E
Underlying factors affecting utilisation rate, 1 July 2014 to 31 December 2016
| Factor |
First case start |
Percentage of cases |
Average time (minutes) |
|||
|---|---|---|---|---|---|---|
|
0–15 minutes |
15–30 minutes |
30–45 minutes |
>45 minutes |
|||
|
Procedure step |
||||||
|
Anaesthetic start |
30.1% |
31.2% |
23.7% |
15.1% |
||
|
Positioning and preparing the patient |
24.0% |
38.0% |
24.9% |
13.0% |
||
|
Surgery start |
12.2% |
40.0% |
33.0% |
14.8% |
||
|
Turnaround time |
||||||
|
From procedure stop |
21.0 |
|||||
|
From anaesthetic stop |
17.5 |
|||||
|
Underruns and overruns |
||||||
|
Underrun |
55.3% |
31.8 |
||||
|
Overrun |
16.4% |
12.0 |
||||
Source: VAGO.
If a four-hour surgical session starts 20 minutes late and finishes 30 minutes early, then more than one-fifth of the entire session is unused and theatre staff are being paid for their presence but not their work.
We expected to find that late starts correlate strongly with fewer underruns and more overruns (or more cancellations), reasoning that starting late may cause surgeons to overrun their scheduled session or cancel elective surgery.
What we found was health services with high incidences of both late starts and underruns. This indicates that these health services construct surgical lists with a time buffer to avoid running late or cancelling surgery. In doing so, they enable these inefficient practices to persist without addressing the causes of wasted surgical time.
Health services' results against common efficiency performance indicators are shown in Appendix F.
Late starts
A surgical session 'starts late' if the first operation does not begin at the session's commencement. Health services have different theatre infrastructure, timestamp definitions and IT systems, which influence how they measure their late start performance. In particular, we found that health services use different points in the procedure to assess performance, which inhibits comparison.
We analysed late starts at three different points in the procedure:
- anaesthetic start—when the anaesthesia process begins, shown in Figure 2F
- positioning and preparation—when the patient is prepared by the surgical team for surgery in the theatre, shown in Figure 2G
- surgery start—this measure varies between health services, as they have different definitions for when surgery has started, shown in Figure 2H.
These charts show the proportion of cases that started in each five-minute block after the surgical session began. The darker the box, the higher the percentage of cases begun in that time block. Ideally, the charts should be darker to the left and lighter to the right—Figure 2F exhibits this pattern, but Figure 2H does not.
Health services have cited management focus and the provision of data‑supported performance feedback as key drivers in reducing late starts.
Among the audited health services, Alfred Health demonstrated the strongest performance in minimising late starts, with 45 per cent of its surgery beginning within 20 minutes of the scheduled session start. Alfred Health staff advised that the key to this result was to provide data-driven feedback that attributes personal responsibility and accountability for timeliness to staff when appropriate.
Figure 2F
Percentage of cases when anaesthetic has started, relative to session start time (minutes), 1 July 2014 to 31 December 2016 (elective sessions only)
Source: VAGO.
Figure 2G
Percentage of cases when the patient is being positioned and prepared in theatre, relative to session start time (minutes), 1 July 2014 to 31 December 2016 (elective sessions only)
Source: VAGO.
Figure 2H
Proportion of cases when surgery has started, relative to session start time (minutes), 1 July 2014 to 31 December 2016 (elective sessions only)
Source: VAGO.
Reasons for late starts
Most health services can record the reason a session started late, depending on their IT system. We have identified two key flaws in health services' current practices for capturing this data:
- the health service does not capture the reasons for late starts
- the reasons captured do not identify whether the delay was within the control of the health service.
This lack of clarity means health services cannot always identify the reason for a delay, which hampers their efforts to improve performance.
For sessions with a recorded reason for the delay, 81 per cent were within the health services' control, as shown in Figure 2I. The reasons given for the other 19 per cent of delays were either not specific enough, or were outside health services' control.
The surgeon being late to the session is the most common reason for sessions starting late. The audited health services reported that they have governance arrangements to provide feedback to surgeons via department heads if they identify a performance issue with a surgeon. However, the prevalence of this issue across the sector indicates that current practices are not driving changes in behaviour.
Between December 2014 and May 2015, Austin Health audited its late starts against a 15-minute threshold. Surgeon lateness caused 27 per cent of their delays and was the leading driver of theatre inefficiency. Austin Health discussed the data with the surgeons involved and identified that early morning meetings frequently delayed on-time starts. To rectify this, management adjusted surgeons' start times and rescheduled meetings.
Austin Health's late start audits further emphasise the importance of accurate data entry. Despite exceeding the 15-minute buffer, 23 per cent of delayed sessions were recorded as 'started on time'. This hinders accurate analysis of the data, making trends difficult to identify and address.
Austin Health currently reports daily on the reasons sessions start late and has governance processes in place to provide feedback to individuals who consistently arrive late.
Figure 2I
Reasons for delays in morning elective sessions on business days, 1 July 2014 to 31 December 2016
Note: Reasons for delays outside the control of health services have been omitted from this figure.
Note: Late starts have been measured against morning elective sessions only, as these are least likely to be affected by emergency surgery or earlier sessions overrunning.
Source: VAGO.
Turnaround times
Turnaround time is the time taken for staff to clean and prepare the theatre for the next surgery. Victoria does not have a benchmark for assessing turnaround time performance. Queensland Health recommends a turnaround time of 15 minutes. Victoria's average turnaround time between surgeries is 17−21 minutes, depending on the measure used. Turnaround time varies between health services, as shown in Figure 2J.
Figure 2J
Turnaround time by health service, 1 July 2014 to 31 December 2016
Note: Not all health services provided data for 'anaesthetic stop', which is a more accurate measure of turnaround time because it closer to when a patient leaves the operating theatre and staff can begin to prepare it for the next patient.
Note: Health services' performance can be interpreted differently depending upon the points in the procedure used to measure turnaround time and infrastructure. For example, Alfred Health, which does not have anaesthetic bays on all theatres, measures turnaround time from when the patient leaves theatre until the next patient enters. Using this definition leads to a different performance result—internally, Alfred Health reports a turnaround time of 15.6 minutes.
Source: VAGO.
Turnaround time almost halves as the number of elective surgeries performed in a session rises, as shown in Figure 2K. More scheduled surgeries in a session typically indicates that less complex, routine operations are being performed.
Figure 2K
Turnaround time in elective surgeries on business days, 1 July 2014 to 31 December 2016
Source: VAGO.
Session underruns
Across Victoria, 55.3 per cent of elective surgery theatre sessions finished before their scheduled time—known as an 'underrun'—at an average of 31.8 minutes.
Although a degree of underrun is inevitable, Figure 2L shows that 11 per cent of sessions finished more than 90 minutes early, which is enough time to perform many types of surgery.
Figure 2L
Session underrun measured by surgery stop time, 1 July 2014 to 31 December 2016
|
Underrun threshold |
Tertiary health service |
Major health service |
Specialist health service |
Regional health service |
Subregional health service |
State average |
|---|---|---|---|---|---|---|
|
More than 30 minutes |
34% |
39% |
31% |
30% |
21% |
34% |
|
More than 60 minutes |
22% |
21% |
16% |
16% |
17% |
21% |
|
More than 90 minutes |
13% |
10% |
8% |
9% |
9% |
11% |
Note: The totals are not cumulative—they display the percentage of sessions that underran against each threshold.
Source: VAGO.
Figure 2M shows performance by peer group.
Figure 2M
Elective session underrun, by peer group, 1 July 2014 to 31 December 2016
Source: VAGO.
The frequency and number of underruns vary between health services, as shown in Figure 2N.
Figure 2N
Elective session underrun by health service, 1 July 2014 to 31 December 2016
Note: We were unable to calculate an underrun average for SVHM due to issues matching data with data collected from other health services.
Note: Data reports sessions as finishing at the time of the 'surgery stop' timestamp. This will lower the apparent performance of health services because the patient does remain in theatre after this time while the anaesthetist concludes his or her work.
Source: VAGO.
Session overruns
In Victoria, 16.3 per cent of elective sessions overran their scheduled finishing time by an average of 11.6 minutes. Figure 2O shows the overrun by average minutes across peer groups. Health services aim to finish sessions on time, although surgery may take longer than anticipated or there may be more demand for emergency surgery than forecast. In this scenario, operating suite managers have to choose between either running late, with an impact on cost and staff, or cancelling patients awaiting elective surgery. The decision to cancel is governed by internal policies, and the rate of cancellation is included in a health service's SOP and monitored by DHHS.
Figure 2O
Elective session overrun by peer group, 1 July 2014 to 31 December 2016
Source: VAGO.
Overruns vary significantly between health services, as shown in Figure 2P.
Figure 2P
Elective session overrun by health service, 1 July 2014 to 31 December 2016
Note: Overrun results are measured to 'surgery stop' for the last operation performed in the elective session, whether it was an elective or emergency surgery.
Source: VAGO.
Impact on postponements
Figure 2Q compares hospital-initiated postponements with the percentage of elective sessions that underran and overran at the audited health services. These measures describe how effectively health services book elective surgery lists and the impact emergency surgery has on planned elective surgery.
Health service performance against these measures is strongly correlated—for example, high numbers of underruns correlate with fewer postponements. However, a high underrun rate means that time within a surgical session is not efficiently utilised.
Figure 2Q
Audited health services' hospital-initiated postponements, underruns and overruns, 2015–16
Source: VAGO, based on hospital-initiated postponement data from health services' annual reports, 2015–16.
Barriers to benchmarking utilisation rates
Targets
DHHS does not set utilisation benchmarks in Victoria. Benchmarks for utilisation are not common in Australia or internationally. Where these benchmarks are present, they use different methodologies to measure utilisation. Figure 2R compares the publicly available measures from other jurisdictions.
Figure 2R
Theatre utilisation benchmarks
|
Agency |
Measure |
Methodology |
|---|---|---|
|
New South Wales Agency for Clinic Innovation, 2015 |
Utilisation rate of 80% |
Measures from when the patient enters the theatre until they leave. |
|
Queensland Health Operating Theatre Efficiency Guideline, 2017 |
'Comparative elective theatre utilisation'—the target varies by the number of cases per session |
Measures occupied theatre time against the expected occupation rate given the number of scheduled surgeries. |
|
Queensland Health advice to Queensland Audit Office, 2016 |
Utilisation rate of 85% |
A 'better practice' benchmark. Measures from when patients enter the theatre until they leave. |
|
UK Audit Commission, 2003 |
Performance target of 77% |
An estimated target based on the average performance of the health system. It measures from anaesthetic start to surgery stop and includes the amount of unused capacity due to session cancellation. |
Source: VAGO, based on information from the Queensland Audit Office, Theatre efficiency in Queensland public hospitals; Queensland Health, Operating Theatre Efficiency Guideline; New South Wales Agency for Clinical Innovation, Operating Theatre Efficiency Guidelines; and UK Audit Commission, Operating Theatres: Review of National Findings.
We cannot compare Victoria's performance against these measures because they are all calculated based on different methodologies and points in the surgical procedure.
Variations in the process measures used
Process measures—such as timestamps—are important as they enable health services to monitor operating theatre efficiencies, particularly the utilisation rate. Timestamps capture key points in a patient's surgical journey, such as anaesthesia induction time, known as 'anaesthetic start'.
In 2012, DHHS published A guide to surgical services redesign measures for improvement. This guide recommended assessing surgical services through key performance indicators, as well as demand, capacity and process measures. DHHS recommended the timestamps outlined in Figure 2S.
Figure 2S
DHHS's recommended minimum timestamps
|
Timestamp |
Agreed definition |
|---|---|
|
Anaesthetic start |
Time when the anaesthetist begins preparing the patient for anaesthetic |
|
Position/prep start |
Time when the nursing or surgical team begins positioning or preparing the patient for the procedure |
|
Procedure/surgery start |
Time when the procedure is begun—for example, incision for a surgical procedure |
|
Procedure/surgery stop |
Time when the surgeons/physicians have completed all procedure-related activities on the patient |
|
Anaesthetic stop |
Time when the anaesthetist hands over care of the patient to a post-anaesthesia care team |
|
Patient leaves recovery |
Time when patient leaves recovery |
Source: VAGO, based on DHHS, A guide to surgical services redesign measures for improvement.
In the devolved system, health services have customised timestamps to suit their needs, reflecting their practices, infrastructure and IT systems. Although the timestamp names are broadly similar, the underlying definitions can vary between health services—Figure 2T shows an example of the various definitions health services and DHHS use for a single timestamp.
Figure 2T
Different definitions of 'surgery start time' timestamp across agencies
|
Agency |
Definition of 'surgery start time' timestamp |
|---|---|
|
Alfred Health, Austin Health and Melbourne Health |
When the surgical or nursing team begins positioning or preparing the patient for the procedure |
|
SVHM |
Following team 'time out'(a), and immediately before the first surgical incision (positioning and preparing has already occurred) |
|
DHHS |
Time when the procedure is begun—for example, incision for a surgical procedure |
(a) 'Time out' is a surgical safety checklist created by the World Health Organisation.
Source: VAGO, based on health services' internal documents.
2.3 Unused capacity
Health services close their theatres for many reasons, including:
- theatres being serviced, repaired or upgraded
- inbuilt flexibility to respond to changing demand for surgery
- other capacity constraints in the hospital, such as a lack of available beds
- limited funds to fully staff theatres.
We measured unused capacity between 1 July 2016 and 31 December 2016, because this period most reflects currently available theatres. We excluded theatres that first opened during this period so they did not reduce the overall performance result.
We define a theatre as 'unused' if a health service did not run an elective or emergency surgery session for some portion of a business day.
Health services closed theatres on 9.5 per cent of theatre business days throughout Victoria. The distribution varied significantly between health services, as shown in Figure 2U.
Figure 2U
Percentage of business days where theatres were unused, by health service, 1 July to 31 December 2016
Note: Austin Health's unused capacity is explained by four theatres being under-utilised. Its other theatres display a usage level comparable with those of the other audited health services.
Source: VAGO, based on health services' operating theatre data.
Figure 2V shows that regional, subregional and specialist health services have higher levels of available capacity than metropolitan and tertiary health services. These health services also closed theatres on more business days during the six months we reviewed—16.6 days per theatre compared to 10 days per theatre at major and tertiary health services.
Figure 2V also shows an alignment between theatres and waiting lists—70 per cent of the theatres and 62 per cent of the elective waiting list are at major and tertiary health services. However, the major and tertiary health services have limited unused capacity to deliver additional surgery.
To meet rising demand there are a number of options:
- increase theatre capacity through infrastructure investment
- use existing theatres more efficiently
- increase the amount of patients treated at health services with capacity.
Figure 2V
Available capacity and demand for elective surgery, 1 July 2016 to 31 December 2016
Source: VAGO, based on health service operating theatre data and DHHS data.
Among the audited health services, only Austin Health has some available capacity, as it has four under-utilised theatres, shown in Figure 2W. Austin Health confirmed it does not have enough funding to open these theatres more often.
Figure 2W
Austin Health operating theatres with high unused capacity, 1 July 2016 to 31 December 2016
|
Theatre |
Unused capacity |
|---|---|
|
The Surgical Centre, Theatre 1 |
60% |
|
The Surgical Centre, Theatre 2 |
60% |
|
The Surgical Centre, Theatre 3 |
34% |
|
The Surgical Centre, Theatre 4 |
31% |
Note: The four theatres are at the Heidelberg Repatriation Hospital.
Source: VAGO, based on Austin Health data.
Austin Health could treat more patients in these theatres with more funding. As these theatres are suitable for routine elective surgery, Austin Health would require both enough patients requiring low-acuity treatment on its waiting list and sufficient bed capacity to maximise the use of these theatres. As Austin Health already has good access to surgery, making this capacity available to patients from health services with lower access would lead to a better outcome for Victoria.
There are two key barriers to this occurring:
- unused capacity is not identified at the system level due to a lack of data
- there are barriers to moving patients between health services, as discussed in Section 4.2 of this report.
Health services run fewer sessions during the Christmas period, as staff often take leave and patients delay non-urgent elective surgery. Excluding this period, Figure 2X shows that unused capacity is actually lower than the overall data suggests during most of the year.
Figure 2X
Unused capacity by peer group
Source: VAGO.
2.4 Efficiency of surgery
Length of surgery is not an appropriate efficiency measure, as it may encourage surgeons to rush and potentially compromise safety. However, health services could review the cost-efficiency of their surgeons' performance to identify practices that may improve efficiency.
Figure 2Y shows that surgeons who perform operations more frequently tend to perform surgery faster. This enables more operations to be performed within a surgical session.
Appendix C provides other examples of the relationship between frequency and operation length. Graduate surgeons—known as registrars—take longer to perform an operation, as discussed in Part 3 of this report.
Figure 2Y
Hip replacements performed by consultants at one the health services in the ESIS, 1 July 2014 to 31 December 2016
Source: VAGO.
2.5 Cost per hour
The average direct cost of a 'productive hour' of theatre time in Victoria is $2 004. The lowest cost health service ran at $1 647 per hour and the highest cost at $2 468.
The cost per hour includes costs directly recorded by health services as occurring in theatres—salary costs for surgeons, anaesthetists, nurses and technicians, and sterilising services. It does not include the costs of consumables, pharmaceuticals or prostheses, as these vary by case. Excluding them enables us to better compare health services.
A productive hour is time spent performing all surgery, including emergency sessions. We calculated the state's overall productivity rate at 70 per cent of total surgical session time within business hours.
Figure 2Z shows the cost per hour for the health services that provided us with usable data. A challenge in comparing data is the variation in methods health services use to record their financial information, despite DHHS mandating a chart of accounts, as discussed in Appendix D.
Figure 2Z
Cost per hour of surgery
|
Health service |
Total in-surgery hours in business hours |
Productivity rate |
Cost per hour |
||
|---|---|---|---|---|---|
|
At current productivity rate |
At 80 per cent productivity rate |
At 100 per cent productivity rate |
|||
|
W |
6 026 |
79% |
$2 468 |
$2 431 |
$1 945 |
|
T |
39 954 |
76% |
$2 357 |
$2 243 |
$1 795 |
|
X |
51 492 |
72% |
$2 178 |
$1 963 |
$1 571 |
|
I |
15 073 |
81% |
$2 161 |
$2 184 |
$1 747 |
|
V |
14 673 |
66% |
$2 158 |
$1 784 |
$1 427 |
|
N |
34 535 |
71% |
$2 064 |
$1 827 |
$1 461 |
|
A |
19 568 |
87% |
$2 054 |
$2 234 |
$1 787 |
|
K |
14 340 |
59% |
$2 039 |
$1 514 |
$1 211 |
|
D |
18 559 |
60% |
$2 036 |
$1 529 |
$1 223 |
|
Statewide |
679 678 |
70% |
$2 004 |
$1 796 |
$1 437 |
|
Q |
10 731 |
73% |
$1 994 |
$1 807 |
$1 446 |
|
F |
17 513 |
80% |
$1 975 |
$1 983 |
$1 587 |
|
Alfred Health |
57 254 |
72% |
$1 959 |
$1 752 |
$1 401 |
|
L |
105 723 |
71% |
$1 889 |
$1 682 |
$1 346 |
|
E |
52 690 |
69% |
$1 877 |
$1 622 |
$1 297 |
|
G |
63 499 |
73% |
$1 857 |
$1 694 |
$1 355 |
|
SVHM |
40 420 |
66% |
$1 712 |
$1 412 |
$1 130 |
|
Melbourne Health |
52 872 |
77% |
$1 655 |
$1 593 |
$1 275 |
|
Austin Health |
64 756 |
71% |
$1 647 |
$1 457 |
$1 166 |
Note: We excluded five health services as we could not reconcile their financial or theatre data with that provided by other health services to enable an accurate comparison.
Source: VAGO.
Any increase in productivity lowers the average cost per hour—for example, raising the state's average productivity rate to 80 per cent would enable 10 per cent more surgery to be delivered within the same cost base, thereby reducing the average cost per hour by $208.
Comparing the cost at current productivity rates to an 80 per cent benchmark shows there is considerable opportunity for most health services to lower their cost per hour.
The difference in cost per hour of surgery time is driven by:
- underlying costs, such as salary rates
- the amount of out-of-hours work conducted at higher cost
- the productivity rate of theatre sessions.
Health services would reduce their cost per hour by improving their performance against any of these three factors. Productivity rate is the factor that health services are most likely to be able to influence.
3 Management practices
Efficient and effective management of resources requires clear objectives, evidence-based resourcing models, relevant and reliable data to evaluate performance, and sound governance structures to control resource allocation.
In this part of the report, we assess how health services' management practices affect the efficient use of their operating theatre resources.
3.1 Conclusion
Driving and sustaining improved operating theatre efficiency is challenging and needs to be underpinned by a comprehensive suite of reliable, accepted performance measures that are widely shared and actively monitored.
More attention needs to be given to understanding and addressing systemic issues that adversely affect efficiency. Health services do not have a strong understanding of the impact of training of registrars on their theatre efficiency levels or cost base. There are opportunities for health services to improve efficiencies through strategies such as greater specialisation within a surgical unit and prioritising their use of procedure rooms for short, clinically simple cases.
A broader systemic issue for DHHS as system manager is the impact of patient choice on capacity-constrained hospitals.
3.2 Management approaches and practice
We examined how four health services—Alfred Health, Austin Health, Melbourne Health and SVHM—manage their operating theatres at both the executive and operational levels to achieve efficient outcomes. We also consulted with other health services outside the audited group to identify a range of management structures across the sector.
Allocating theatre resources
Health services allocate theatre resources between emergency and elective surgery and for different surgical specialities. They adjust the allocation to meet the changing demand for elective surgery, waiting lists and emergency forecasting. Health services allocate resources over varying time frames, and management groups meet daily, weekly and monthly to adjust allocations as required.
Health services manage the allocation of theatre resources through:
- operating suite floor managers controlling on-the-day theatre allocation
- executive-level management forums evaluating health service performance and forecasting resource allocation.
DHHS issues policies that influence some aspects of how health services allocate resources. For example, the Elective Surgery Access Policy 2015 directs health services to treat patients in turn. Certain circumstances may prevent patients' being scheduled for surgery according to waiting time:
- when a patient's condition has deteriorated
- when the health service has previously postponed the patient's surgery
- a patient being unavailable for surgery
- availability of resources (for example, theatre time, staff, equipment and hospital capacity)
- when there are sound clinical reasons
- teaching and training needs.
When scheduling patients for surgery, health services are required to negotiate with the patient to agree on a mutually acceptable admission date. The policy also requires health services to have local policies that comply with its directions.
Where DHHS does not establish formal policy requirements, the audited health services typically lack comprehensive, finalised policies that govern resource allocation. For example, there is limited guidance for decision-makers on allocating theatres between emergency and elective surgery and between types of elective surgery. Instead, the health services rely on experienced professionals using their best judgement and available data to allocate resources.
The lack of policies affects the transparency of decision-making and the evaluation of resource allocation decisions. It also diminishes the organisational sustainability of the health service if key personnel leave.
Monitoring efficient theatre performance
Figure 3A lists measures that the four audited health services use to assess the efficiency of their operating theatres. However, as health services have developed their measures independently, the definitions and assumptions underlying the measures are not necessarily comparable and, as a result, some health services have better information than others to drive decision-making.
Figure 3A
Comparison of efficiency metrics used at the audited health services
|
Metric |
Melbourne Health |
SVHM |
Austin Health |
Alfred Health |
|---|---|---|---|---|
|
Late start analysis |
✔ |
✔ |
✔ |
✔ |
|
Morning session overrun |
✔ |
✔ |
||
|
Utilisation rate |
✔ |
✔ |
✔ |
✔ |
|
Percentage of surgery completed within session |
✔ |
✔ |
||
|
Cases with overrun greater than 30 minutes |
✔ |
|||
|
Total elective cases |
✔ |
✔ |
✔ |
|
|
Total emergency cases |
✔ |
✔ |
✔ |
|
|
Total scheduled surgical hours |
✔ |
✔ |
||
|
Total overrun hours analysis |
✔ |
✔ |
✔ |
|
|
Surgical utilisation rate |
✔ |
✔ |
✔ |
✔ |
|
Productive/contact time |
✔ |
✔ |
||
|
Turnover time |
✔ |
✔ |
Note: Austin Health uses a measure called 'contact hour' which has an underlying definition similar to 'utilisation rate'.
Source: VAGO, based on audited health services' reports.
Generally, reporting at the audited health services enables management to identify inefficient practices. These internal reports focus on lost theatre time, such as late starts and underruns. These are valuable measures, as they target waste, do not affect patient safety and are within the health services' control.
Executives advised that they regularly provide feedback to surgical units that demonstrate ongoing performance issues, such as starting late. However, continued underperformance indicates that driving and sustaining improved efficiency is challenging, and health services report that projects to improve efficiency take significant management effort and years to implement.
The health services advised that key barriers include clinicians rejecting data as inaccurate and managers not maintaining enough focus on issues to sustain performance improvements.
Alfred Health
Alfred Health's performance reports provide comprehensive information to theatre teams and managers and are an example of better practice. The reports convey a clear visualisation of changing waiting list numbers, as shown in Figure 3B. Alfred Health's reports also provide multiple measures for efficiency—such as utilisation and overrun hours—as demonstrated in Figure 3C. This clear and concise format enables managers to identify trends over time and inefficiencies.
Staff use these reports in multiple management forums, including their monthly Theatre Reference Group, which focuses on managing the health service's resources. The group used the reports to identify a surgical unit that started 75 per cent of its sessions late. As a result, the health service identified emergency surgery and earlier sessions overrunning as the drivers of this inefficiency, which Alfred Health could address through process changes.
Data-driven reporting has enabled Alfred Health to identify inefficiency and has led to management intervening to improve performance.
Figure 3B
Alfred Health's performance report
Source: Alfred Health.
Figure 3C
Alfred Health's visual representation of its waiting lists
Source: Alfred Health.
Austin Health
Austin Health uses a range of reporting to monitor its performance efficiency. This includes daily reporting that captures reasons why sessions started late, consolidated reports used in performance meetings and a live dashboard that tracks patients waiting for and progressing through surgery, as shown in Figure 3D. The dashboard enables theatre managers to understand surgical demand in allocating theatre resources on the day and supports efficiencies, as demonstrated by Austin Health's lower overrun and hospital-initiated postponement rates.
Figure 3D
Austin Health's live dashboard which tracks patients waiting for and receiving surgery
Source: Austin Health.
Data-driven reporting is well established at Austin Health and enables staff to track, identify and address performance issues.
In 2013, Austin Health identified that late starts were significantly disrupting its theatre utilisation rate. This prompted the 'start on time' initiative, which ran from 2013 to 2015. Staff identified vague definitions of key reporting terms, poor inpatient processing, and unreliable data entry as barriers to efficiency.
In response, management formally outlined its 'start time' measure and altered the nurses' rosters in the foyer to ensure the timely transfer of patients. Management also increased staff education about capturing data—an issue that remains particularly important, as tracking the reasons for delays requires complete, consistent and accurate data. Floor coordinators also troubleshoot barriers to start time performance on a daily basis and broadcast a reminder on the operating suite's announcement system.
Although the project formally concluded in 2015, Austin Health has sustained these changes and regularly audits its on-time start rate. This shows the importance of continued managerial effort in driving efficiency.
Melbourne Health
Melbourne Health has improved its systems for reporting performance data, including developing new tools for internal performance reporting over the past three years. By developing better data, Melbourne Health has been able to improve efficiency.
To increase its 'on-time start rate', Melbourne Health used data to identify that 58 per cent of inpatients arrived late to the anaesthetic bay from the wards. This was primarily due to poor communication and staff shortages. In mid-2016, Melbourne Health improved its ward notification system, changed its rostering arrangements, organised additional meetings, and emphasised the importance of accurate data entry. This increased its on-time start rate, as shown in Figure 3E.
Figure 3E
Melbourne Health—improvement in patients arriving on time from hospital wards
Source: Melbourne Health.
St Vincent's Hospital Melbourne
SVHM has an ongoing and wide-ranging project that began in 2014 to improve its operating theatre performance by evaluating its data integrity, performance measures and system reporting. SVHM redeveloped its data collection and quality assurance policies, redefined performance measures and increased staff training as part of the project.
In 2017, SVHM created and is testing data visualisation tools to monitor and evaluate performance, as described in Figure 3F. The time and effort required to implement this change demonstrates the barriers to improvement in health services, although SVHM's current framework should enable it to evaluate and drive efficient performance in the future.
Figure 3F
Case study: Testing business intelligence tools at SVHM
|
SVHM is refining a business intelligence tool to create reports and a smart phone application to provide live performance data to managers. Reporting includes measures such as theatre utilisation rate and the number of surgeries performed. As part of the project, the hospital formalised business rules and definitions for its data. Key steps in the process included:
SVHM staff engaged in extensive consultation to complete each step of the process. Using the business intelligence tool, SVHM quantified utilisation rates across specialities. As a pilot, the project team provided the head of the lowest‑performing surgical unit with the utilisation results for the team—59 per cent—and saw performance improve to 73 per cent and 76 per cent in the following months. Ongoing monitoring and system change enabled SVHM to sustain its positive performance. |
Source: VAGO.
The efficiency initiatives at SVHM show that good data improves performance, and that continuous focus is required to sustain change.
3.3 Influences on productive efficiency
Health services and experts have identified a range of factors that influence operating theatres' productive efficiency:
- the need to train registrar surgeons
- theatre capacity constraints
- patients receiving treatment outside of their local hospitals
- the specialisation of surgeons
- procedure room usage.
The audited health services are aware of these issues, but have not quantified their impact. For this audit, we used data from the 23 ESIS health services to measure the influence of these factors on efficiency.
Training registrar surgeons
Training registrar surgeons is an important aspect of the public healthcare system. However, it limits the productive efficiency of operating theatres.
Using data to quantify the impact of registrars' involvement—such as increased operating time—enables health services to evaluate the cost of teaching. It also assists in the efficient planning of surgical sessions and can help health services reduce the prevalence of overruns.
We found that operations led by a registrar are, on average, 15 minutes longer than operations led by a fully qualified surgeon, known as a consultant. Figure 3G shows the impact of surgery length across peer groups.
In 2015–16, registrars led 74 000 operations. At an average of 15 minutes more time per surgery, the training added an additional 19 050 hours of theatre time to these surgeries. With theatre costing an average of $2 004 per hour for staff, this training cost about $37 million. Consultant-led operations in which they teach registrars will also incur an additional time burden that is not identifiable in the existing data.
Health services have not demonstrated a strong understanding of the impact of training on their theatre efficiency levels or cost base.
Figure 3G
Comparison of the length of operations for consultants and registrars in 2015–16
Source: VAGO.
Capacity constraints
We have identified a relationship between physical operating theatre capacity and efficiency—as the number of unused theatre days decreases, theatre inefficiencies rise.
Melbourne Health runs its theatres at 97 per cent capacity, which is the highest of the audited health services. Melbourne Health has advised that this is necessary to meet its high surgical demand.
Figure 3H compares capacity and efficiency measures at Melbourne Health with other tertiary hospitals, health services with less than 10 per cent unused capacity, and the state's average.
Figure 3H
Comparison of operating theatre efficiency measures
Note: Unfunded capacity data from 1 July 2016 to 31 December 2016; hospital-initiated postponement data for 2015≠–16; utilisation, overrun and underrun data for 1 July 2014 to 31 December 2016.
Source: VAGO.
The data shows a clear correlation between decreased capacity and rising inefficiencies. This indicates that health services require some unused capacity to create flexibility and stabilise performance. In particular:
- As Melbourne Health runs at 97 per cent capacity, it is difficult for management to accommodate increased surgical demand and cover periods of theatre maintenance.
- Melbourne Health manages its high emergency demand by adding emergency cases to the end of its elective sessions, which creates overruns. Melbourne Health overruns 41 per cent of its elective sessions by 44minutes, compared to the state's average of 16 per cent at 12 minutes.
- By adding emergency cases to the end of its elective sessions, Melbourne Health rarely underruns and its utilisation rate is higher than its peers and the state average. It underruns 27 per cent of its sessions by 13minutes against the state's average of 55 per cent at 32 minutes.
- Melbourne Health's hospital-initiated postponements—the deferral of an elective patient's scheduled admission date—was 9.8 per cent in 2015–16 against the state target of 8 per cent and state average of 5 per cent. Melbourne Health's performance in 2016–17 fluctuated across the course of the year, from a high of 9.4 per cent in the first quarter to 6.3 per cent in the final quarter.
Patients not being treated at their local health service
Patients, in consultation with their general practitioner (GP), decide where they will be referred for their elective surgery.
Figure 3I shows that 40 per cent of patients treated at major and tertiary health services—located within greater Melbourne—lived more than 20 kilometres away from where they had their surgery.
Patients at regional and subregional health services travel further for surgery, which is a result of the greater distance between health services and the larger areas that regional services cover.
Figure 3I
Distance elective surgery patients travel (kilometres) by peer group, 1 July 2014 to 30 June 2016
Source: VAGO, based on DHHS VAED data.
By knowing where their patients come from, health services can better understand growth and engage with health networks to influence outcomes.
Austin Health receives 80 per cent of its patients from within a 20-kilometre radius, giving it the opportunity to engage with local GPs to drive behaviour such as ensuring that referrals contain complete information and that patients have undertaken required testing before attending a specialist clinic appointment.
At the health service level, the distance that patients travel varies significantly, and is influenced by patient choice, localised population growth, type of service provided and the distance between hospitals, as seen in Figure 3J.
Figure 3J
Distance elective surgery patients travel (kilometres) by health service, 1 July 2014 to 30 June 2016
Source: VAGO, based on DHHS VAED data.
Health services do not have geographical 'catchments' or control over whether a GP refers a patient to their clinics for assessment. Health services have advised that patients may choose a health service based on factors such as professional relationships between clinicians, surgeons working at different locations, ability to provide treatment in a timely manner, health service reputation and patient preference, as well as proximity.
The cost of providing treatment is broadly similar across health services, so as long as a health service has capacity, the impact of patients choosing not to be treated locally is minimal.
However, an inefficiency arises if a tertiary hospital treats a 'routine' patient and consequently cannot treat a complex case within clinically recommended time frames.
Melbourne Health has limited available capacity and uses its theatres for both emergency and elective surgery. Figure 3K shows that Melbourne Health treated 1 670 elective orthopaedic patients from Melbourne's inner west, north-west and the Ballarat region, between 1 July 2014 and 31 December 2016. Ballarat Health, Barwon Health, Western Health and Northern Health are non-tertiary health services closer to the patients' homes, which could have treated these elective orthopaedic patients.
From the available data, we could not identify if these patients had additional clinical needs requiring treatment in a tertiary hospital or were routine cases.
Figure 3K
Elective orthopaedic surgery delivered by Melbourne Health for patients from Melbourne's north west, 1 July 2014 to 30 June 2016
Source: VAGO.
Specialisation of surgeons
Victorian health services provide surgery according to their capability, capacity, profile and demand. As a result, surgeons may perform some operations infrequently, resulting in increased surgical times. Health services may improve their productive efficiency by encouraging specialisation within a surgical unit.
We compared the length of time it takes surgeons to complete six common operations against the number of operations performed. The operations were:
- appendectomy
- fractured neck of femur
- hip replacement
- knee replacement
- cataract surgery
- coronary artery bypass.
Figure 3L shows the difference in average operation time between the 10 highest-volume surgeons and those who performed the operation not more than 10 times.
Figure 3L
Average length of surgery (minutes), by type of operation, comparing high- and low-volume surgeons, 1 July 2014 and 31 December 2016
|
Surgeon cohort |
Appendectomy |
Fractured neck of femur |
Hip replacement |
Knee replacement |
Cataract surgery |
Coronary artery bypass |
|---|---|---|---|---|---|---|
|
Top 10 by volume |
47.7 |
59.8 |
99.0 |
92.3 |
20.6 |
223.4 |
|
≤ 10 operations |
53.1 |
62.7 |
119.5 |
118.6 |
25.9 |
220.6 |
|
Difference |
11% |
5% |
21% |
28% |
26% |
–1% |
Source: VAGO.
In three types of operations, the surgeons' average surgical time fell by over 20 per cent as the number of operations increased.
This is beneficial, as in cataract surgery, where saving five minutes per operation may enable health services to book additional cases. Conserving over 20 minutes per hip and knee replacement may allow health services to schedule short, simple operations at the end of existing surgical sessions. Both scenarios allow health services to maximise the amount of surgery generated from their available theatre time.
In two types of surgery, the time saved is marginal, and we observed a minor increase in time for coronary artery bypass operations.
Reducing the number of surgeons performing low-volume activity also addresses recommendations from the 2016 review of patient safety, Targeting Zero: Supporting the Victorian hospital system to eliminate avoidable harm and strengthen quality of care, which identified a relationship between surgeons performing an operation irregularly and adverse safety outcomes.
Procedure room usage
Many health services have procedure rooms in their hospitals. These sterile spaces are less equipped than operating theatres and accommodate simple procedures, such as cystoscopies and endoscopies. Surgeons sometimes perform these procedures in operating theatres, and a patient's clinical needs may make this necessary. Efficiency may increase if health services prioritise procedure rooms for short, clinically simple cases—this creates space in operating theatres for more complex surgery. Between 1 July 2014 and 31 December 2016, over 15 000 procedures that required less than 15 minutes each for anaesthesia and operative time occurred in fully equipped operating theatres. Figure 3M shows the most common procedures in this group—these types of operations are often booked in procedure rooms and are of limited complexity.
Figure 3M
Short procedures occurring in operating theatres, 1 July 2014 to 31 December 2016
Source: VAGO, based on health services' data.
Health services across all peer groups deliver short procedures in fully equipped operating theatres, as shown in Figure 3N.
Figure 3N
Short elective procedures in operating theatres, by peer group, 1 July 2014–31 December 2016
Source: VAGO.
From the data, we cannot verify whether these procedures required an operating theatre due to increased complexity of the individual patient. Health services should re-evaluate their allocation policies to ensure that procedure rooms and operating theatres are appropriately booked.
4 System design
Under Victoria's devolved governance model, DHHS does not control the operating models health services choose or how they meet their targets.
In this part of the report, we examine how DHHS and health services design systems to allocate theatre resources and drive the productivity of Victoria's public operating theatres.
4.1 Conclusion
The current health system design does not support the efficient use of operating theatres. Victoria is not meeting its access targets for semi-urgent and non‑urgent elective surgery, because resource allocation focuses instead on achieving waiting list targets. The funding model and the targets set for health services by DHHS do not provide incentives for health services to be as productively efficient as possible.
The lack of centralised control of data quality, definitions and performance measures inhibits benchmarking and sharing of better practice across the sector. DHHS needs to improve operating theatre efficiency by collecting information that would enable health services to identify inefficiencies and by supporting the transfer of good ideas and practices between health services.
DHHS's current information on theatre usage and demand for surgery is incomplete, which inhibits its ability to plan for capital investment and budget allocation. DHHS does not measure access to emergency surgery, so it is not possible to assess whether enough theatre resources are being allocated to treat emergency patients within required time frames.
4.2 Health service organisation
Victoria's health services use a range of models to manage their theatre resources to deliver emergency and elective surgery across different surgical specialities. Elective and emergency surgery compete for the same finite theatre resources, although only access to elective surgery is measured directly. As a result, it is not possible to assess whether health services are allocating resources efficiently between the two surgery streams. Health services therefore risk misallocating theatre resources, resulting in patients waiting beyond clinically recommended time frames for surgery.
Theatre resource allocation
DHHS produced Good practice in management of emergency surgery: A literature review in 2010, which described four models used by Victorian health services to allocate theatre resources between elective and emergency surgery:
- using dedicated emergency surgery lists or theatres
- reserving capacity in elective surgery lists to allow flexibility in the schedule for emergency cases
- balancing business-hours and out-of-hours work by using twilight lists or out‑of-hours operating theatre sessions for emergency surgery
- clearly separating elective and emergency surgery resources to reduce the impact that emergency cases have on elective sessions, and vice versa.
The review did not evaluate the outcomes of each model or make recommendations to health services on which model they should use. All four models are in use in Victoria, with most health services using components of several models in a hybrid approach.
Health services identified infrastructure, case load and historical precedent as key drivers in their choice of resource allocation model. Rather than finding consistency between health services with similar circumstances, we observed that health services with similar case loads or infrastructure adopt significantly different models. This indicates that historical precedent can have a strong influence—health services maintaining a 'this is how we do it' ethos—which may not deliver the best allocation of resources.
Figure 4A shows how the audited health services allocate their theatre resources alongside their overrun results. The table shows a clear correlation between separating the two surgical streams and overrun results for both elective and emergency surgery.
A comprehensive analysis of the relationship between the models, case loads, infrastructure and outcomes would improve the sector's understanding of the benefits of each model in different circumstances.
Figure 4A
Overruns in elective and emergency surgery at the audited health services
|
Health service |
Model |
Hospital |
Main use |
Overrun (percentage of sessions) |
Average overrun (minutes) |
|---|---|---|---|---|---|
|
Alfred Health |
|
Alfred Main |
Emergency and complex elective surgery |
20.5% |
16.0 |
|
Alfred Centre |
Routine elective surgery |
8.9% |
22.7 |
||
|
Sandringham Hospital |
Emergency and routine elective surgery |
12.6% |
4.6 |
||
|
Austin Health |
|
Austin Hospital |
Emergency and complex elective surgery |
17.5% |
12.9 |
|
Heidelberg Repatriation Hospital |
Routine elective surgery |
5.2% |
1.4 |
||
|
Melbourne Health |
|
Royal Melbourne Hospital |
Emergency and all elective surgery |
37.5% |
40.5 |
|
SVHM |
|
St Vincent's Hospital |
Emergency and all elective surgery |
24.3% |
29.6 |
Source: VAGO.
Health services frequently review their theatre resources allocation, such as the number of sessions assigned to each speciality, compared to demand. However, we found limited evidence of health services evaluating how their chosen model affects efficiency.
The 2011 paper Streamlining elective surgery care in a public hospital: The Alfred experience shows how this evaluation could occur by quantifying how physically separating elective and emergency surgery improved efficiency at Alfred Health.
Elective surgery access
Access to elective surgery varies between health services and across different types of elective surgery.
Figure 4B shows the percentage of patients waiting longer than their recommended time in category 2 (treat within 90 days) and category 3 (treat within 365 days) at the health services that submit data to ESIS.
Figure 4B
Percentage of category 2 and 3 patients treated outside clinically recommended time frames, 1 April to 3 June 2017
Source: VAGO, based on DHHS data.
A comparison of Alfred Health's and Melbourne Health's access outcomes shows that patients at Melbourne Health have a much higher likelihood of waiting longer than the clinically recommended time frames for their surgery. The distribution of theatre resources is important in this example—during 2105−16, Alfred Health's elective surgery waiting list grew by 28 per cent but the health service managed it with comparably higher funding and with access to 19 theatres compared to Melbourne Health's 12.
Access to different surgery types also varies across health services. Allocative efficiency would ensure that patients waiting for the same type of surgery received it in a similar time frame, regardless of which health service performed the surgery.
Figure 4C shows the difference across several major surgical types at the audited health services. It shows that the median wait time for an ear, nose and throat (ENT) operation at Austin Health was nearly twice as long as at SVHM. However, the situation is reversed for plastic surgery, with the median wait time at SVHM less than half that of Austin Health.
Figure 4C
Median wait for surgery by speciality, April 2016 to March 2017
Note: DHHS reports quarterly on median waiting times. This graph reports the median result of those published figures over the year to 31 March 2017.
Source: VAGO, based on DHHS data.
Key drivers of this variation are a mismatch between the demand for and supply of a surgery type at a health service, the way a health service allocates resources between surgery types, and the system's inability to distribute patients because its design incorporates patient choice and devolved governance.
Victoria runs a devolved health system in which health services are responsible for managing their own resources and waiting list. Victorian GPs can refer patients to any health service, regardless of capacity and wait times, although GPs should consider this information. The health system could encourage allocative efficiency by improving dissemination of waiting time information and by moving patients between health service waiting lists.
Across the ESIS health services, between 3 000 and 4 000 patients a year receive elective surgery at a different hospital to the one at which they were waiting. Health services or DHHS may facilitate this reassignment of patients.
This represents approximately two per cent of the elective surgery performed by the ESIS health services. DHHS's Elective Surgery Access Policy is designed to support the transfer between health services of patients who have been on the waiting list for a long time.
Health services have advised us that there are barriers to moving patients, such as:
- patients being unwilling to transfer due to geographic inconvenience or clinician preference
- local clinicians needing to maintain continuity of care up to surgery and beyond
- difficulties in negotiating clinical responsibility, funding and costs between health services
- performance reporting mechanisms that attribute the patients' waiting times to the treating health service, rather than the one that managed the patient before surgery.
None of these barriers are insurmountable, but health services need to expend additional resources to facilitate a transfer.
Emergency surgery access
Victoria does not have access measures for emergency surgery. Establishing access measures would direct health services' focus to balancing resources between elective and emergency patients. Health services could use access measures to evaluate whether patients receive emergency surgery in time to avoid worse clinical outcomes.
In 2012, DHHS released A framework for emergency surgery in Victorian public health services, which explains the challenges for health services:
'In many health services, both elective and emergency caseloads share the same operating theatres, surgeons and teams Ö A balanced approach in the provision of emergency and elective surgery can facilitate improved access, and result in improved patient outcomes, decreased cancellations of elective and emergency surgery, shorter waiting times and reduced rates of emergency surgery being undertaken after hours.'
This document recommended a six-tier category system linking clinical urgency to waiting times. The system is designed to ensure that clinical urgency is the key driver of decisions in allocating theatre resources.
DHHS is currently working with the Victorian Surgical Services Advisory Committee to gain agreement on appropriate access targets based on the 2012 framework. Underpinning this work is new evidence concerning access times for particular emergency surgery types—this evidence became available when DHHS began collecting surgery start times for emergency surgery cases. DHHS has found that procedure-focused access measures could provide incentives for health services to focus on improving procedures.
Health services have found that emergency access measures would help them balance resource allocation. They report that some clinicians seek additional emergency surgery theatre time for their speciality, without being able to prove the need.
In 2017, SVHM began to use a set of internal measures of emergency access, as shown in Figure 4D, which enables it to evaluate resource allocation between emergency and elective surgery based on quantifiable need.
Figure 4D
SVHM's emergency priority codes
|
Priority codes |
KPI (to anaesthetic preparation) |
Examples |
|
|---|---|---|---|
|
0 |
Immediate |
Within 30 minutes |
The patient is at immediate risk of loss of life, shocked or moribund, resuscitation not providing positive physiological response Abdominal trauma, burr holes, vascular repairs, compartment syndrome |
|
2 |
Urgent |
Within 120 minutes |
The patient is physiologically stable but the surgical problem may undergo significant deterioration if left untreated Peritonitis, ischaemic bowel, strangulated hernia, severe sepsis |
|
3 |
Urgent |
Within 6 hours |
The patient's condition is stable—no deterioration is expected Localised peritonitis, incarcerated hernia |
|
4 |
Urgent |
Within 12 hours |
The patient's condition is stable—no deterioration is expected Bowel obstruction no ischemia, appendectomy, sick gall bladders, compound fractures, contaminated wounds |
|
5 |
Urgent |
Within 24 hours |
The patient's condition is stable—no deterioration is expected but the patient is not suitable to be discharged Most fractures, most acute gall bladders |
|
8 |
In hours urgent |
Within 72 hours |
The patient is stable, however, due to co‑morbidities/support systems required, surgery needs to be performed in hours |
|
12 |
Not ready for surgery/knowledge of potential surgery |
May be a case being transferred from another hospital, in which the other hospital is flagging that the patient requires surgical access |
|
Source: VAGO, based on information from SVHM.
4.3 Health system governance
DHHS's strategic documents identify efficient use of resources and equity of access as key goals for the health sector. DHHS's governance of the system needs to be based on robust data and performance management frameworks to achieve these objectives.
Data management
DHHS collects multiple datasets to enable it to count, classify and cost activity across the health system. The datasets most relevant to this audit are:
- Victorian Admitted Episodes Dataset (VAED)—provides a comprehensive dataset of the use of health services in Victoria
- Victorian Emergency Minimum Dataset (VEMD)—comprises data on presentations at emergency departments
- Victorian Cost Data Collection (VCDC)—collects data on the cost and mix ofresources used to deliver patient care
- Elective Surgery Information Systems (ESIS)—collects elective surgery waiting list data from participating Victorian public health services
- Victorian Integrated Non-Admitted Health (VINAH)—collects data across a range of services, including specialist clinic information.
DHHS uses these datasets to recalculate the ABF price and weighting to drive efficiency.
DHHS does not collect operating theatre system data from health services. DHHS began to collect surgery start times for emergency surgery from health services in 2016≠–17, although it does not collect the full range of timestamps needed to analyse theatre efficiency, or any timestamps for elective surgery.
The lack of a statewide dataset is the key barrier to measuring theatre efficiency, benchmarking health service performance, and identifying and disseminating better practice.
DHHS's datasets also do not identify if there is unused capacity in the health system because they do not record if a theatre is staffed and available to perform surgery.
Performance management
DHHS has a detailed performance management framework for health services, outlined in the Victorian health services performance framework and Victorian health agency monitoring and intervention. DHHS routinely provides performance information to health services and assesses them against the targets in their SOPs. However, it does not assess theatre efficiency.
Measuring productive efficiency
DHHS's A guide to surgical services redesign measures for improvement recommends minimum timestamps that health services should capture and recommends multiple measures of theatre efficiency, such as utilisation rate, underruns and overruns.
DHHS does not require health services to use these measures or set efficiency targets in their SOPs. Health services are using some of the recommended measures internally, as discussed in Part 3 of this report.
The New South Wales Agency for Clinical Innovation and Queensland Health produced operating theatre efficiency guidelines, in 2014 and 2017 respectively, which contained recommendations similar to those in DHHS's guide.
Queensland Health collects nine theatre timestamps—including 'in anaesthetic time' for anaesthetic start, 'in operating room time' when a patient enters the theatre and 'procedure start time' when the patient is positioned and prepared. Queensland Health provides definitions for each timestamp, which health services incorporate into their IT systems and processes to ensure consistency. Queensland Health and its health services can use this information to measure and benchmark theatre efficiency.
Queensland Health has begun to evaluate health services' theatre efficiency against utilisation measures including overall utilisation rates and late starts, with plans to incorporate this into its reporting regime.
These measures target wasted surgical time and identify how a health service can become more efficient in its theatre usage. Similar measures would be effective in Victorian hospitals too, although Victoria lacks a common dataset and definitions to enable their implementation in the short term.
Supporting productive efficiency
DHHS has supported projects that target theatre efficiency under various programs, including through its Redesigning Hospital Care Program and through Better Care Victoria's current funding mechanisms.
DHHS funded nine health services to participate in the United Kingdom National Health Service's Productive Operating Theatre program. Health services chose projects based on their perceived efficiency risks and measured improvements in hospital-initiated postponements, start on time and utilisation measures. The benefits of support programs can be maximised by communicating successful elements of the projects, and DHHS has published case studies of a range of successful interventions.
DHHS currently funds health services to participate in benchmarking programs run by private providers. This enables health services to compare some aspects of their performance, although the benefits are limited for a number of reasons:
- programs rely on health services providing accurate data
- not all health services participate
- data is anonymised and does not necessarily benchmark factors that drive theatre efficiency, such as turnaround times or underruns.
Benchmarking and sharing better practice
The Victorian health sector does not have the data or systematic processes for identifying better practice and sharing knowledge to improve operating theatre efficiency.
Benchmarking
Health services are able to measure their own performance, but are unable to benchmark their results because they do not have access to their peers' information. Health services are keen to have this information to help them understand how they are performing and to identify strategies they could learn from high performers.
For this audit, we collated theatre data from the 23 ESIS health services from 1 July 2014 to 31 December 2016 and compared performance across peer groups and state averages. Using this data, we created visual dashboards that enabled us to analyse performance at the state, peer group and health service levels across the measures in Part 2 of this report.
We provided the four audited health services with data that compared their performance with those of their peer group and state averages. This led Austin Health and Alfred Health to identify areas they could re-evaluate to improve their efficiency. If this dataset existed for all of Victoria, more health services would be able to identify areas for improvement.
Sharing better practice
DHHS leads forums within the sector that examine health service practices, including the Victorian Surgical Services Advisory Committee and the Elective Surgery Group. These forums enable DHHS and health services to discuss issues relating to health service performance. They have led to projects that could improve theatre efficiency, such as improving the categorisation of elective surgery and developing emergency surgery access measures.
However, health services advised us that the existing forums do not facilitate benchmarking, the identification of better practice or the exchange of ideas between health services, although they do focus on beneficial projects. Health services advised that theatre efficiency would be improved through detailed discussion of what works in managing theatre resources. Health services have stated that knowledge is being informally shared through staff movement, professional relationships and ad hoc forums.
The Victorian Agency for Health Information and Better Care Victoria—now incorporated into Safer Care Victoria—are new agencies that may support the sharing of better practice and establish datasets to evaluate performance in future.
Allocative efficiency
DHHS reports on measures—waiting list numbers and access targets—that drive and evaluate the health system's allocation of resources to elective surgery. Of the two measures, access targets evaluate whether patients receive treatment within clinically recommended time frames and is a better measure of allocative efficiency.
The waiting list target focuses on delivering an amount of surgery, without considering the timeliness or the type of surgery delivered. The emphasis DHHS places on the waiting list target in planning the level of funded activity across the state does not support Victoria to achieve its elective surgery access targets.
DHHS's forecasting of the amount of surgery required to maintain the state's waiting list target is based on robust historical data, resulting in the state balancing additions to and removals from the waiting list. The state finished only 0.63 per cent away from its overall target in 2015–16.
DHHS's analysis includes:
- counting and costing previous activity based on DHHS datasets
- forecasting growth across elective and emergency surgery
- analysing health service performance and necessary growth to maintain delivery levels
- engaging with health services.
The resulting advice quantifies the amount of surgery required to meet anticipated demand across emergency and elective surgery.
However, although the advice describes access levels and a proposed target, it does not quantify how different levels of resource allocation will affect Victoria's performance across its access targets. The state has not achieved its access targets for treating semi-urgent (category 2) and non-urgent (category 3) patients over the four years to 2015–16, as shown in Figure 4E. The state met its category 1 access target of 100 per cent in each of these years.
Figure 4E
Access to elective surgery compared to the state's targets
Source: VAGO, based on DHHS annual reports and Victorian State Budget papers.
Against the access criteria, the health system is not allocatively efficient because it is not meeting its targets and patients are waiting longer than the clinically recommended time frames for surgery.
Productive efficiency
Although Victoria has a devolved system of health service management, DHHS's performance measures and funding model could provide incentives for health services to use their theatre resources efficiently.
While Victoria's operating theatres demonstrate good overall utilisation rates at the state level, there are opportunities to improve the causes of inefficiency, such as late starts and underruns. Health services have identified that improving performance in these areas is possible, although it requires significant management effort to drive change in processes and culture. Further, they have found that the gains can be lost if management focus is not maintained. The persistence of these inefficiencies indicates that the design of the health system does not provide sufficient incentives for health services to address theatre efficiency issues.
DHHS can affect health service practices in two key ways—through the SOPs and through its funding mechanism. How DHHS designs these tools affects the productive efficiency of operating theatres.
SOP targets
To deliver the state's elective surgery waiting list target, DHHS sets access targets and negotiates with each health service to deliver a set amount of elective surgery. While the target for the amount of elective surgery could act as a minimum level of surgery delivered, we found that it is instead acting as a goal that drives resource allocation levels for elective surgery. This level of surgery is calculated based on waiting list targets, not to meet access targets.
Figure 4F shows that health services delivered surgery at or close to their targets in 2015–16.
Figure 4F
Elective surgeries delivered as a percentage of the health services' targets, 2015–16
Source: VAGO, based on health services' SOPs and annual reports 2015–16.
Health services could reduce the cost of performing surgery by becoming more efficient, which would enable them to fund more treatment—both surgery or other treatment—from among their competing demands for service. It is understandable that once a health service meets its elective surgery target it will direct resources to the areas of highest clinical priority, which may or may not be additional elective surgery.
Becoming more efficient in delivering elective surgery is one way that health services could improve performance against their targets using existing resources, although current targets do not explicitly link the delivery of elective surgery to resources consumed.
Targets that require health services to maximise the amount of surgery performed during a session—such as a late start target—would focus health services on minimising wasted surgical time to become more efficient.
Funding
The funding model provides incentives for health services to deliver ABF activities, including surgery, to the amount that will maximise revenue and funding growth—104 per cent of their capped funding. Once health services reach their capped activity level, DHHS does not fund them to deliver additional activity—surgery or other treatment. Health services may therefore not have sufficient budget to open theatres and deliver more surgery, even when they create theatre capacity by becoming more productively efficient.
In 2015–16, only one health service exceeded its final cap—at 104.2 per cent, as shown in Figure 4G. The audited health services told us about their efforts to balance the provision of additional surgery to deliver clinical outcomes with financial constraints due to the capped funding.
Figure 4G
Health service output relative to their funding cap, 2015–16
Source: VAGO, based on health services' annual reports 2015–16.
DHHS may adjust a health service's cap during the year, subject to available budget and competing priorities, although health services cannot rely on this adjustment occurring. In 2015–16, the highest adjustment to a health service's cap was 2.4 per cent, but most adjustments were less than 1 per cent.
DHHS may also alter a health service's cap year to year, based on performance. This means that a health service that delivers above 100 per cent of the cap may receive greater funding in following years. Figure 4H shows that funding growth in 2016–17 did largely follow performance above the cap in 2015–16.
Figure 4H
Changes to health services ABF caps, 2015–16 to 2016–17
Note: The large increases at health services F and P reflect extra funding to staff newly opened theatres.
Source: VAGO, based on health services' annual reports.
Funding adjustments
Extra funding may become available during the year, which DHHS distributes to health services so they can deliver more surgery. DHHS does not link additional funding to efficient performance.
In 2016–17, $162.87 million of federal National Health Reform funding became available to DHHS mid-year. DHHS allocated $35.62 million of this to support health services to manage risks in the delivery of their SOPs. DHHS made an additional $22.93 million available for mid-year review requirements.
DHHS considered a range of demands and risks that it and the health services identified when deciding how to distribute this funding, including:
- health services' cashflow and budget position
- health services' activity levels
- previous funding commitments
- minor capital support requested for critical items
- health services' requests for funding to deliver additional surgery.
Although the priorities for funding are clear, the funding policy provides limited guidance on how DHHS should allocate funds between competing priorities. Eight health services bid unsuccessfully for additional funding to deliver more surgery. If funded, these health services could have maximised the delivery of surgery from their theatre infrastructure and overheads, thereby increasing efficiency.
DHHS may also provide funding tied directly to activity—usually later in the financial year—which focuses on helping health services and the state meet waiting list targets.
In March 2017, DHHS funded health services to treat an extra 2 245 patients during the last quarter of 2016–17 at a cost of $18.1 million. This additional activity enabled the state to meet its end-of-year waiting list target, although, as Figure 4I shows, the number of people waiting for elective surgery fluctuates significantly during the year.
Figure 4I
Patients on the elective surgery waiting list, 2016–17
Source: VAGO, based on DHHS data.
Health services used different methods to deliver additional funded surgery in the final quarter of the year, including out‑of‑hours surgery, outsourcing to private hospitals, and staff working extra shifts within business hours. Health services have identified that funding surgery in this way increases costs—for example, the cost of penalty rates to deliver surgery out of hours. Health services have advised that they could plan for and deliver this activity at lower cost if DHHS provided funding earlier in the financial year.
Figure 4J shows the increase in weekend elective surgery that occurs later in the year to support the additional delivery. Private hospitals treated 645 public patients in 2016–17. We could not quantify the number of additional shifts worked within business hours from available data.
Figure 4J
Weekend elective surgery, 2014–15 and 2015–16
Source: VAGO.
4.4 Health system planning
DHHS is responsible for leading the growth of theatre capacity to meet rising demand for surgery, including capital infrastructure development and funding health service activity.
DHHS can create capacity within existing infrastructure by supporting health services to improve their theatre efficiency and ensuring sufficient funding is available to staff theatres.
There are limitations to DHHS's data and its usage which affect its understanding of theatre capacity and demand for surgery in Victoria.
Understanding operating theatre capacity
DHHS maintains a census of operating theatres in Victoria, which it uses to identify the number of available theatres. However, DHHS does not collect information on how health services are using and staffing their theatres.
The amount of surgery performed in operating theatres, and consequently their capacity to meet demand, is dependent on how efficiently health services manage their theatres. DHHS does not have access to the data required to assess theatre efficiency.
The absence of this data creates two key risks for DHHS:
- Existing theatres are closed—additional recurrent funding for clinical staff could deliver more surgery without further capital investment and would maximise surgical output from the same overhead costs.
- Theatre resources are not being efficiently utilised—where productive efficiency is low, performance improvements would increase capacity without additional infrastructure and would reduce wasted recurrent funding.
By collating operating theatre data, we have identified that there is limited additional physical capacity in tertiary and major health services, which manage the majority of the metropolitan theatre infrastructure. To deliver more surgery, DHHS will need to invest in additional infrastructure or provide incentives for health services to use existing theatres more efficiently. Any increase in surgical output would need to reflect other potential capacity constraints such as available intensive care units and ward beds.
Understanding demand
DHHS uses historical data and growth projections to forecast future demand for emergency and elective surgery. Key determinants include the amount of surgery that health services have previously delivered, the elective surgery waiting list, population growth and system changes such as ongoing work to improve access to specialist clinics.
There are several key risks inherent in the existing system due to gaps in the information available to DHHS:
- There are 37 health services that perform surgery but that do not provide data to the ESIS dataset. As a result, DHHS has limited information about demand for surgery at these health services.
- Patients are added to a health service's waiting list by either attending a public specialist clinic appointment or by a surgeon's private rooms referring them to the health service for surgery. Health services, particularly tertiary health services, may also receive transfers from lower-acuity hospitals that are unable to provide treatment to emergency patients. DHHS expects that health services' recent increased focus on improving access to clinics will raise the number of patients on the waiting list. However, the anticipated size of the increase is unknown, as DHHS has not estimated the increase in clinic appointments or the proportion of patients who will require surgery.
- DHHS uses general population growth and change in health service demand to forecast surgery activity at individual health services. DHHS could strengthen its analysis by using the geographical information available unsaved dataset as part of its planning for funding growth and capital expansion.
Appendix A. Audit Act 1994 section 16—submissions and comments
We have consulted with DHHS, Alfred Health, Austin Health, Melbourne Health and SVHM, and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report, or relevant extracts, to those agencies and asked for their submissions and comments. We also provided a copy of the report to the Department of Premier and Cabinet.
Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
Response provided by the Secretary, DHHS
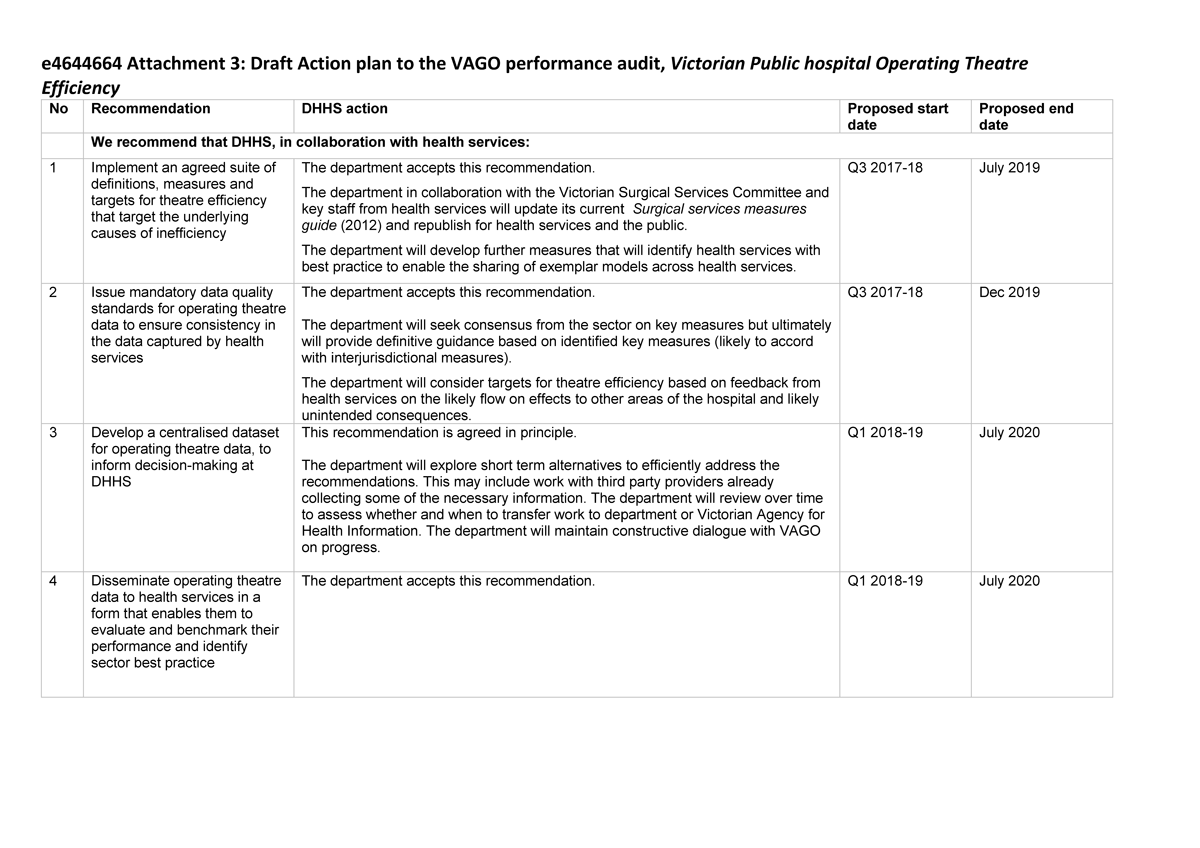
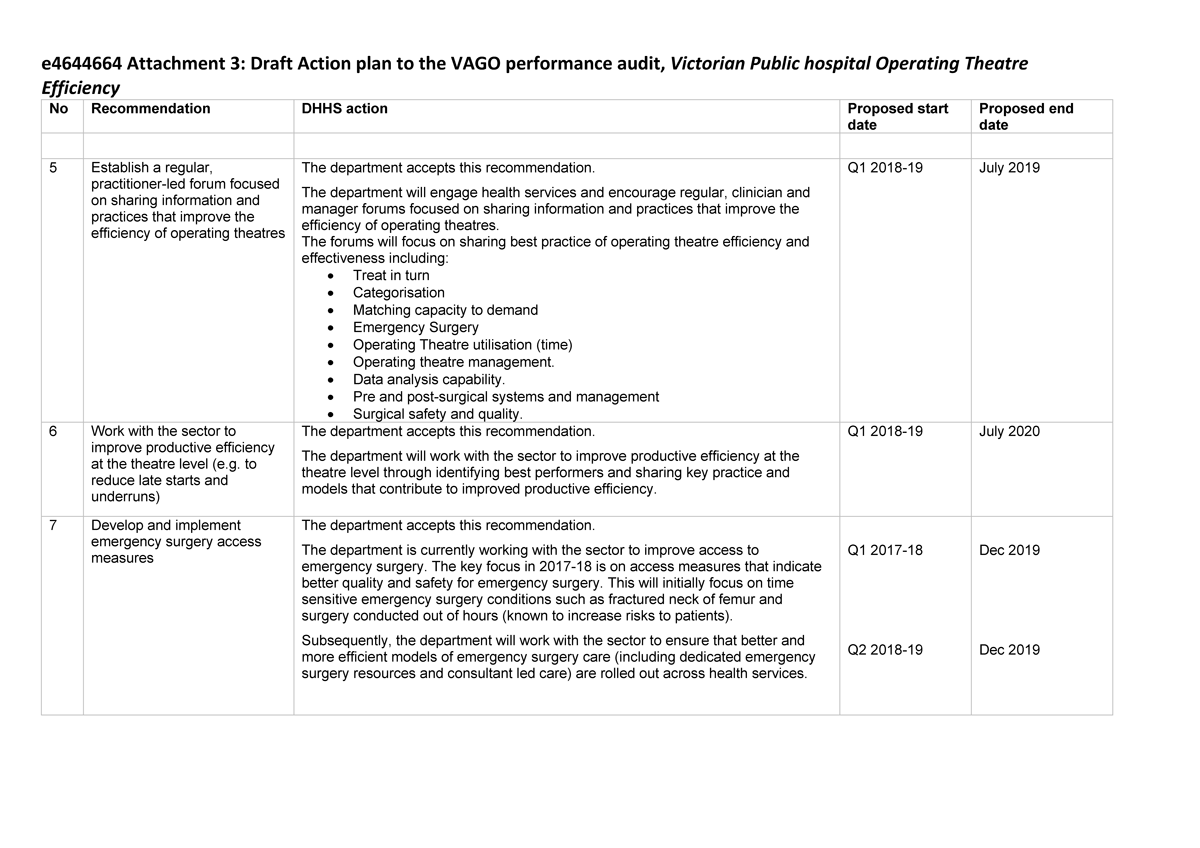
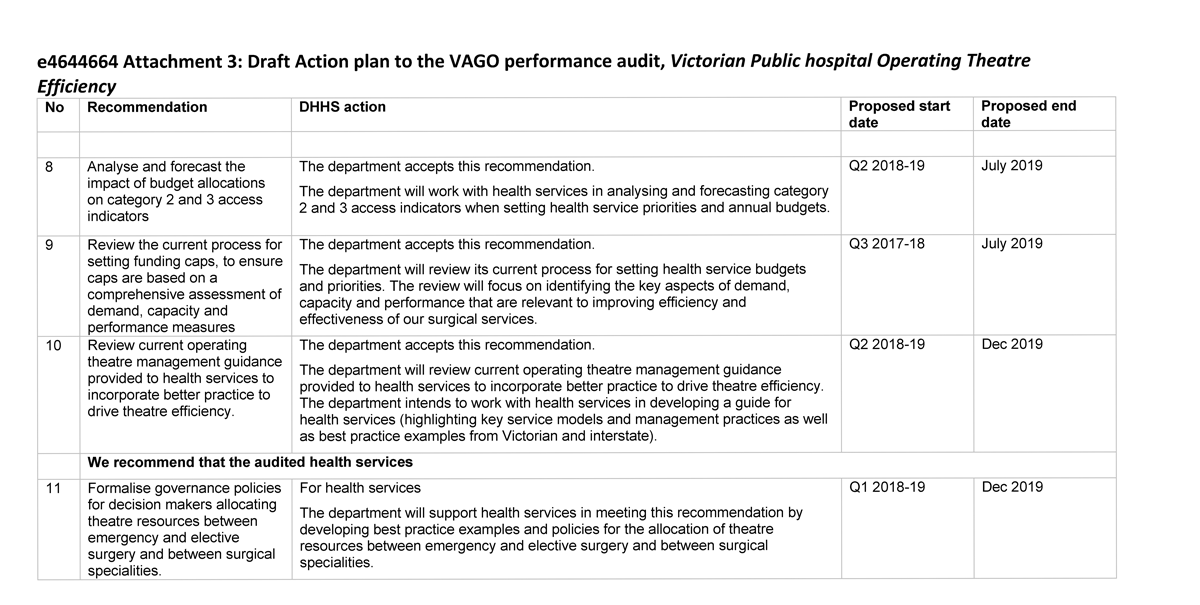
Response provided by the Chair, Board of Directors, Alfred Health
RESPONSE provided by the Executive Director, Clinical Operations and Imaging Services, Austin Health
Appendix B. Data quality
DHHS does not collate health services' operating theatre data into a statewide dataset, and therefore does not centrally govern, audit and assure health services' theatre data. The weaknesses in the data outlined in this appendix result from the lack of central governance.
There is significant variation in health services' data quality due to a lack of central governance. Introducing a statewide framework for governance of the theatre data, combined with consistent definitions and measures, would enable performance evaluation across the health system.
Inaccuracies in data
Data inaccuracy is the first major issue we identified in this audit. We applied logic rules and found that 5 per cent of records across the state had at least one error—such as recording that anaesthesia started after the operation commenced. However, this methodology cannot identify incorrect timestamps when they record sequential times.
Melbourne Health conducted an audit in 2016 to compare the recorded timestamps with the time the event actually occurred. They found 26 per cent of the records were accurate, 52 per cent had an error of less than 10 minutes and 22 per cent had an error of between 15 and 48 minutes. Since then, Melbourne Health has prioritised data improvement through its Theatres Transformation Project.
Although undetected data quality issues are present in the dataset we compiled, we expect the impact on our analysis to be low because we are reporting across a large number of records, and the Melbourne Health audit shows the degree of error is likely to be low.
Variation in data fields and terminology
Another major issue with data collection in the health services is the variability of the data fields collected. Health services collect different sets of timestamps and not all health services record the full set needed to assess theatre efficiency due to limitations in their IT systems or business rules. Only two health services were able to provide the full set of fields requested, and the lowest score of completeness was 77 per cent of the fields.
Health services also use data fields with the same name differently, such as the point in the surgery used to define 'surgery start'. This makes aligning data complicated and subject to error. In some cases, the combination of timestamps kept and definitions used do not enable the data to be accurately aligned across the 23 ESIS health services.
Common additional data errors we encountered included:
- terminology being defined in different ways
- different names being used for the same thing—for example, procedure names being abbreviated in different ways
- multiple rows of data being recorded for the same operation
- surgical session usage or length not being recorded accurately.
In the case of three health services, we determined that they recorded their data so differently from the other 20 health services that we could not include them in our reporting. For example, one health service's IT system records surgical sessions as running for 24 hours, which does not reflect reality and affected their reported efficiency rates in our dataset.
Appendix C. Assumptions and methodology
In this audit, we analysed efficiency in various ways, as described in Part 1. The health services currently use some of the measures in their internal reporting. We developed some measures to test issues identified by our engagement with health services, DHHS, stakeholders and subject-matter experts. This appendix outlines the assumptions and qualifications that apply to each measure.
Universal assumptions
We used a range of assumptions and measures, which apply throughout the report unless specified:
- We measured performance in ways that are most within the health services' control—we focused on business-day elective sessions, as this activity is a fairer measurement of management's performance.
- The available data has limited us to particular sorts of analysis, and we identify this in relevant parts of the report when it has affected the results.
- We excluded health services from certain measures when we were not satisfied with the quality of the data or how it reconciled with data provided by other health services.
- Theatre timestamps lack centralised governance, and health services do not necessarily collect all the possible timestamps. 'Procedure stop'—the time when the operation finishes—was provided to us by all of the health services and has been our default point for recording the end of a surgery. However, we acknowledge that this may reduce performance results for some measures such as utilisation rate and turnaround time.
- Health services collect data in their theatre data system in their operating theatres, procedure rooms and some ad hoc 'work around' locations. We have only reported on surgery that occurs in full operating theatres.
Utilisation rate
The utilisation rate discussed in Part 2 includes any elective and emergency procedures that occurred within business-day elective sessions. Session utilisation begins at 'anaesthetic start' and concludes at 'procedure stop' or 'anaesthetic stop'.
Some theatres have attached anaesthetic bays, which enable 'parallel processing'—the next patient can begin the anaesthetic process while the previous patient is still in the theatre. In this audit, we counted anaesthesia and the operation in the utilisation rate to mitigate the impact of different theatre infrastructure across the health services.
Late starts
To assess the frequency of late starts, we analysed morning elective sessions conducted on business days to mitigate the impact of emergency surgery and overrun morning sessions on our performance analysis. We had difficulties aligning each health service's timestamps as definitions vary across the sector. For this reason, our results may vary from those that health services report internally.
Health services also did not consistently record reasons for delays—either not recording delays or using different terms and definitions for their recorded reasons.
Underruns and overruns
Underruns and overruns assess the time difference between the conclusion of the session's last procedure and the session's scheduled finish. We have measured the end of the last elective or emergency surgery that occurred relative to the end of the elective session.
Unused capacity
This measure records whether health services scheduled a surgical session in a theatre on a business day. We have not limited the type or length of the surgical session. We define an unstaffed theatre as being 'unused', though the available data does not tell us the reason why it was unused.
Cost efficiency and specialisation
Health services provided us with procedure-based data that enables us to view data at the theatre, procedure and speciality levels. However, as this data comes from the theatre systems, much of the terminology is inconsistent. For example, the names used to describe procedures differ significantly between health services. We attempted to standardise the data to create a common dataset, but we could not link all procedures because of data limitations.
Consultants and registrars
We attempted to identify whether a consultant or a registrar performed each procedure to evaluate the impact of teaching on efficiency. Unfortunately, not all health services' data enabled us to identify the surgeon's status. The reported results comparing surgical length only include operations when we could clearly identify the surgeon's status.
Appendix D. Specialisation
We identified that the length of an operation falls as the surgeon performs more of that particular operation.
To demonstrate this, we examined six common surgeries that are performed by consultants in Victoria. In five of the surgeries we examined, the duration of the operation was shorter when it was performed by the top 10 highest-volume surgeons compared to surgeons who had performed the procedure 10 or fewer times, as shown in Figure D1. In three cases the difference was over 20 per cent.
The data did not enable us to identify the methodology used to deliver the operation or if there were complicating factors. Incorporating this information into the data captured would enable health services to better benchmark the average duration of particular operations.
Figure D1
High- and low-volume surgeon efficiency (average minutes per procedure)
|
Surgeon |
Appendectomy |
Fractured neck of femur |
Hip replacement |
Knee replacement |
Cataract surgery |
Coronary artery bypass |
|---|---|---|---|---|---|---|
|
Top 10 by volume |
47.7 |
59.8 |
99.0 |
92.3 |
20.6 |
223.4 |
|
≤ 10 operations |
53.1 |
62.7 |
119.5 |
118.6 |
25.9 |
220.6 |
|
Difference |
11% |
5% |
21% |
28% |
26% |
–1% |
Source: VAGO.
Health services can improve efficiency by scheduling surgery in a way that concentrates types of operations with surgeons so that their clinicians undertake higher volumes of particular operations.
Each operation tested is shown in Figures D2 to D7.
Figure D2
Appendectomy performed by a consultant at the ESIS health services, 1 July 2014 to 31 December 2016
Source: VAGO.
Figure D3
Fractured neck of femur performed by a consultant at the ESIS health services, 1 July 2014 to 31 December 2016
Source: VAGO.
Figure D4
Hip replacement performed by a consultant at the ESIS health services, 1 July 2014 to 31 December 2016
Source: VAGO.
Figure D5
Knee replacement performed by a consultant at the ESIS health services, 1 July 2014 to 31 December 2016
Source: VAGO.
Figure D6
Cataract surgery performed by a consultant at the ESIS health services, 1 July 2014 to 31 December 2016
Source: VAGO.
Figure D7
Coronary artery bypass performed by a consultant at the ESIS health services, 1 July 2014 to 31 December 2016
Source: VAGO.
Appendix E. Financial accounting consistency
DHHS mandates a common chart of accounts for health services to drive standardisation in recording financial information. However, we found significant inconsistency in how health services use the accounts.
Compiling a shared financial dataset required significant data manipulation to overcome the variation. Even then, attributing some costs was challenging, and undertaking analysis to the level we wanted was impossible. For example, we could not distinguish between costs used to deliver emergency and elective surgery or for surgery that occurs within or outside business hours. Due to the lack of comparable data, health services are unable to benchmark their costs and efficiency.
Figure E1 shows the variation in how the four audited health services capture anaesthetic salaries. The use of different cost centres, evidenced by the different numbers used, is a significant barrier to the easy comparison of costs between health services. This is one example and indicative of the inconsistencies in how the health services use the chart of accounts.
Figure E1
Anaesthetic cost centres used at audited health services
|
Cost centre |
Alfred Health |
Austin Health |
Melbourne Health |
SVHM |
|
|---|---|---|---|---|---|
|
A4152 |
Anaesthetics |
|
|
✔ |
|
|
A4155 |
Anaesthetics HMO |
|
|
✔ |
|
|
A8252 |
Anaesthesia |
✔ |
|
|
|
|
Anaesthesia salaries |
|
✔ |
|
|
|
|
Anaesthetics |
|
|
|
✔ |
|
|
A8254 |
Anaesthesia external medical staff CLOSED USE A4190 |
|
✔ |
|
|
|
HMO Anaesthesia |
✔ |
|
|
|
|
|
A8257 |
Anaesthetics |
|
|
|
✔ |
Source: VAGO.
Appendix F. Health services' operating theatre performance
We collected operating theatre data from the 23 health services that report to ESIS, and collated it into a dataset. Figure F1 outlines the 23 health services' results against common performance indicators. Health services use their own efficiency measures with different underlying assumptions. Our data, therefore, may differ from the health services' internal reports, as we have applied our own definitions.
Figure F1
Health services' theatre performance against key utilisation measures
Note: The table excludes Health Services H, O and P due to underlying data issues.
Note: Cells are blank if health services do not collect the relevant data point (generally 'anaesthetic stop').
Note: All data is for the period 1 July 2014 – 31 December 2016 except for 'unused capacity', which covers 1 July 2016 – 31 December 2016. The shorter period is used for 'unused capacity' to account for new theatres being opened over the full date range, which affects the results.
Source: VAGO.