Carer Support Programs
Overview
There are approximately 700 000 informal carers in Victoria, including around
194 000 primary carers, providing unpaid care to a relative, partner or friend. Carers contribute greatly to our community, but often at a physical and emotional cost to themselves. Carers need access to effective, equitable and timely supports to help them continue in their role.
This audit examined whether the departments of Health and of Human Services effectively recognise and support carers.
The departments fund a range of carer support programs and recognise that supporting carers is core business. However, they do not treat carer support programs with the rigour that core business warrants.
The departments cannot demonstrate the timeliness or effectiveness of the carer support programs they fund because they do not monitor wait times or outcomes against program objectives. Despite demonstrated effort by the departments and service providers to promote carer supports, carers lack awareness of them. The departments have yet to attempt to understand and address why current promotion strategies are not more effective.
Carers have difficulty navigating the service system. The departments and service providers do not consistently assess, either directly or by referral, the needs of carers they interact with. This means carers who need and want support
may miss out. The equity of carer supports is compromised by inconsistent prioritisation practices and management of brokerage funds.
To facilitate carers’ access to support programs and demonstrate program effectiveness, the departments need to understand how carers find out about supports, require consistent carer identification and needs assessments and monitor wait times and outcomes against program objectives.
Carer Support Programs: Message
Ordered to be printed
VICTORIAN GOVERNMENT PRINTER August 2012
PP No 161, Session 2010–12
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report on the audit Carer Support Programs.
Yours faithfully
D D R PEARSON
Auditor-General
15 August 2012
Audit summary
A carer is someone who cares for a relative, partner or friend on an unpaid, informal basis. Carers enable many people to remain living in their homes and communities. This also reduces the financial burden on the health and human services systems. In 2010, Carers Australia estimated that informal carers provided $40.9 billion in care services nationally. In Victoria, there are over 700 000 informal carers, including 194 000 ‘primary carers’, providing support to someone for most of their daily living activities.
While carers contribute greatly to our community, they often do so at an emotional, physical and financial cost to themselves. Carers tend to have poorer health and wellbeing than their non-carer peers and can experience high levels of stress, anxiety and depression as a result of their care responsibilities. Younger carers and those of working age may miss educational or employment opportunities that then affect their ability to participate fully in the community.
Victorians will rely more heavily on informal care from family and friends in the coming decades. The population is ageing, and the prevalence of physical and mental illness is also on the rise. In addition, State and Commonwealth health and welfare policies continue the shift from institution-based services to community care, in recognition of the benefits of enabling people to stay in their own homes.
Given these challenges, carers need support to maintain their care role, and recognition for the contribution they make. The role of carers is an integral component to the efficient and effective operation of the health and human services systems. Supporting the sustainability and capacity of carers to maintain their role is therefore core business for system managers and service providers.
The Department of Health and the Department of Human Services fund a range of programs to support primary carers. The following departmental program areas provide and manage carer supports:
- the ageing and aged care and palliative care program areas in the Wellbeing, Integrated Care and Ageing division of the Department of Health
- the mental health program area in the Mental Health, Drugs and Regions division of the Department of Health
- the disability program area in the Disability Services division of the Department of Human Services
- the child protection program area in the Children, Youth and Families division of the Department of Human Services.
This audit examined whether the departments are effectively recognising and supporting carers.
Conclusions
The departments recognise carers as important stakeholders in the health and human services systems and the programs they manage. This is evident through the range of supports made available to carers. The departments and service providers also recognise the care relationship. They include and consider carers in policy and program development, and involve them in decision-making with the people they care for.
The departments recognise that supporting carers is core business. However, they do not treat their carer support programs with the rigour core business warrants. This is evident in gaps in data collection, the failure to assess carer needs, and a lack of outcome measurement. Greater rigour around carer support programs is essential to the ongoing development and improvement of these services. Effective carer supports are particularly important, as the departments’ focus on supporting their clients to remain in their homes and communities is reliant on carers.
Carers experience barriers to accessing supports, such as poor awareness of services and difficulty navigating service systems. The departments’ lack of referral processes, needs assessments, and prioritisation practices for carers across each of the program areas contributes to this. The department and service providers do not identify many carers who may benefit from support services. Inconsistent practices also raise the risk of inequity, particularly for carers trying to access high-demand services.
Despite clear program objectives, such as reduced stress or improved family functioning, the effectiveness of carer support programs is unknown. The departments do not monitor support programs against outcomes for carers and so cannot demonstrate effectiveness. This is a significant gap given the need for effective programs to support the growing community reliance on carers.
Findings
Accessing supports
The departments fund a range of carer support programs, such as counselling, respite and training. However, many eligible carers can miss out because there is limited awareness of available supports, and lack of assessment and referral processes.
Awareness of supports
Carers frequently reported to this audit that they lack awareness of the available supports. It is also a common finding of departmental evaluations of carer supports. This is despite demonstrated efforts by the departments and service providers to promote carer support programs, for example through print and web media and community expos or events. The departments have yet to attempt to understand what is not working and address the problem.
Carer identification and referral
The departments and their funded service providers do not consistently assess, either directly or by referral, the needs of carers they interact with to identify and provide assistance to those who may need and want support. It is therefore likely that some carers in need are missing out.
All program areas have systems in place to identify and record the existence of a carer. Three of the five audited program areas have guidance to prompt staff and service providers to assess carer need, or refer them for assessment and support:
- The Home and Community Care service, in the ageing and aged care program, has a standard tool to assess carer need.
- The palliative care program adopts national assessment tools for its service providers to use on a voluntary basis.
- The standard kinship carer assessment tool prompts the child protection worker to consider the carer's needs and whether they would benefit from a referral to a support service.
However, service providers and departmental staff do not consistently or reliably use the tools in palliative care and child protection.
Consultation with 12 service providers across the five program areas found there was no consistent use of a standardised tool for assessing carer needs. Better identification of carer needs, through referral and assessment processes, would facilitate carer access to supports. This information would also provide the departments with a more complete understanding of their carer population.
Equity of access
Departmental staff and service providers are prioritising carer access to supports differently, and in some cases, subjectively. Consistent prioritisation of carer need is necessary to assure equity and timely access to high-demand services for those in greatest need.
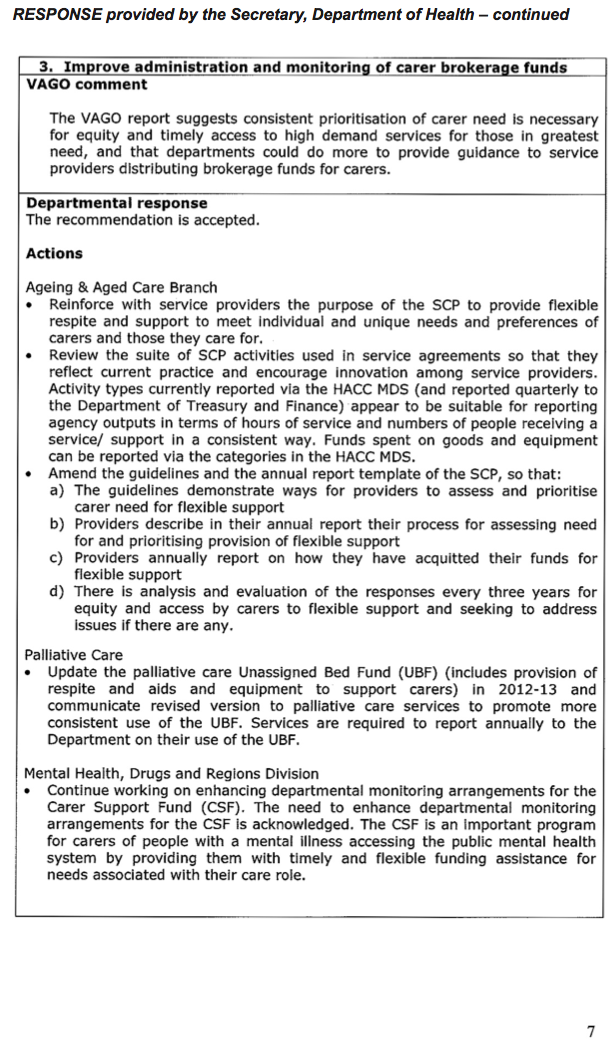
Brokerage funds provide carers with responsive and flexible financial support including assistance to purchase services or one-off material items. The departments are not adequately oversighting brokerage funds for carers, or providing enough guidance to the service providers distributing these funds. Variable practices are evident, such as different funding rules between service providers who are administering the same fund, unexplained variations in average amounts paid by service providers, and a lack of independent processes which allows the same staff to make and approve applications. These inconsistencies raise the risk of inequity for carers.
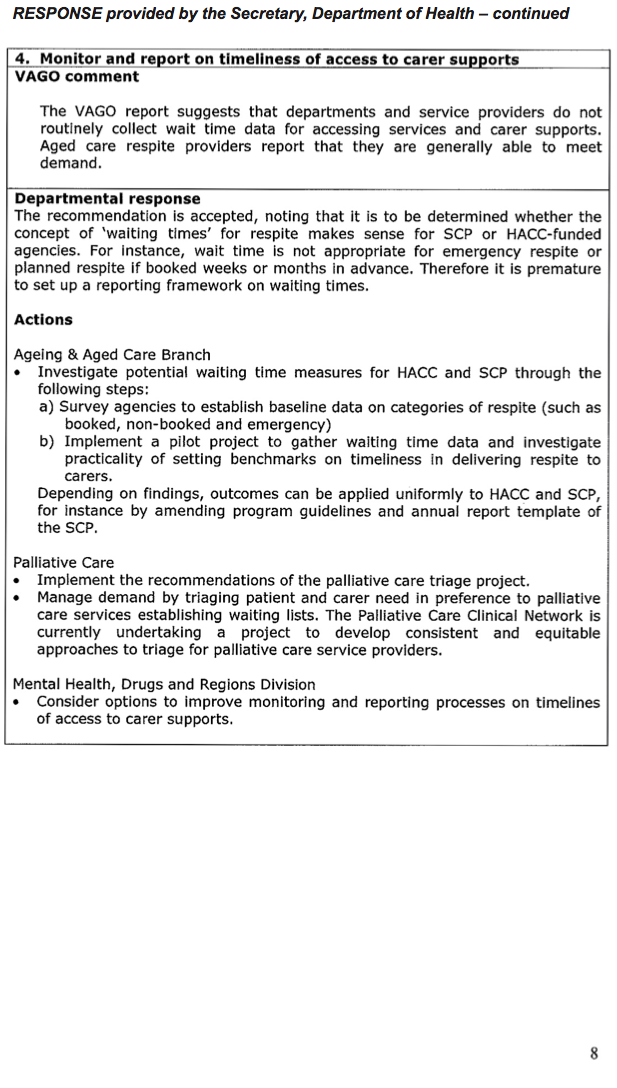
Timeliness of access
Wait time data is one indicator of the service system’s ability to cope with demand. It can provide useful information to departments and service providers for service planning and development work. However, the departments and service providers do not routinely collect wait time data, which means that timeliness of access to carer supports is unknown.
Anecdotal wait times reported by consulted service providers indicate variable performance within and across program areas. Wait times are measured for one carer support only—case management in disability. Wait times for this service vary from just over a week to 12 weeks across geographical areas. Such variation makes it difficult for carers to have any expectation of how long they may wait for a support.
Experience of supports
The departments and service providers are effective in recognising carers and the care role in policy and program development and delivery. However, they cannot clearly demonstrate the effectiveness of carer support programs.
Carer recognition
There is clear departmental policy guidance to program areas and their funded service providers that states they must recognise the role of carers in their service delivery. Departments and service providers have demonstrated a commitment to realising this policy. Across the audited program areas, the audit found many examples of:
- the involvement of carers in program, policy and service development
- the involvement of carers in planning processes with the person they care for
- the inclusion of carer-related standards in quality assurance regimes.
Carers report varied experiences of recognition by the departments and service providers. Many carers we consulted related good experiences where they felt recognised. Some carers, for example, those caring for people with mental health issues, felt that awareness of their role has been increasing over the past decade. However, all had examples where this had not occurred, and in particular, where their needs as individuals were not always considered. These experiences indicate the ongoing need for effort to embed a culture of carer recognition in service provision.
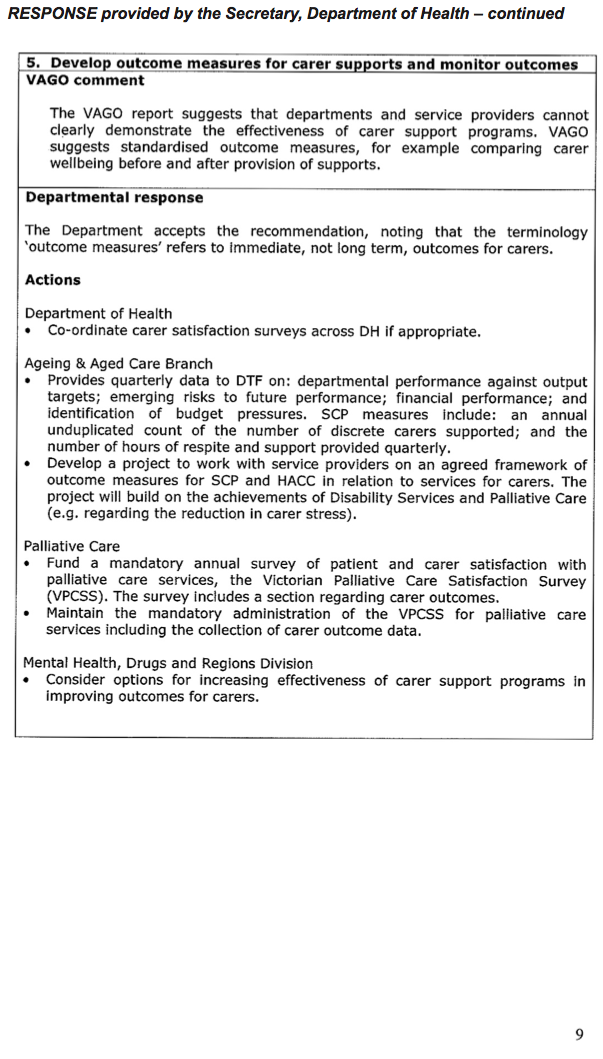
Effectiveness of supports
The departments are not monitoring outcomes against program objectives to demonstrate the effectiveness of carer supports. Objectives of carer support programs include reducing carer stress, sustaining the care relationship, or improving family functioning. However, consultation with service providers revealed only isolated, ad hoc use of carer-related outcome measurement tools.
The departments have undertaken one-off evaluations of most carer support programs. However, these provide only limited assurance of effectiveness. Often evaluations do not address the objectives of the program, review only a narrow part of a service, and cannot determine effectiveness due to a lack of data on carer-related outcomes.
Recommendations
That the Department of Health and the Department of Human Services:
- identify and address gaps in the promotion of carer supports to improve carer awareness of services
- require consistent carer identification and needs assessment
- improve administration and monitoring of carer brokerage funds
- monitor and report on timeliness of access to carer supports
- develop outcome measures for carer supports and monitor outcomes.
Submissions and comments received
In addition to progressive engagement during the course of the audit, in accordance with section 16(3) of the Audit Act 1994 a copy of this report was provided to the Department of Health and the Department of Human Services with a request for submissions or comments.
Agency views have been considered in reaching our audit conclusions and are represented to the extent relevant and warranted in preparing this report. Their full section 16(3) submissions and comments however, are included in Appendix A.
1 Background
1.1 Introduction
A carer is someone who cares for a relative, partner or friend on an unpaid, informal basis. They may care for someone who is aged, has a disability or mental illness, is terminally ill, or for a related child who can no longer live with their parents. A carer who supports a person in most of their daily activities, such as dressing, eating or social activities, is called a ‘primary carer’.
According to the Australian Bureau of Statistics (ABS) in 2009, 703 000 people, or 13 per cent of Victoria’s population, identified themselves as carers of an aged person or someone with a disability. Of this group, 194 000 identified themselves as the primary carer. The ABS figures do not include carers of people with a mental illness or those caring for related children, called kinship carers.
Kinship carers are family members who care for a child who can no longer be cared for by their parents. This arrangement can be termed ‘formal’, due to the involvement of child protection, or ‘informal’, if child protection is not involved. According to Australian Institute of Health and Welfare data, there were over 2 275 formal kinship carers in Victoria in 2011. The Department of Human Services (DHS) estimates that the number of kinship carers is approximately 10 000 when informal care is included.
Another carer group who are often unrecognised, as they do not identify with the term ‘carer’, are young carers. Carers Victoria estimates there are 105 000 carers under the age of 25 in Victoria.
Victoria will rely more heavily on carers over time. Census data reveals Australia’s population is ageing, and the prevalence of physical and mental illness is also on the rise. As the number of people requiring care increases, and as health and welfare services have moved from institution-based to community care, society’s reliance on carers will increase.
In 2010, Carers Australia estimated that informal carers provided the equivalent of $40.9 billion in care services nationally. Care provided by informal carers reduces the financial burden on the healthcare and human services systems. To sustain the current trend of community and home-based care, carers need support to maintain their care role.
1.2 Carer needs
Carers are not a homogeneous group. They have different needs depending on their age, cultural and ethnic backgrounds and socio-economic status, as well as the needs of the person they care for. However, care responsibilities put additional strains on all carers and affect their financial position, social connections, and health and wellbeing. Commonly, carers are:
- more likely to live in households with below-average incomes. Carers of working age who have had to leave the workforce often experience immediate and future financial hardship, with lost income and less superannuation. Young carers can miss schooling and higher education opportunities
- more likely to have a disability themselves, with 35 per cent of carers having a disability compared with 22 per cent of the general population
- more at risk of mental health problems, such as stress or depression, than other people of the same age
- more likely to suffer declines in their physical health—in 2006, DHS reported that over 50 percent of carers suffered a decline in physical health due to caring, 30 percent reported physically injuring themselves, 70 percent reported persistent low energy and 60 percent reported feeling that their care role reduced their options in life opportunities.
The programs in place to support carers, therefore, need to be able to meet a range of needs, such as assistance with daily tasks, respite from the care role, and counselling and emotional support.
1.3 Carer supports
Common types of carer supports include:
- Respite—provides support for the person receiving care, enabling short-term breaks for carers. Respite care can include overnight stays in residential facilities, day-care or outings, in-home care, community programs, camps or other flexible arrangements.
- Case management—provides assistance with coordinating and facilitating access to supports and services.
- Counselling—provides emotional and psychological support for carers in order to reduce stress and assist with coping strategies.
- Financial support—provides assistance in the form of payments or brokerage funds for goods or services to assist carers to perform their care role.
- Carer advocate/consultant—provides advocacy and peer support.
- Information services—provide carers with access to information, such as: emergency services, carer support, domestic and nursing care, respite options and council services.
- Education and training—provides information and skills to assist carers to carry out their care role safely and effectively.
1.3.1 State-funded carer supports available
The Department of Health (DH) and DHS deliver a range of supports for primary carers. Figure 1A lists the state-funded supports available to carers, the funding provided, and available carer participation rates, as collected by departments. The Commonwealth Government also funds a range of carer supports, including carer payments and the National Respite for Carers Program that funds respite, support and counselling. It is a major contributor to Home and Community Care (HACC) services that carers, particularly those caring for older or disabled persons, can access.
Figure 1A
State-funded carer supports
Aged care(a) |
Palliative care |
Mental health |
Disability |
Child protection (kinship carers) |
|
|---|---|---|---|---|---|
In and out of home respite |
Yes |
Yes |
No(c) |
Yes |
No(e) |
Flexible respite |
Yes |
Yes |
No |
No |
No |
Case management |
Yes |
Yes |
No |
Yes |
Yes |
Brokerage |
Yes |
Yes |
Yes |
No |
Yes(f) |
Support groups |
Yes |
Yes |
Yes |
Yes |
Yes |
Counselling |
Yes |
Yes |
Yes |
No |
No |
Education/Training |
Yes |
Yes |
Yes |
Yes |
Yes |
State funding 2010–11 (million) |
$33.4 |
$18 |
$8.2 |
$127.9 |
$13.1 |
No. of carers accessing supports (approx.) |
12 200(b) |
13 000 |
3 000(d) |
15 000 |
1 500 |
(a) Includes selected activities through HACC services and the Support for Carers Program.
(b) Approximate figures due to missing/incomplete records.
(c) The Commonwealth funds mental health respite services.
(d) Carers accessing carer support groups, counselling and training are not included in the figure provided as the department does not collect participation data for these activities.
(e) DHS does not fund a respite program for kinship carers. However, departmental policy states that respite is available to all children in out of home care. In practice, carers may be able to access it on an ad hoc basis through their own networks or volunteers within the foster care system. Respite carers can claim reimbursements on these occasions.
(f) Brokerage funds are available to support all children where child protection is involved, and so while kinship carers can access the funds they are not solely aimed at them.
Source: Victorian Auditor-General’s Office.
The state allocates approximately $200.6 million per year for these programs to support approximately 44 700 carers. This includes $21.4 million to HACC respite and day programs through aged care, and $89.4 million to disability respite. The aim of these respite programs is to provide support for the person receiving care to engage in activities (from a couple of hours during the day up to several weeks) such as community programs, camps, holidays, overnights stays, thereby providing the carer with a break from their role. HACC also provides personal care and domestic assistance services which some 40 000 carers can benefit from indirectly.
The remaining $89.8 million goes towards supports that aim to assist the carer directly in their care role and as an individual, such as counselling, facilitation of support groups, education and training, and brokerage funds. Uniquely among the audited program areas, DH funds Carer Consultant positions located in Area Mental Health Services. Carer Consultants have lived experience of caring for someone with a mental illness. They can provide direct support to families and carers, as well as inform service and program planning activities at their service.
Volunteers play an important role in supporting carers in palliative care and disability. There is no current data on the numbers of volunteers in these areas.
1.4 Legislation
Carers Recognition Act 2012
The Carers Recognition Act 2012 (the Act) is intended to recognise and support the needs of people in care relationships, and enact principles to ‘promote understanding of the significance of care relationships’. This legislation brings Victoria in line with Commonwealth legislation and that of four states and one territory.
The Act acknowledges that carers are in a shared arrangement involving the person providing care and the family member or friend for whom they care. Each person in a care relationship should be respected, recognised and supported as an individual.
The principles supported in the Act include that a carer should:
- be recognised as an individual with his or her own needs
- be recognised for the social and economic contribution to the whole community arising from his or her role as a carer
- have his or her social wellbeing and health recognised in matters relating to the care relationship
- have the effect of his or her role as a carer on his or her participation in employment and education recognised and considered in decision-making.
Organisations receiving funds from DH and DHS to provide services or programs that directly impact on carers are obliged to make sure that staff and carers have an awareness and understanding of these principles and reflect them in developing, providing and evaluating services. Funded service providers must report compliance with these obligations in their annual report.
1.5 Departmental responsibilities and policies
DH and DHS are responsible for developing policy and delivering and funding programs to support carers. Figure 1B shows the departmental divisions and program areas that lead this work.
Figure 1B
Departmental divisions and program areas
Departmental division |
Program area |
|---|---|
Department of Health |
|
Wellbeing, Integrated Care and Ageing |
Ageing and aged care |
Palliative care |
|
Mental Health, Drugs and Regions |
Mental health |
Department of Human Services |
|
Disability Services |
Disability |
Children, Youth and Families |
Child protection |
Source: Victorian Auditor-General’s Office.
The departments deliver carer supports directly but also fund a range of community service organisations to deliver carer supports. These supports target primary carers. Regional department staff monitor the performance of these service providers against funding and service agreements.
Recognising and supporting care relationships (2006)
The Recognising and supporting care relationships policy provides a framework for departmental staff and funded service providers to support informal care by focusing on the relationship between the carer and the person being cared for.
The policy recognises that each person in the relationship can have different needs and outlines three principles to support the care relationship:
- recognition and respect
- support
- participation.
Victorian Charter Supporting People in Care Relationships (2010)
The charter acknowledges the role of carers in our society. It articulates the rights and responsibilities of people in care relationships, and how they can be supported by organisations, governments and the community. The charter states that those in 'care relationships’ should be:
- recognised and respected
- supported to access services
- supported through community awareness raising
- able to take part in care planning and making decisions about care.
The charter is aimed at people in care relationships, government departments and funded service providers. The principles in the charter were used as a foundation for the Carers Recognition Act 2012. A revised charter will be released in 2012 to reflect the new legislation. The Act and the charter guide DH and DHS program activity and funded service provision.
1.6 Audit objective, scope, method and cost
The audit assessed the extent to which DH and DHS are effective in recognising and supporting people who care for others by examining whether:
- supports and services are accessible to carers
- agencies’ practices recognise the role of carers and provide effective support.
The audit covers the support provided and funded by the departmental divisions and program areas as shown in Figure 1B.
Funded community service organisations and carers were included as stakeholders, through interviews with 12 service providers and consultation with 37 carers.
Part 2 of the report examines carers’ access to support programs. Part 3 looks at carer recognition and the effectiveness of supports.
The audit was undertaken in accordance with Australian Auditing and Assurance Standards.
The audit cost was $290 000.
2 Access to carer supports
At a glance
Background
Carers play a vital role in the community and need support to maintain this role. This requires community awareness of the supports that exist and for carers to understand how to access them. Access processes should be transparent and equitable, and supports should be flexible and responsive to carer needs.
Conclusion
Many eligible carers miss out on support due to barriers to accessing services. Carers lack awareness of supports available despite demonstrated efforts by the Department of Health, the Department of Human Services and service providers to promote them. The departments have yet to analyse and address this problem.
Carers have difficultly navigating the service system and there is a risk of inequity in accessing supports. The departments and service providers do not routinely or systematically assess and prioritise carer need, refer them to supports, or monitor wait times for services. Access to brokerage funds is not consistent or transparent.
Findings
- Carers lack awareness of supports.
- The departments have not evaluated promotion strategies, and service providers do not routinely monitor referral sources.
- The departments and service providers do not have a consistent approach to assessing or prioritising carer needs.
- The departments do not adequately monitor brokerage funds for carer supports.
- Lack of wait time data means the timeliness of access to supports is unknown.
Recommendations
That the Department of Health and the Department of Human Services:
- identify and address gaps in promotion of carer supports to improve carer awareness of services
- require consistent carer identification and needs assessment
- improve administration and monitoring of carer brokerage funds
- monitor and report on timeliness of access to carer supports.
2.1 Introduction
Carers are a vital part of the health and human services system and provide over $40 billion in care nationally. Care provided by informal carers reduces the financial burden on public services and helps to maintain family and community connections.
Carers need a range of flexible services to support them to continue in their care role. Supports need to be responsive to urgent needs and enable carers to build their capacity and plan for the future.
Not all carers identify with the term ‘carer’ and may not seek or be aware of carer support services. Staff in the broader health and human service systems play an important role in identifying carers and facilitating their access to carer support services. Consistent carer identification and referral improves opportunities for carers to access supports.
Access to supports should be transparent, equitable and timely for all carers. Consistent use of carer needs assessments and tools for prioritising urgency of need provide assurance to the community that carers are supported consistently and fairly.
2.2 Conclusion
The departments of Health (DH) and of Human Services (DHS) provide a range of supports to meet a variety of carer needs across their program areas. However, carers cannot always access the supports available to them. Carers lack awareness of supports, despite departmental and service provider efforts to promote them. The departments have not evaluated promotion strategies to determine the cause of this. Carers also have difficulty navigating the system and the departments and their funded service providers do not reliably refer carers to support programs.
There is potential unmet demand for carer supports, but its extent is unknown. Departmental and service provider staff and processes do not consistently identify carers as having needs of their own, assess these needs or refer for assessment, or monitor wait times to access services.
Improvements to the equity and accessibility of supports are necessary to assist carers to maintain their care role and to help address the higher levels of stress and poorer wellbeing they experience compared with their peers.
2.3 Awareness of carer support programs
Carers can access support through a referral from another service or by contacting the service provider directly—‘self-referral’. Health and community services, such as general practitioners, hospitals, aged care homes, disability or mental health services, local government, and schools, need to identify carers and be aware of the carer supports available to facilitate access to them. Carers report a lack of awareness of supports despite demonstrated efforts by the departments and their funded service providers to promote them.
2.3.1 Promotion
The departments and their funded service providers adopt a range of promotion strategies to raise awareness of supports among carers and other health and community services. The method and extent of promotion depends on individual service providers, geographical location and the support type. Strategies include:
- networking between service providers
- distribution of brochures and promotional resources to health centres
- attendance and promotion at local and regional expos and events
- publishing information in regular newsletters, local papers and regional bulletins
- advertising on radio and television broadcasts
- website and internet promotion
- some service providers report using innovative promotional strategies such as smart phone applications and online promotional videos to market their services and raise broader community awareness
- departmental funding of advisory or peak bodies, such as the Kinship Carers Peak Advisory Body.
Effectiveness of promotion
Carers routinely report a lack of awareness of the supports available. Figure 2A provides a summary of program evaluation findings since 2001 relating to promotion and awareness of supports.
Figure 2A
Summary of promotion and awareness findings
Program area/evaluation |
Finding |
|---|---|
Support for Carers Program (SCP) evaluation (2001)(a) |
Carers found it ‘difficult to find information’ about supports |
Aged care |
|
SCP and HACC(b) evaluation (2011) |
‘…carers did not know about services’ |
Mental health |
|
Carer Support Program evaluation (2008) |
‘…further work in promoting availability of the [Carer Support Fund] is required’ |
Disability |
|
Respite report (2009) |
There is a need to ‘improve the understanding of families/carers…of the variety of respite support services available’ |
Respite report (2010) |
‘[carers] do not consider they are sufficiently informed about the types of carer supports that are available’ |
Child protection (kinship carers) |
|
Kinship care policy review (2007) |
There is a ‘lack of information’ for kinship carers |
(a) The 2001 Support for Carer Program evaluation applied to support programs across ageing and aged care, mental health and disability program areas.
(b) Home and Community Care (HACC).
Source: Victorian Auditor-General’s Office.
Despite these repeated findings, the departments have not undertaken any evaluation of promotion strategies and service providers do not routinely monitor their referral sources. Consultation with 12 funded service providers revealed only one example of a service provider performing a formal evaluation of their promotion methods by asking carers how they found their service.
2.4 Carer identification and referral
The Carers Recognition Act 2012 states that carers should be supported as a person with their own needs as well as in their role as a carer. For this to be realised, service providers need a consistent practice of carer identification and needs assessment. This would increase carers’ awareness of, and access to, the supports available, and improve the departments’ understanding of the carer population.
All program areas have systems in place to identify carers and to record this. However, the extent to which the departments have guidance designed to prompt their staff and service providers to assess carer need, or refer them for assessment and support, is variable. Figure 2B provides an overview of current systems and guidelines to identify carers and consider referral to carer support.
Figure 2B
Carer identification and referral
Aged care and HACC |
Palliative care |
Mental health |
Disability |
Child protection (kinship care) |
|
|---|---|---|---|---|---|
Carer identification |
|||||
System in place |
Yes |
Yes |
Yes |
Yes |
Yes |
Reliable |
Yes |
Yes |
No |
Yes |
Yes |
Carer referral |
|||||
Formal guidance |
Yes |
Yes |
No |
No |
Yes |
Reliable |
Yes |
No |
No |
No |
No |
Source: Victorian Auditor-General’s Office.
Carer identification in Area Mental Health Services (AMHS) and Psychiatric Disability and Rehabilitation Support Services (PDRSS) is not reliable and, as a result, DH’s records are incomplete. To comply with the National Mental Health Standards, all AMHS and PDRSS providers must identify carers as early as possible during their client’s episode of care. However, these services do not reliably identify carers at intake. Instead, mental health clinicians often identify carers later in treatment and then do not update departmental systems.
Child protection workers reliably identify kinship carers and effective use of their assessment tool could result in a referral for carer support. However, child protection staff do not reliably or consistently undertake the assessment. The department has identified staff workload and resources as a reason for this.
Disability services guidelines for staff working with clients to plan their Individual Support Package state that they should consider family or carer needs in the planning process. However, there is no guidance to direct staff to consider referral of carers to supports specifically for them. The Disability Services division in DHS has recently produced the draft ‘Family-centred, person-centred’ practice guide which will address this gap and provides guidance on considering family and carer needs, and making referrals or identifying alternative funding sources for carer supports.
Departmental guidelines for aged and palliative care prompt staff to consider referring the carer to dedicated carer supports. Figure 2C provides a case study of the Home and Community Care (HACC) carer identification and assessment guidance.
Figure 2C
HACC carer identification and assessment guidance
The HACC assessment guidelines Strengthening assessment and case planning set out the principles and practice for assessing people’s needs for community-based care to enable them to remain living as independently as possible.
HACC assessors identify and assess these needs through the ‘Living at Home Assessment’. An important component of this assessment is a holistic needs assessment that looks at the needs of the individual as well as their family or carers’ needs, goals and aspirations. The guidelines include carers in the target group for HACC assessments. The assessment is intended to result in the development of a care plan which takes into account services available in the broader service system, not only HACC services.
Carers of frail and elderly people participating in a focus group revealed varied experience of HACC assessors considering their needs as carers, but overall they were positive about HACC assessment.
Source: Victorian Auditor-General’s Office.
2.4.1 Navigation
Participants in our five carer focus groups stated that they find navigating the system difficult:
- Carers feel either overwhelmed with information or are not able to find out enough.
- Quality case management greatly assists with system navigation, but is not readily available due to long wait times.
- Identification and referral of carers by schools, general practitioners, hospitals (including private psychiatrists and hospitals) would assist with navigation. However, this does not consistently occur and is dependent on individual practice.
- The most common way that carers found out about supports was word of mouth or through support groups.
These comments suggest there is a degree of luck involved in carers finding and accessing supports. Evaluations of carer support programs in Aged Care (2011) and Disability (2009) also highlighted carers’ difficulties in navigating through the system due to lack of adequate information or referrals from other service providers.
2.5 Equity of access
Regardless of where they live or the diagnosis or condition of the person they care for, carers should expect a consistent and fair response from carer support providers. It is important that each program area has processes to assess and prioritise carer needs so that departmental and service provider staff can identify those most in need and distribute finite resources equitably.
There is a risk of inequitable access to carer supports due to inconsistent needs assessment, prioritisation and brokerage fund management practices.
2.5.1 Carer needs assessment and prioritisation
Accessibility of carer supports varies across program areas and services. The departments do not mandate the use of a carer needs assessment tool. Only one program area, palliative care, suggests a range of tools that providers could use. Among the 12 service providers consulted there is no consistent use of a standardised tool for assessing carer needs. Service providers measure urgency differently and in some cases, subjectively. This variability in needs assessment and prioritisation leads to inconsistency in providing supports and raises the risk of inequity.
Seven of the 12 service providers (two each in aged care and palliative care, one each in mental health, disability and kinship care) conduct formal needs assessments. The remaining five assess needs using informal, subjective assessments, such as conversations with carers.
Eight service providers (four in aged care, two in palliative care and one each in disability and kinship care) use a formal prioritisation tool or framework. Within program areas, there is no consistency in the tool used. One disability provider relies on subjective judgement of carer stress levels, or what the worker can ‘hear in the carer’s voice’ when they contact the service. The three remaining service providers (two in mental health and one in kinship care) do not use any prioritisation method.
Carers in our focus groups indicated an awareness of subjective practices in use, saying they often felt they would only receive a service if they exaggerated their need, or sounded desperate. Most carers reported prompt provision of supports in a crisis. However, this was less common for carers of a person with a disability.
2.5.2 Access to brokerage funds
Brokerage funds are available to carers on request to purchase services and one-off material items. These funds should to be responsive and flexible to address a wide range of carers’ needs, and fund guidelines need to be able to accommodate this if the support is to be effective. However, the departments need to balance this flexibility with maintaining transparency, accountability and equity through effective monitoring and governance.
The mental health and aged care program areas offer flexible brokerage funds to support carers. However, there is inadequate oversight of spending from the funds. The guidelines do not specify minimum expectations of service providers in assessing, prioritising or approving applications which has led to inconsistent practices and raises the risk of inequitable access for carers. Figure 2D outlines a number of oversight and equity issues evident in these brokerage funds.
Brokerage funds are not available through the Disability Services division. However, flexible support packages may indirectly support families and carers with discretionary funds to purchase supports aimed at the person with a disability.
Kinship carers can access Placement Support Grants. While they are not aimed towards supporting the carer specifically they can provide financial support through the purchase of goods or services, such as bedding or therapy, to meet immediate needs of the child in the placement. It is not possible to determine the extent to which kinship carers derive benefit from these grants as reporting and acquittal does not categorise the type of placement, either kinship or foster, that funds go to.
Figure 2D
Oversight and equity of carer support brokerage funds
Aged Care Support for Carers Program (SCP) brokerage capacity
In 2011, brokerage accounted for approximately $560 000 of SCP funds in aged care. Consultation with two service providers revealed inconsistent practices regarding the use of funds. For example, one service limits use of funds to the purchase of respite from a number of predefined ‘approved providers’, while the other service will permit use of the funds for the purchase of goods or services if they consider there to be a ‘genuine need’. Service providers are not required to provide acquittals to DH and it is not possible to determine how many applications for funds service providers receive each year.
Mental Health Carer Support Fund (CSF)
There are a number of issues regarding the $1.6 million mental health CSF which relate to inadequate oversight, transparency and accountability.
DH’s Mental Health, Drugs and Regions division has funded an external agency to administer the CSF since July 2009. However, there is no contract or service agreement in place stipulating conditions, targets or performance indicators for this activity.
Application and approval processes handled by staff in Area Mental Health Services (AMHS) are inconsistent and can result in a potential conflict of interest. AMHS Case Managers or Carer Consultants complete applications on a carer’s behalf and applications are approved either by individuals or committees within the AMHS. In some instances the same individuals who complete the applications are responsible for approving them.
Analysis of payments from CSF allocations demonstrates wide, and unexplained variation between different AMHSs in the average amount paid per application, from just under $200 to just over $1 000. The statewide average is $560.
Consultation with Carer Consultants revealed one instance of a service spending their quarterly CSF allocation within the first month. This lack of internal management of spending results in inequitable distribution of the funds to carers in that area.
Analysis of CSF reporting between June 2010 and June 2011 shows that the number of applications to the fund has increased by 17 per cent but underspending has also increased, from 12.5 per cent to 16.1 per cent. Underspending from the fund could indicate a lack of demand or inadequate promotion but ultimately it means that carers are not gaining the full benefit from the resources available to them.
Service providers consulted indicated that underspending results from not receiving timely, monthly reports on their expenditure. However, not all service providers monitor their own CSF spending.
Source: Victorian Auditor-General’s Office.
2.6 Timeliness of access and wait time data
Carer supports are often intended to ‘fill a gap’ or meet an urgent need while waiting for other, more long-term supports, such as an ongoing funding package in aged care or disability. Responsiveness, on these occasions, is crucial to the effectiveness of the program.
The departments do not set timeliness targets and do not require reporting of wait times for carer supports, except for case management provided by the Disability Services division. Service providers do not consistently, or routinely, collect data on wait times.
A number of service providers report that they do not maintain wait lists. They state that they prefer to refer people to other services if they do not have capacity to respond, rather than keeping someone holding on for an extended period of time.
The two disability respite providers consulted monitor their unmet demand: one for internal purposes, the other voluntarily reports it to their regional departmental office. The annual disability carer respite satisfaction survey found that carers offered alternative respite options, such as in-home respite or holiday programs, report low satisfaction due in part to long wait times.
Aged care SCP respite providers do not maintain a wait list and they report they are generally able to meet demand.
2.6.1 Wait times and wait time data
For time-critical services, such as respite, financial support or counselling, a long or indefinite waiting period can have a profoundly negative effect on a carer’s health and wellbeing and ultimately their ability to continue in their role. Wait time data is one indication of the service system’s ability to cope with demand, and can provide useful information to departments and service providers for service planning and development work.
Formal wait time data is not available for carer supports, except for disability case management, as the departments and service providers do not routinely collect it. Departmental wait time data for disability case management shows a statewide average of 51.4 days, or just over seven weeks. The target wait time is 50 days. The data also shows a high degree of variation between departmental regions, from just under one week in one region to over 12 weeks in another.
Figure 2E outlines the anecdotal wait times reported by consulted service providers. It shows variable wait times depending on the type of support, for example access to brokerage funds usually occurs within two weeks while case management or respite can be over a month. Variability within program areas is also evident, such as case management for kinship carers. This makes it difficult for carers to have any expectations of how long they can expect to wait for a support.
Figure 2E
Anecdotal wait times
Type of support |
Aged care(a) |
Mental health |
Palliative care |
Disability |
Child protection (kinship care) |
|---|---|---|---|---|---|
Respite |
Providers report no wait for respite |
Commonwealth funded |
Average 2 days |
No data: one provider reports 4 months |
Urgent: no wait Non-urgent: not available |
Case management |
Average 5 weeks |
Not applicable(b) |
No data |
5–6 weeks |
Variable: 0 to several weeks |
Counselling |
Variable: 3–6 weeks |
Commonwealth funded |
Variable: 0–3 days |
Commonwealth funded |
Not applicable(b) |
Information/advice |
Within 48 hours |
Within 48 hours |
No data |
Within 72 hours |
Within 24 hours |
Training/education |
No data |
Variable: depends on frequency of training session |
No data |
No data |
Sessional (max. 9 weeks) |
Brokerage funds |
1–2 weeks |
Variable: 1–10 days |
No data |
No data |
Not applicable(b) |
(a) SCP service providers only.
(b) Types of supports not available to carers through these programs.
Source: Victorian Auditor-General’s Office.
Carers’ experiences of waiting
The experiences of carers echo the variability that service providers report. Comments from carers participating in our focus groups indicate that wait times vary depending on the condition of the person they are caring for and the type of support they are accessing. For carers of a person with a mental illness access to supports can be quick, ‘but only if you are in crisis’. Kinship carers found that regular carer reimbursements can be established promptly but that the process for accessing reimbursements for one-off expenses is long and burdensome.
Carers participating in our aged care and disability focus groups reported extended periods of waiting—from a couple of months to over a year—for approval to access supports such as planned respite and case management, and then additional periods of waiting prior to receiving those supports. Their comments also indicated a lack of understanding of the reasons behind the long wait times. This suggests that the departments and their funded service providers are not adequately communicating with carers. This uncertainty adds to feelings of helplessness and increases carer stress.
Recommendations
That the Department of Health and the Department of Human Services:
- identify and address gaps in promotion of carer supports to improve carer awareness of services
- require consistent carer identification and needs assessment
- improve administration and monitoring of carer brokerage funds
- monitor and report on timeliness of access to carer supports.
3 Experience of supports
At a glance
Background
As the population ages and the prevalence of chronic disease and disability increases, supporting carers to maintain their role becomes increasingly important. Supports therefore need to effectively achieve their objectives. The Department of Health, the Department of Human Services and service providers also need to recognise carers by involving them in policy and program development, and service planning and provision.
Conclusion
The departments and service providers clearly recognise carers as a group and consistently involve them in policy and program development activities.
The effectiveness of carer support programs is unknown as the departments do not routinely monitor outcomes against program objectives. This is a significant gap given the growing community reliance on carers and increasing need for effective supports.
Findings
- The departments recognise carers as a group, for example, by:
- routinely involving carers in policy and program development
- applying quality assurance processes to service providers that assess carer recognition and involvement.
- The departments have evidence-based carer support programs in place.
- The departments do not use outcome measures to determine the effectiveness of their carer support services.
Recommendation
That the Department of Health and the Department of Human Services develop outcome measures for carer supports and monitor outcomes.
3.1 Introduction
Given our community’s reliance on carers, supporting them to maintain their care role is crucial. As well as identifying individual carers and providing supports to them, recognition of carers as a group is also important. Not all carers will require or want direct supports. However, recognition of their role contributes to more effective and sustainable care relationships. This includes involving carers in care and treatment planning with the person they care for.
The programs designed to support carers must be evidence-based and effective. The objectives of carer support programs range from increasing social connectedness to reducing carer stress. Standardised outcome measures—comparing, for example, carer wellbeing before and after provision of supports—can be used to demonstrate effectiveness of supports against these objectives.
3.2 Conclusion
The Department of Health (DH) and the Department of Human Services (DHS) and their funded service providers recognise carers in many ways, from including them in policy and service development, to promoting policies and guidelines for carer involvement in client planning and service delivery. Quality assurance processes provide independent assurance of how service providers involve carers.
Carers in focus groups conducted for the audit, report varied experiences of recognition by service providers. This indicates the need for ongoing effort to embed a culture of carer recognition in service provision.
The departments developed the current suite of carer support programs following extensive carer consultation and using a comprehensive evidence base, consisting of academic research and program evaluation.
Given the vital need for, and benefits from, supporting carers, the departments’ carer support programs are core activity and they should monitor them accordingly. However, the effectiveness of carer support programs is unknown as the departments do not apply or monitor carer-related outcome measures.
Due to the lack of effectiveness data, understanding performance relies strongly on anecdotal feedback from carers and service providers and one-off, narrowly scoped evaluations which present mixed results. A common finding of these evaluations is the need to develop outcome measures.
3.3 Carer recognition
Community, health and other care services can recognise carers by acknowledging their role, the special knowledge they have of the person they are caring for and the contribution they make to the broader community.
The departments and their funded service providers are effective in recognising carers by involving them in policy and program development activities. However, recognition at the service provision level, by involving them in care planning and decision-making, requires continued effort.
3.3.1 Carer recognition policy
There is clear departmental policy guidance to program areas and their funded service providers that they must recognise and respect the relationship between a carer and the person being cared for in their service delivery. Stakeholders and departmental program staff are familiar with the recognition principles contained in the 2006 policy Recognising and Supporting Care Relationships and the 2010 Victorian charter supporting people in care relationships.
Departments and service providers have demonstrated a commitment to realising this policy. At a strategic level, departments involve carers in program and policy development. At the level of service provision, service providers involve carers in care planning and service development.
Carer involvement in policy development
All program areas have effectively consulted with, and involved carers in, policy development. Methods for involving carers included written submissions, surveys, focus groups, one-to-one interviews and membership of committees and working groups. Figure 3A lists examples of carer involvement in policy development.
Figure 3A Examples of carer involvement in policy development
|
Program/policy |
Method of carer involvement |
|---|---|
|
Carers’ Charter (2010) and the Carers Recognition Act 2012 |
The development of the Carers Charter during 2008 involved four carer focus groups. Facilitators asked carers to identify what makes them feel service staff recognise their role, and whether they think the charter would make a difference to them. A key theme to come out of these groups was that carers felt that legislation is needed to support the principles of the charter. The recently passed Carers Recognition Act 2012 reiterates the principles outlined in the Carers’ Charter. |
|
Mental Health Reform Strategy (2009) |
DH consulted with 80 carers during the development of the 2009 Mental Health Reform Strategy. Implementation of the strategy was coordinated through five working groups, four of which included carer members. |
|
Kinship care policy and service design (2007) |
DHS sought input by calling for comments in response to an issues paper directly distributed to kinship carers and support groups and received 50 responses from carers. It also heard from a total of 71 carers at face-to-face consultation sessions held around the state. This input contributed to the development of the Victorian Kinship Care Model. |
Source: Victorian Auditor-General’s Office.
In late 2011, representatives from the ageing and aged care, mental health and disability program areas and the Children, Youth and Families division in DH and DHS started to meet informally and have started the process of establishing a formal ‘Carers Steering Committee’. The purpose of the group is to provide advice and guidance on the implementation of carer-related policy and initiatives within DH and DHS and across government. This group resembles an earlier ‘Carers Victoria Liaison Group’, maintained by the former DHS. Membership of this group included Carers Victoria. The liaison group has been in recess since the split of DHS, creating DHS and DH, in August 2009. To date, membership of the newly established steering committee has not included Carers Victoria. However, the terms of reference lists Carers Victoria among its stakeholders.
Carer involvement in service provision
At a practical level, service providers can demonstrate the extent to which they recognise carers by identifying and involving them in the provision of care and service development. All audited program areas have state or national standards and monitoring regimes that include minimum requirements for carer recognition. Figure 3B summarises the range of carer-related quality assurance standards and monitoring processes in place across the five program areas.
Figure 3B
Monitoring of carer involvement in service provision
|
Standards |
Aged care |
Palliative care |
Mental health |
Disability |
Child protection |
|
|---|---|---|---|---|---|---|
|
AMHS |
PDRSS |
|||||
|
Carer involvement in care assessment, planning, review |
No |
Yes |
Yes |
No |
Yes |
No |
|
Carer needs assessment |
Yes |
Yes |
No |
No |
No |
No |
|
Provision of relevant information to carers |
No |
Yes |
Yes |
Yes |
No |
No |
|
Access to relevant carer supports |
No |
Yes |
No |
Yes |
No |
No |
|
Carer capacity building |
No |
No |
No |
No |
Yes |
Yes |
|
Carer involvement in service development |
Yes |
No |
Yes |
No |
No |
No |
Source: Victorian Auditor-General’s Office.
The extent of carer involvement required by the standards and the rigour of the monitoring regimes varies across the five audited program areas. All program areas, except palliative care, require external accreditation and independent monitoring against the relevant standards at least every three years. Palliative care monitoring is voluntary and done through self-assessment.
Only the standards in aged care and palliative care explicitly require an assessment of carer needs. Standards in disability and child protection require service providers to demonstrate how they ‘build carer capacity’ This could include actions similar to those articulated in the standards for the other program areas, such as provision of relevant information or access to relevant supports. However, the variation in standards could result in carers’ experiencing an inconsistent degree of recognition.
3.3.2 Carers’ experience of recognition
Carers experience recognition to varying degrees depending on their age and the diagnosis or condition of the person they care for. A number of carers felt that the quality of recognition was as a result of the work practices of individuals rather than a consistent systemic approach. Themes on recognition from our carer focus groups include:
- Carers in the mental health focus group reported that they felt more recognised in Area Mental Health Services (AMHS) than in Psychiatric Disability Rehabilitation and Support Services (PDRSS). This may be as a result of the greater investment in, and scrutiny of, carer recognition in AMHS than in PDRSS. Some carers also noted the level of recognition had been improving over time.
- Carers in the disability focus group felt service providers do not recognise their needs as individuals. One carer in the disability focus group felt that she experienced a much greater level of recognition from service providers as the carer for her elderly mother than the carer of her son who has a disability.
- Feedback from stakeholders indicates that kinship carers feel taken for granted by the child protection system. Participants in a kinship carer focus group reported inconsistent engagement and advice from DHS staff, citing staff turnover and the resulting lack of continuity as contributing to this.
- Worryingly, young carers participating in our focus group related experiences of hospital staff, teachers and CentreLink workers not believing their descriptions of the care responsibilities they maintain.
3.4 Effectiveness of supports
Carer support programs should have clearly stated objectives, be evidence-based and draw on carer input in their design. To determine whether programs are effectively meeting their objectives, the departments and service providers need to use outcome measures to assess performance, such as before and after indicators of carer wellbeing.
The current suite of carer support programs has developed from a sound evidence base comprising a combination of research, evaluation and carer involvement. However, the extent to which the programs meet their objectives cannot be clearly determined as there is no consistent use of outcome measures.
3.4.1 Evidence base for supports
Research and evaluation
Each program area was able to provide examples of academic research and pilot program testing and evaluation that had informed the development or improvement of carer supports.
The former DHS established many of the current carer support programs in 1996 as a suite of supports known as the Support for Carers Program. The Victorian Government funded academic research to inform the development of this program, which provided the first profile of Victorian carers.
Carer involvement
Departmental practices demonstrate a strong commitment to genuine carer involvement in program development and improvement. Common consultation methods include surveys, focus groups and interviews, with subsequent reports identifying the major themes arising from the consultations. For example:
- Carer focus groups informed the Disability Services division’s development of a set of principles to guide the allocation of funds for ‘Innovative Respite’ programs, newly funded in 2011–12.
- Consultation with kinship carers influenced the design of the Victorian Kinship Care Model.
The ageing and aged care, and mental health program areas in DH, and child protection in DHS also maintain a range of committee and working group structures that include carer membership or representation.
Figure 3C describes a pilot project, supported by the mental health program area, of an innovative service development and improvement model called Mental Health Experience Co-design, or MH ECO. A key feature of the model is the active involvement of carers and consumers. Services involved in the project pilot reported sustainable changes to their services and practices because of their participation in the program.
Figure 3C
Mental Health Experience Co-design project
The MH ECO model is designed to engage carers, consumers and service provider staff in ‘co-designing’ service improvements. Carers, consumers and service provider staff work together to identify areas in need of improvement in their mental health services and develop, implement and monitor a service improvement project. An important element of this approach includes the development of evaluation and project skills, particularly among carers and consumers, to enable the whole team to contribute equally to the project.
The evaluation of the pilot project conducted across two sites, one AMHS and one PDRSS, during 2008–2010 found a high level of support for the model among the project participants. The report concluded that the model was successful in achieving sustainable service and practice changes, such as improved information provision for carers and consumers and support for carers.
Source: Victorian Auditor-General’s Office.
3.4.2 Monitoring and evaluation
A comprehensive performance monitoring framework includes routine monitoring of activity and outcomes combined with regular evaluations addressing the objectives of the program.
Routine monitoring
Departmental monitoring of funded service providers focuses on activity. All program areas collect data relating to activity, for example hours, episodes, applications, and some carer demographic data. However, activity monitoring across programs is inconsistent. For example, respite activity within aged care and disability is measured either by time (hours, days), or episodes of service. This makes it difficult to compare activity levels with funding to assess efficiencies either between service providers or across programs. However from 2012–13 disability services will report respite provision in hours. Figure 3D outlines reporting requirements across a number of carer supports.
Figure 3D
Reporting requirements for carer supports
|
Number of carers |
Hours/ days |
Contacts/episodes |
$ |
Wait time |
Other(a) |
|
|---|---|---|---|---|---|---|
|
Aged care |
||||||
|
Support for Carers Program |
Yes |
Yes (respite) |
No |
Yes |
No |
No |
|
Dementia Carer support(b) |
Yes |
No |
Yes (respite) |
Yes |
No |
Yes |
|
Mental health |
||||||
|
Carer Support Fund |
Yes |
No |
Yes |
Yes |
Yes |
No |
|
Disability |
||||||
|
Respite |
Yes |
No |
Yes |
No |
No |
Yes |
|
Case management |
Yes |
No |
No |
No |
Yes |
No |
|
Kinship |
Yes |
Yes |
Yes |
No |
No |
No |
(a) ‘Other’ includes qualitative reporting, such as case studies or satisfaction surveys.
(b) Dementia carer support is a sub-activity of the Support for Carers Program.
Source: Victorian Auditor-General’s Office.
The ageing and aged care, and palliative care program areas in DH and the Disability Services division in DHS collect some qualitative feedback, either through manual reporting templates or annual surveys. However, this is based on subjective assessments of service providers or service users. Figure 3E provides cases studies of the qualitative monitoring practices in these programs.
Figure 3E
Qualitative monitoring practices
Aged care
Ten aged care Support for Carers Program providers who receive additional program funding to support carers of people with dementia include qualitative case studies on client outcomes in their annual reporting. The reporting proforma requires service providers to comment on the level of carer ‘enjoyment or satisfaction’ in relation to the service provided.
A review of four sample reports showed that carers were satisfied with the supports. However, the service providers based their reports on different feedback channels, including an independent carer satisfaction survey, routine follow-up of carers who have received services or ad hoc personal feedback from individual carers.
The inconsistent amounts and quality of information contained in these reports do not provide a reliable indicator of effectiveness.
Disability
Disability Services conducts an annual carer respite satisfaction survey. The survey includes carer experience indicators to show the impact of respite services for carers.
Results show low carer satisfaction with respite availability, with 50 per cent of carers being ‘satisfied’ in 2011, down two per cent from 2010. The survey authors suggest this is due to limited service availability.
The survey report also includes a ‘carer needs gap analysis’. The results of this analysis indicate that respite does not meet carer expectations of ‘being less fatigued’ and ‘being able to do more things you enjoy’. One of the objectives of respite is to ‘enhance family functioning and maintain positive family and care giving relationships’. The negative effect carer fatigue and discontent would have on family functioning and relationships suggest that respite does not reliably achieve this objective.
Source: Victorian Auditor-General’s Office.
Monitoring outcomes
The departments have demonstrated work on the development of outcome measures for clients receiving mental health or disability services, but none for those receiving carer supports. The ageing and aged care and child protection program areas have not developed any outcome measures. The Disability Services division has conducted a consultation workshop to develop a set of outcome measures for the recently funded ‘innovative respite’ program. The division is proposing to base the measures on the objectives of the program, which include supporting family and care relationships.
The palliative care program advocates the voluntary participation of service providers in the national Palliative Care Outcomes Collective (PCOC) which includes a carer related indicator. Figure 3F provides a case study of PCOC. This model is an example of how a patient-centred monitoring system has incorporated carer outcomes to provide an overall indication of care efficacy and quality.
Figure 3F
Palliative Care Outcomes Collaborative
The Palliative Care Outcomes Collaborative (PCOC) is a nationally funded program that uses standardised and validated clinical assessment tools to benchmark and measure the outcomes of palliative care. Participation is voluntary. Twenty-two of Victoria’s 55 palliative care services participate in the program.
While the primary focus of the model is on the patient receiving palliative care, one of the four measures, termed Palliative Care Problem Severity Scores, includes a rating of carer and/or family physical and emotional needs. Palliative care services recognise that the carer’s ability to cope is an important determinant in enabling a person to die in the place of their choice, which for many people is in their own home.
Services record these problem severity scores as the palliative care patient moves between the different pre-defined phases of care: stable, unstable, deteriorating, terminal and bereaved.
Results from the January to June 2011 report show that rates of carer stress receiving a ‘severe’ score were lower among Victorian in-patient palliative care services compared to the national averages in all phases, and in all phases except the terminal phase in community based services. The authors excluded the bereaved phase from the report.
The overall results suggest that carer supports in Victorian palliative care services are a significant factor in achieving lower rates of carer stress compared to the national average.
Source: Victorian Auditor-General’s Office.
Consultation with 12 funded service providers revealed evidence of only three services, one each in palliative care, mental health and disability, using outcome measures at the service provision level.
The mental health provider uses two standardised tools to monitor carer stress levels before and after accessing counselling or their carer capacity building program. A formal evaluation of the capacity building program found that carer stress levels based on the ‘Involvement Evaluation Questionnaire’ were reduced following their participation in the program. However, the service provider used this tool during the evaluation period only and subsequently discontinued its use.
The disability service provider develops ‘SMART’ goals (Specific, Measurable Attainable, Relevant, Timely) with carers using a tool developed in-house. A service provider staff member and the carer revisit these goals at the end of a period of service provision to see whether the support has helped the carer reach their stated goals.
One-off evaluations
Most program areas have completed one-off evaluations of most of their carer support programs. The exceptions are child protection which commenced a kinship carer support program in 2010, and palliative care. These evaluations provide only limited assurances of program effectiveness as they either did not address the objectives of the program, or appropriate data was not available. A consistent theme identified in these evaluations is the need to develop carer-related outcome measures to determine program effectiveness.
Figure 3G shows that most program evaluations have not addressed the objectives of the program.
Figure 3G
Carer support program objectives and evaluation comparison
|
Program |
Program objectives/aims |
Evaluation objective/focus |
|---|---|---|
|
Support for Carers Program(a) |
Objectives include:
|
One evaluation, 2001:
|
|
Aged care |
||
|
Support for Carers Program |
Objectives include:
|
One evaluation, 2011:
|
|
Mental health |
||
|
Carer support fund |
To meet the needs of carers by:
|
Two evaluations, 2008 and 2011:
|
|
Disability |
||
|
Respite |
Aims of disability respite include:
|
Two reports, 2009 and 2010:
|
(a) The 2001 Support for Carer Program evaluation applied to support programs across ageing and aged care, mental health and disability program areas.
Source: Victorian Auditor-General’s Office.
DH has not evaluated the Psychiatric Disability and Rehabilitation Support Service carer supports, but has recently scheduled evaluations for this service.
Recommendation
- That the Department of Health and the Department of Human Services develop outcome measures for carer supports and monitor outcomes.
Appendix A. Audit Act 1994 section 16—submissions and comments
Introduction
In accordance with section 16(3) of the Audit Act 1994 a copy of this report was provided to the Department of Health and the Department of Human Services with a request for submissions or comments.
The submission and comments provided are not subject to audit nor the evidentiary standards required to reach an audit conclusion. Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows: