Follow up of Access to Public Dental Services in Victoria
Overview
Good oral health is important in its own right, and because of its close link with general health and wellbeing.
Economically and socially disadvantaged Victorians, who are eligible for public dental services, are most likely to experience poor oral health. The Department of Health & Human Services and Dental Health Services Victoria (DHSV) are primarily responsible for preventive oral health care and oral health promotion activities.
In 2016 the Victorian Auditor-General tabled a report Access to Public Dental Services in Victoria, which examined whether public dental services are accessible in a timely manner and whether the agencies effectively facilitate timely access. The report made 11 recommendations to DHHS and DHSV. In this follow up, we assessed whether the two agencies have effectively implemented these recommendations.
Transmittal letter
Independent assurance report to Parliament
Ordered to be published
VICTORIAN GOVERNMENT PRINTER November 2019
PP No 98, Session 2018–19
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of the Audit Act 1994, I transmit my report Access to Public Dental Services in Victoria.
Yours faithfully

Andrew Greaves
Auditor-General
28 November 2019
Acronyms
| BP3 | Budget Paper 3: Service Delivery |
| CBA | cost-benefit analysis |
| CDA | community dental agency |
| DHHS | Department of Health and Human Services |
| DHSV | Dental Health Services Victoria |
| DWAU | Dental Weighted Activity Unit |
| ICHOM | International Consortium for Health Outcomes Measurement |
| ICT | information communications technology |
| KPI | key performance indicator |
| MoC | model of care |
| OHQ | Oral Health Questionnaire |
| RDHM | Royal Dental Hospital of Melbourne |
| SoP | Statement of Priorities |
| VAGO | Victorian Auditor-General's Office |
| VBHC | value-based healthcare |
Audit overview
This report follows up our performance audit Access to Public Dental Services in Victoria, tabled December 2016.
Performance audits focus on the efficiency, economy, effectiveness and legislative compliance of public sector agencies, and include recommendations to improve the management and delivery of public services.
Each year, we ask agencies to attest to their progress in addressing the recommendations that they accepted. Using these attestations―as well as our assessment of the public interest and materiality of audit topics―we selected Access to Public Dental Services in Victoria to follow up.
This audit examined whether the Department of Health and Human Services (DHHS) and Dental Health Services Victoria (DHSV) have effectively implemented the recommendations we made in that audit and addressed the underlying issues that led to them.
Conclusion
DHHS and DHSV agreed to implement our recommendations by December 2020 and have made some progress in driving preventative care. However, there remains more work to be done. This is in part due to the major reform required to shift public dental services' focus from treatment to a more patient-centred model aimed at prevention, early intervention and improving health outcomes. As a result, adult public dental health patients will continue to wait for improvements to the system. Some actions, such as work on the funding model, could have started earlier.
DHSV applied the principles of value-based healthcare (VBHC) to seven new models of care (MoC) that will help deliver the reform needed. Community dental agencies (CDA) co-designed this work. The first MoC has been piloted in a hospital environment, and DHSV acknowledges that the next step is to test it in CDAs to fully understand issues that may impede implementation. DHSV has not analysed the costs and benefits of shifting to the VBHC MoC as part of the piloting process. With no cost-benefit analysis (CBA), it is difficult to assess whether the VBHC MoC will deliver the expected benefits.
DHHS and DHSV reviewed different funding models that could effectively deliver public dental services. Results from commissioned work due in March 2020 should improve their understanding of CDAs' cost structures and the efficiency of these costs. To optimise patient access with available funding, DHHS needs to know how much it costs CDAs to deliver efficient services.
DHHS and DHSV are working to improve access to care through enhanced waiting list management and CDAs are providing more preventive services. However, further testing with CDAs needs to occur before implementing changes. Until this work is completed, CDAs and patients will only realise limited benefits.
DHHS and DHSV completed work to develop oral health outcome measures. An important next step will be to support CDAs to use the indicators developed to collect better health data on patients accessing their services. Only then can DHHS, DHSV and CDAs show whether patient oral health outcomes are improving.
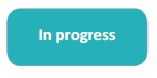
Assessment of actions to address 2016 audit recommendations
Figure A shows our assessment of the actions taken by DHHS and DHSV to address the 2016 audit recommendations. It uses the following key:
|
Recommendation completed |
|
|
Recommendation in progress |
Figure A
Assessment of progress against recommendations
|
A new approach to delivering public dental services (Chapter 2) |
|
|
|
DHHS and DHSV partially accepted this recommendation. As part of its shift to more client-centred and value-based services, DHSV is piloting one of seven new MoCs. It needs to work more closely with CDAs to test the new MoCs in their environment. Piloting of MoCs that focus on adult care are likely to be impacted by DHSV's added responsibility for designing, piloting and implementing a new school dental program. |
|
|
DHSV has not yet completed a CBA. However, in mid-2019 it began a cost analysis of the Royal Dental Hospital of Melbourne's (RDHM) current model and the new VBHC MoC. In a separate project at the RDHM, evidence for the benefits of a VBHC model is being collected as part of piloting the general dental care MoC. |
|
|
DHSV has reviewed a range of alternative funding models and has engaged consultants to examine how its preferred conceptual model would work in practice. |
|
|
DHHS started a quantitative analysis of the need for loadings in July 2019, after the funding model review. This analysis could have started earlier, as it was not dependent on the funding review's findings. |
|
|
A comparative cost analysis of CDAs began in July 2019 and is aiming to identify the efficient cost of public dental services. Implementing consistent pricing is likely to be challenging and will require a phased transition. |
|
Access to care during the transition (Chapter 3) |
|
|
|
Both DHHS and DHSV identified strategies to improve waiting list management. A review of patient eligibility and priority access criteria is complete. The tool DHSV developed following the review is still being validated, and further testing of the Bendigo model is required before scaling up. |
|
|
DHSV identified examples of regional collaboration with CDAs to address access barriers. A more systematic approach is required to help CDAs identify suitable collaborative approaches for piloting/scaling up programs to test their effectiveness in addressing access barriers and improving oral health outcomes. |
|
|
DHHS and DHSV helped CDAs provide more preventive services, including changes to regulations that allow dental assistants to apply fluoride varnish and provide oral cancer screening and prevention packages. A funding model that provides greater incentives for prevention work will help CDAs take advantage of these initiatives. |
|
Measuring and reporting performance (Chapter 4) |
|
|
|
DHHS and DHSV worked with an international consortium to develop oral health outcome measures. An important next step will be to involve CDAs in collecting health outcome data to demonstrate whether access to care has improved oral health outcomes. |
|
DHHS completed a review of the Statement of Priorities (SoP) key performance indicators (KPI) as part of its review of the State Budget Paper 3: Service Delivery (BP3) KPIs. New measures are included in the SoP. Improving the value of this reporting, including outcome measures, will be an important next step to assess the impact of the dental health program. |
|
|
DHHS developed new BP3 KPIs for public dental services and is continuing to review and trial further measures. As yet, DHHS is still working to identify a set of measures that provide a comprehensive picture of dental service delivery. |
Source: VAGO.
Responses to report and recommendations
We have consulted with DHHS and DHSV and considered their views when reaching our audit conclusions. As required by the Audit Act 1994, we gave a draft copy of this report to these agencies and asked for their submissions and comments. We also provided a copy of this report to the Department of Premier and Cabinet.
The full responses are included in Appendix A.
1 Audit context
1.1 Oral health
Good oral health is important in its own right, and because of its close link with general health and wellbeing.
Poor oral health is a significant contributor to the burden of disease in Australia. Oral disease is a key marker of disadvantage, as it is more often experienced by individuals with low socio-economic status.
Although common, most oral disease can be prevented. Notably, a preventive approach to oral health is widely recognised as the most cost-effective approach to improving oral health outcomes.
1.2 Public dental services in Victoria
Who delivers public dental services?
DHHS has overall responsibility for the public dental program and leads negotiation of the National Partnership Agreement on Public Dental Services for Adults with the Australian Government. DHHS funds DHSV, the leading public oral health agency in Victoria, to purchase and deliver public dental services on its behalf. DHSV fulfils this responsibility by providing oral health services through the RDHM and by purchasing dental services for public patients from 52 CDAs across Victoria.
Who is eligible for public dental services?
Access to public dental services is not universal. Eligibility criteria target individuals who are disadvantaged, including children up to the age of 12 and young people and adults with healthcare and pensioner concession cards. Specific population groups recognised as being at higher risk of poor oral health compared with the general population are given priority access, including children and young people, homeless people and Aboriginal and Torres Strait Islander people.
How are public dental services funded and delivered?
Funding model
|
The amount of funding provided to CDAs for a particular service item is determined using the Dental Weighted Activity Unit. This takes into account the complexity and length of time required to complete the service. |
The state government provides the majority of funding for public dental services. The Victorian Dental Health Program has a capped funding model, with current funding levels sufficient to treat only approximately 25 per cent of people eligible for public dental services, based on 2016 data.
The Australian Government has provided additional funding since 2013 through National Partnership Agreements and the Child Dental Benefits Schedule since 2014. However, this funding stream is not certain, as the Australian Government can choose to discontinue them—in the case of the National Partnership Agreement—or legislate to close it—in the case of the Child Dental Benefits Schedule—at any time.
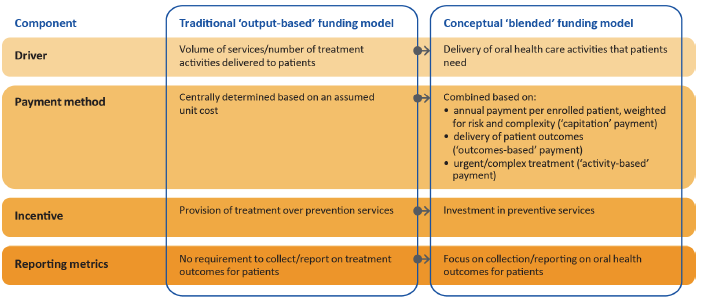
The current 'output-based' funding model, which uses the Dental Weighted Activity Unit (DWAU) to measure activity or output, was in place at the time of our 2016 audit. Limitations of the current funding model include that it does not:
- encourage CDAs to provide preventive activities
- allocate a consistent rate to CDAs for delivery of state-funded activities
- take account of factors that affect CDAs' ability to deliver care, such as their geographical location.
Care model
Currently, eligible individuals can access public dental services through two pathways—routine or general care, and emergency care.
Individuals seeking general care are placed on a waiting list without an assessment of their oral health needs, or their risk of deteriorating oral health while waiting for care. They are advised that if their condition deteriorates, they can seek emergency care. However, around 80 per cent of patients receive care without needing to be placed on a waiting list. Individuals from priority access groups are not placed on a waiting list but are given the next available appointment. Individuals requiring emergency care are assessed and treated in accordance with clinically appropriate time frames.
1.3 Value-based healthcare
Around the time of our 2016 audit, DHSV had begun to explore VBHC as it relates to oral health. VBHC grew out of a body of work on healthcare systems undertaken by the Harvard Business School. Figure 1A represents this approach in terms of a value equation.
Figure 1A
Value equation
Source: DHSV.
VBHC intends to maximise value for patients by focusing on outcomes that matter to them. Patients under a VBHC model will discuss their oral health needs with a clinician and then co-develop a treatment plan.
The principles underpinning VBHC include:
- achieving the best outcomes for patients at the lowest cost
- patient-centred systems organised around what patients need
- the right services provided by the right person, in the right place and at the right time
- integrated care across providers and systems
- measuring outcomes and costs for every patient
- reducing variation in workforce practices and service activity.
DHSV has adapted VBHC principles to oral health, leading to the development of the DHSV VBHC framework as shown in Figure 1B. The framework has nine components, with MoCs comprising two of these. One focuses on individualised interventions and the other on population or setting-based interventions.
Figure 1B
DHSV's VBHC framework
Source: DHSV.
DHSV has embarked on a major reform of public dental service delivery in Victoria through its VBHC framework, with the objective of improving oral health outcomes for eligible patients.
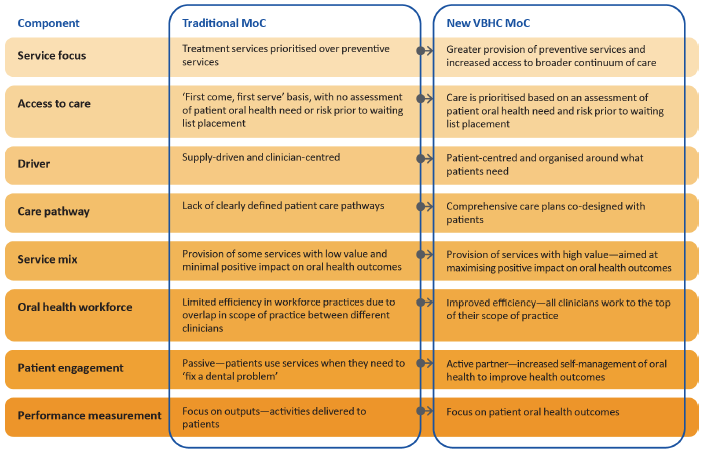
VBHC represents a significant departure from traditional service delivery and is a relatively new approach to healthcare, both in Australia and internationally. Figure 1C compares the key features of traditional public dental service MoCs with the VBHC approach.
Figure 1C
Traditional MoC compared with the VBHC MoC
Source: VAGO.
Moving from principles to implementation
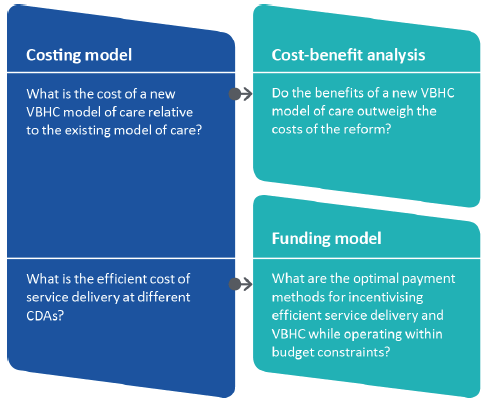
The transition to a VBHC approach to public dental services requires changes to the care model's design. It also requires close examination of the costs and benefits of this new approach and the best way to fund its delivery in the long term. DHSV believes that modelled costs for a VBHC approach will be lower over time.
Each of these components play an important role:
- A costing model will determine the cost of VBHC relative to current service delivery and establish the efficient cost of services.
- A CBA will assess the net benefit of the VBHC reforms. It also helps evaluate the economic merit of alternative options as part of the design process. A CBA uses information on cost of services as a basis for identifying cost savings, or additional resources required to implement VBHC.
- A funding model helps service providers to have sufficient revenue to cover their cost of service, while also incentivising prevention—one of the core principles of VBHC.
Figure 1D shows these components, and how they are interrelated.
Figure 1D
Relationship between costing model, CBA and funding model
Source: VAGO.
Given the strong interdependence between these components, a better practice approach is to progress work on all three in parallel.
1.4 Why this audit is important
Access to public dental services is not universal. People who are eligible for public dental services include vulnerable and socially and economically disadvantaged individuals. Compared with the general population, these individuals:
- have more disease and fewer teeth
- wait longer to get routine care
- are less likely to access services.
Our 2016 Access to Public Dental Services in Victoria audit made 11 recommendations related to care and funding models, aspects of service delivery, and measurement and reporting on performance of service delivery.
DHHS and DHSV partially accepted recommendation 1 and fully accepted all other recommendations, noting funding certainty and availability may constrain their ability to implement some recommendations. In this follow up audit, we assessed how effectively they have addressed the recommendations.
1.5 What this follow up audit examined and how
To determine how effectively DHHS and DHSV addressed the audit recommendations, we considered whether:
- performance issues relating to the recommendations have been addressed
- timely action has been taken to address recommendations
- plans are in place to address incomplete recommendations
- actions are monitored for review and impact.
As part of the audit, we sought to verify the agencies' attestations about their progress in addressing the recommendations, reviewed documents and interviewed staff. We also visited three CDAs.
Unless otherwise indicated, any persons named in this report are not the subject of adverse comment or opinion.
We conducted our audit in accordance with the Audit Act 1994 and ASAE 3500 Performance Engagements. We complied with the independence and other relevant ethical requirements related to assurance engagements. The cost of this audit was $250 000.
1.6 Report structure
The remainder of this report is structured as follows:
- Part 2 looks at the care and funding models for public dental services.
- Part 3 looks at three aspects of service delivery—waiting list management, regional collaboration to address service access barriers, and provision of oral health promotion activities.
- Part 4 looks at measurement and reporting on the performance of public dental services.
2 A new approach to delivering public dental services
Funding models and MoCs are central to how public dental services are delivered. MoCs influence how CDAs deliver services to eligible patients, while funding models and clinical assessment drives the types of services they deliver.
In our 2016 audit, we concluded that the funding model and MoC required fundamental change. We found that CDAs were not able to provide eligible patients with access to a broad range of care services including prevention, promotion, early detection and identification and treatment. This limited their ability to achieve positive oral health outcomes for patients.
While recognising that many public dental patients require both treatment and education, a MoC that focuses predominantly on treatment is demonstrably less cost‑effective than a preventive approach to oral healthcare. We identified the funding model as one of the barriers to DHSV and CDAs adopting a more preventive approach to public dental service delivery. This is because the model rewards outputs, rather than optimal patient outcomes. We found that the funding model did not take into account factors that affect CDAs' cost base to deliver services, such as geographical location and differences in demographics of clients. It also did not fund CDAs at the same rate for the delivery of state‑funded activities.
In this Part, we look at actions taken by DHHS and DHSV to address these issues.
2.1 Conclusion
DHSV responded to recommendation 1 by identifying seven new MoCs based on VBHC principles. Its piloting of the first of these is still in progress. While an evaluation of the initial testing shows positive results, piloting in just a hospital environment rather than at CDAs means there is a risk that implementation in CDAs will be flawed. It is too early to determine the extent to which the new MoC will improve access to care for public dental patients.
DHHS has been slow to start a quantitative analysis of possible systematic differences between CDAs in relation to their cost drivers. It has commissioned work that, if CDAs participate, will provide this data by March 2020. While DHHS has considered mechanisms to address funding inequities between CDAs as part of its review of funding models, it could have begun examining the differences between CDAs independently of that review, speeding up this work.
2.2 Models of care
Our 2016 audit made two recommendations in relation to MoCs. These included developing MoCs that would enable eligible people to access a broader continuum of care, and to determine the costs and benefits of implementing such MoCs.
Identification and piloting of models of care
Recommendation 1
|
|
That the Department of Health and Human Services and Dental Health Services Victoria work with community dental agencies to identify and pilot models of care that redress the current imbalance between treatment and prevention services for eligible people by increasing access to the broader continuum of care, while maintaining the focus on addressing demand for treatment. |
DHHS and DHSV committed to pilot new MoCs by July 2020. It identified seven models, including a general dental care model, all of which will be underpinned by the principles of VBHC. It took a staged approach to co-designing and piloting the MoC prior to implementation.
|
A continuum of care refers to a comprehensive approach to healthcare, involving delivery of a range of services including prevention, promotion, early detection and identification, and treatment. |
DHSV worked closely with the RDHM to pilot the first of its identified MoCs—general dental care—in four dental chairs in the hospital's primary care clinic. DHSV invested significant effort for around 18 months prior to the commencement of a proof of concept, which involves testing all parts of the MoC in a real environment and in real time, to develop the required supporting protocols, processes and tools. The proof of concept began on 1 October 2018. DHSV advise that it finished this on 31 March 2019 and that further testing is continuing based on the results.
A critical next step will be to test the general dental care MoC in CDAs. DHSV has not yet piloted its general dental care MoC using VBHC principles in any of the 52 CDAs that it also funds to deliver public dental services in Victoria. Piloting the new MoC only in the hospital environment limits the ability to both conduct a full assessment of the model's operation and ensure CDAs are engaged in the testing phase.
In August 2019, DHSV completed an evaluation of the general dental care MoC proof of concept at the RDHM. The evaluation compared the MoC with the traditional model of oral healthcare operating in the primary care clinic where equivalent data was available. Over a six-month period, 221 clients accessed the new MoC, with only 28 of the 170 (16.5 per cent) who received general care completing their planned treatment. The data should be interpreted with caution, since it is based on a short period of time and small numbers. Nevertheless, it reflects an uptake of the principles of VBHC. For example, in the MoC cohort:
- A lower percentage of patients (5.9 percent) did not turn up for their treatment appointment compared with patients in the primary care clinic (19.4 per cent).
- Patients received preventive services more often (32.5 per cent) compared with patients in the primary care clinic (21.8 per cent).
- Dentists performed work that could be done by oral health therapists or dental assistants working to the full scope of their practice less often (10per cent) compared with the primary care clinic (47 per cent).
- The response by patients to an introductory session (described in Figure 3A) reflected a commitment to engage with the service. Of the 208 patients with a scheduled introductory session appointment, 168 (80.7 per cent) attended. Just over 95 per cent of these patients started general care or organised a future appointment.
CDAs
Although the general dental care MoC is still being piloted, DHSV advised that a number of CDAs have taken up some of its principles or components within their existing services. This was also evident in our visits to CDAs. Examples include:
- adopting an introductory session as the first point of contact for patients
- maximising clinicians working to the top of their scope of practice within a multidisciplinary team
- upskilling dental assistants to enable them to:
- undertake fluoride varnish applications
- take on the oral health education/coach role and complete oral health promotion and prevention activities for less cost.
As described above, DHSV initially engaged broadly with CDAs to communicate the case for VBHC as the new way of delivering public dental services, and then to co-design the DHSV VBHC framework.
DHSV advised us that it has worked closely with CDAs to identify, encourage and share examples of innovative practice and adoption of VBHC principles. It has done this largely through its annual Public Oral Health Innovations Conference and regional forums. DHSV staff also visit CDAs.
DHSV did not support CDAs to adopt principles and components of the new VBHC approach. Instead CDAs selectively 'opted-in'. The best way to understand the extent to which CDAs have already begun to incorporate components of VBHC into their current services would be to map this activity back to VBHC principles. This analysis would help DHSV ensure ongoing engagement of CDAs and build an evidence base to share learnings with CDAs.
Its engagement with CDAs since the initial stages has not been as effective as it could have been. CDA staff expressed to us uncertainty about the outcomes of the new MoC testing, the plan for implementing it in CDAs, and the status of work to develop a new funding model.
DHSV now has additional responsibility for leading the co-design, piloting and implementation of the new school dental program, though this had not been planned when it began the transition to VBHC.
|
A new school dental program was announced in May 2019 and intends to provide free dental check-ups to Victorian school children in the public system and reach 650 000 children by 2022. |
DHSV considers that the experience of the school dental program will allow it to better understand CDAs' capacity to implement VBHC principles in a MoC for adults. This is because the school dental program is underpinned by VBHC principles and CDAs are involved in its co-design.
DHSV must effectively manage the piloting and implementation of the school dental program, so as to not compromise progress in piloting the general dental care MoC for adults, or in CDA uptake of VBHC principles and MoC components. Equally, implementation of the school dental program during the transition to VBHC will provide DHHS and DHSV with an opportunity to use it as a platform to enhance the success of the VBHC approach for adults. This is because establishing good oral hygiene and behaviours early in life sets the foundation for good oral health outcomes in later years.
Cost-benefit analysis of models of care
Recommendation 2
|
|
That the Department of Health and Human Services and Dental Health Services Victoria work with community dental agencies to carry out a cost-benefit analysis of the long-term outcomes of adopting a model of care for public dental services. |
Costs
DHHS and DHSV have not yet completed a CBA of the VBHC MoC. DHHS committed to complete this work by December 2020.
|
Time-driven activity‑based costing is a methodology that calculates the total cost of services as a patient progresses through a care pathway. |
DHSV has engaged consultants to develop a cost model that will enable it to estimate the cost of new care pathways and compare it to traditional service delivery. Time-driven activity-based costing is being used as a means of establishing the cost of delivering services.
Until the end of July 2019, DHSV had not yet developed an estimate of costs for the new MoC pathways. DHSV advised us that in October 2019 it reported to its finance committee on the methodology and initial analysis supporting the development of the costing and funding model for the new MoC. Further analysis is to be carried out to inform the specification of the proposed model, the results of which will be reported to its board in November 2019.
The cost modelling is based on the MoC for general dental care at the RDHM, and therefore may not be representative of the costs at CDAs. DHSV advised us that it is starting this work at the RDHM because data is readily available. CDAs are separate entities that would need to consent to provide cost data. This means that DHSV does not have easy access to CDAs' cost data for treating patients and performing particular activities.
The cost modelling work is independent of the general dental care MoC proof of concept, which is also being undertaken at the RDHM. The cost of new VBHC pathways is not part of testing the operation of the MoC. This is a lost opportunity. Had cost analysis been incorporated into the proof of concept, it would have provided DHSV with evidence about the indicative cost of the new MoC. This could then have informed the CBA and would potentially help to identify those features of the new MoC that are most cost-effective.
Benefits
DHSV advised us that it has not attempted to quantify the potential monetary benefits of a transition to a VBHC approach, or how these benefits compare to the cost of implementing this approach. This is because it is confident, based on a body of health research evidence, that the benefits of such an approach outweigh the cost.
While the research evidence may be compelling, completing a high-level CBA of DHSV's proposed VBHC approach by December 2020, as agreed in 2016, will build further confidence about the case for reform. It may also highlight the key variables that are most influential for attaining the potential benefits.
2.3 Funding model
Our 2016 audit made three recommendations in relation to the existing funding model for public dental services. These concerned the development of a new model that would enable the government to improve oral health outcomes, including loadings in the model to address existing funding inequities, and implementing a consistent rate for activities across CDAs.
Review of funding model
Recommendation 7
|
|
That the Department of Health and Human Services, in consultation with Dental Health Services Victoria, review the most appropriate and effective funding model to deliver public dental services to achieve the government's goals—this will include an assessment of the value of applying the Commonwealth funding model. |
Action on this recommendation is in progress. DHHS and DHSV commissioned two studies to identify an appropriate and effective funding model to support a MoC based on VBHC principles. This helps to incentivise improved patient outcomes and prevention over treatment they examined a number of alternative models, including the option of retaining the existing 'fee for service' Commonwealth funding model. These studies have been rigorous and comprehensive, and examined international experience with funding models for public dental services and healthcare.
|
Capitation is a type of funding model where annual fees are paid to healthcare providers for each patient enrolled in their service. |
DHHS and DHSV identified a 'blended' funding model as the preferred conceptual model and have provided this to consultants to further develop. It has three components:
- a risk-adjusted, 'packaged' payment per enrolled client over a fixed term (also referred to as a 'capitation' payment)
- payments based on outcomes delivered
- retention of activity-based funding for low-volume, complex care.
Figure 2A summarises the key differences between this model and the current output-based funding model.
Figure 2A
Comparison of output-based and blended funding models
Source: VAGO.
The blended model is now at a conceptual stage. DHHS expects that it will be at least three years before the model is operational. There are many practical implementation issues that need to be resolved.
One of the two studies, led by DHSV, is using the RDHM to examine development and design aspects. This project began in March 2019 and the results are scheduled to be reported to the DHSV board in November 2019.
DHHS leads the other project, called Public Dental and Community Health Services Funding Model Redesign. In July 2019, DHHS engaged consultants to identify parameters, principles and the scope of pricing models, develop options for funding/pricing models and to analyse how this could work in practice within a CDA. The project will recommend a preferred design. This project is due to be completed in March 2020.
DHHS and DHSV have kept CDAs informed about a proposed shift to a MoC based on VBHC principles, which is to be accompanied by a change in funding arrangements. In April 2018 consultants for DHSV completed a discussion paper on the proposed funding model changes, with the intention of seeking feedback from CDAs. DHSV advised us that it subsequently decided not to publicly release this document because 'things have moved on'. This means that CDAs have not been involved in the review of alternative funding models or had any role in selecting a blended model as the preferred option.
As the design of the new funding model progresses, DHHS and DHSV should, through the consultants, engage constructively with CDAs to ensure the design process accounts for practical issues. This will also support development of a better model and greater CDA engagement when introducing the new funding arrangements.
Consideration of loadings in the funding model
Recommendation 8
|
|
That the Department of Health and Human Services, in consultation with Dental Health Services Victoria, when developing the funding model, consider including loading for variables that affect how services are delivered, such as remoteness and client complexity. |
As part of the review of funding models, DHHS and DHSV considered how different models address potential funding inequities between CDAs due to differences in patient populations or degree of remoteness. This action only partly meets the requirements of our recommendation. In the absence of a quantitative analysis of CDA costs, it is not possible to draw conclusions about the extent of inequity and whether loadings are needed in allocating funding.
Funding model capable of addressing inequities
The preferred conceptual funding model that DHHS and DHSV have provided to consultants to work on is capable of addressing potential inequities in funding across CDAs. This is because the capitation payment being considered by DHSV is a risk-weighted payment, in which higher payments are made to CDAs enrolling patients with poorer pre‑existing health or at a higher risk of developing serious health conditions.
DHSV advised us that it will be at least three years before a system of risk‑weighted capitation payments are introduced. This is because DHHS is taking a staged approach to reforming funding arrangements instead of a single‑step shift to a blended funding model. In the interim, DHHS is considering whether it should modify the existing fee for service model by applying loadings to the DWAU payment rates.
|
The amount of funding for a particular dental activity is determined using the DWAU of that activity. Funding for each CDA is capped, with each CDA required to deliver a specified agreed activity level. |
Quantitative analysis of the need for loadings
In May 2018, DHHS committed to investigating the need for a new funding formula for allocating global dental health budgets based on population need, complexity and demand.
In July 2019, DHHS engaged consultants to develop recommendations for DWAU loadings, where appropriate, and how they should apply to particular CDAs to take account of contextual factors. Based on our review of available documentation, the methodology used to assess the need for loadings, and what the weighting factors should be, is sound. This work is not due to be completed until March 2020.
While commencement of this quantitative analysis is a positive step, DHHS could have started this work earlier and initiated it independently of its review of funding models.
A consistent unit price for public dental services
Recommendation 9
|
|
That the Department of Health and Human Services, in consultation with Dental Health Services Victoria, develop an implementation plan for introducing a consistent Dental Weighted Activity Unit rate for all community dental agencies while the Dental Weighted Activity Unit funding model is in place, informed by a sound analysis of reliable data. |
DHHS agrees with the principle of setting a consistent DWAU rate for all CDAs. However, it has not yet committed to a date to do this, nor does it have a planned pathway to transition to a single rate. Further work is therefore required to address this recommendation.
Action to address this recommendation has been slow. On 1 July 2017, DHHS introduced a minimum price of $410 per DWAU for all CDAs. It did not engage consultants to begin work on identifying an appropriate consistent DWAU rate that would apply to all CDAs until July 2019. This work is part of the Public Dental and Community Health Services Funding Model Redesign project.
The methodology being used to develop a recommended consistent DWAU rate is sound. This work will also involve cost benchmarking and an efficiency review of CDAs, which will identify an efficient price for dental services. This project is due to be completed by March 2020.
Implementation issues
DHHS advised that implementing a consistent price is likely to present challenges. This is because some CDAs are likely to be financially disadvantaged due to the consistent DWAU rate being lower than what they currently receive. Other CDAs, however, may benefit from a rate increase. Promoting funding reform to those CDAs that may lose funding will be difficult.
DHHS also expressed concern that the shift to a consistent rate will put pressure on its constrained budget. This is because the additional funding required to lift some CDAs to a higher DWAU rate may exceed the funding made available through reduced payments to CDAs that are being paid above the identified consistent rate.
In addition, DHHS advised us that the introduction of a consistent DWAU rate will be dependent on the funding it receives from the Australian Government. A reduction may result in a shortfall in funding to meet current service targets. Nevertheless, this does not weaken the case for identifying the efficient cost of service delivery as a matter of priority. If Commonwealth funding is reduced, DHHS will need to reassess what services can be procured from CDAs with the funds available and the efficient price.
3 Access to care during the transition
While work progresses on the development of new funding models and MoCs for public dental services, it is important that eligible patients can continue to access services and receive the treatment they require.
Our 2016 audit identified some issues with eligible patients not accessing public dental services.
One concerned the way in which CDAs managed their waiting lists. This included placing patients on a waiting list at the time of service entry, with no assessment of their oral health need or risk of deterioration while waiting for care.
We also found that DHSV's collaborative initiatives with CDAs did not effectively address access barriers. Further, we found that CDAs had limited ability to provide a broad continuum of care, including oral health promotion activities.
In this Part, we look at these three aspects of service delivery.
3.1 Conclusion
DHHS and DHSV identified a number of improvements to waiting list management in response to recommendation 3. However, when DHSV piloted improvements made at Bendigo Health (Figure 3A) in other CDAs it found that further work is needed before implementation in all CDAs. DHHS and DHSV also developed a draft action plan to prevent oral disease, which includes developing oral health promotion packages and screening and prevention programs, and workforce regulatory changes. As a result of some of these actions, waiting time for treatment has improved for patients in some CDAs. However, CDAs remain limited in their ability to provide patients with preventative care while the treatment-focused funding model remains in place.
3.2 Delivering services
Our 2016 audit made three recommendations concerning aspects of CDA operations impacting on the delivery of public dental services. These were:
- improving waiting list management, such as through assessment of patient oral health need and risk
- enhancing regional collaboration to address access barriers
- increasing the provision of oral health promotion activities.
Waiting list management
Recommendation 3
|
|
That the Department of Health and Human Services and Dental Health Services Victoria work with community dental agencies to review and improve the current approach to managing waiting lists, including prioritising need and assessing the risk of people placed on the waiting list. |
Review of eligibility and priority access criteria
In response to this recommendation, DHHS, in consultation with DHSV, reviewed the eligibility and priority access criteria for the public dental program. This review recommended a number of changes to the criteria for eligibility and priority access for dental treatment at all CDAs including for all Aboriginal and Torres Strait Islander people (regardless of concession card status) and people experiencing family violence. These recommendations reflect current practice at the RDHM, but not in CDAs. DHHS advises that these policy changes are currently being considered.
Waiting list management policy
DHSV identified issues concerning the operation of waiting lists for public dental services, including that:
- the current waiting list policy and model is outdated
- the clinical need of patients is unknown at the time of entry to service
- no preventive interventions are provided to clients either at the time of placement on a waiting list or while waiting.
DHSV developed recommendations aimed at improving waiting list management. These recommendations align with DHSV's VBHC framework, and include:
- revising waiting list principles (for example, including an oral health assessment and measuring health outcomes)
- changing the waiting list policy (for example, basing it on patient outcomes)
- incorporating preventive interventions at the time of placement on a waiting list and while waiting for care
- improving tools (for example, developing a health assessment tool to prioritise care based on risk determination)
- increasing use of a skilled workforce, with staff working to the full scope of their practice.
Review of best-practice models
In 2017, DHSV undertook two desktop reviews aimed at identifying examples of best-practice waiting list models. One of these included a review of waiting list approaches used in other jurisdictions. This identified a number of features aligned with VBHC principles, such as assessing a patient's oral health prior to placing them on a waiting list.
The other review looked at successful strategies already used by CDAs that targeted patients at the tail end of their waiting lists. This identified one CDA, Bendigo Health, that operates an 'introductory session' for general dental care patients that is also aligned to VBHC principles, as described in Figure 3A. DHSV have incorporated the introductory session into its new general dental care MoC.
Figure 3A
Case study: Bendigo Health's introductory session for general care patients
|
A review by Bendigo Health CDA of its general care waiting list indicated that a proportion of patients on the waiting list were not engaged or not ready to engage with the service. It saw education of these patients as important. This provided the impetus for developing an introductory session for all general care patients prior to beginning treatment. The Bendigo Health model, first implemented in early 2016, consists of an introductory session for all general care patients before treatment begins. Around 20 to 30 people at a time who were at the top of the general care waiting list received a letter inviting them to a group-based introductory session, which ran for around 20 minutes. Patients are provided with information about the service, their rights and responsibilities, care pathways and oral health and hygiene education, such as on teeth brushing and diet. Following the information session, clients make an informed decision about whether to choose the 'general' or 'emergency only' care pathway. Clients who choose the 'general' care pathway receive the next available dental appointment. Clients who choose the 'emergency only' care pathway receive clinic details for when they have urgent dental needs. Key successes of the model include:
The delivery of introductory sessions has changed as a result of regular review and consumer and staff feedback. The model has continued to be sustainable, with an average general waiting time of 10 months at the end of December 2017, and a further decrease to five months by the end of June 2019. |
Source: VAGO.
DHSV worked with Bendigo Health to broaden the implementation of its model to other CDAs. Initially, this involved promoting the model to other CDAs through presentations at annual regional forums in 2017 and 2018.
DHSV advised that it is aware of a number of CDAs that have now incorporated an introductory session into their existing services.
During our visit to one CDA, we observed an introductory session. This CDA reviewed the 17 introductory sessions it delivered between November 2018 and July 2019. Of the 414 patients at the top of the waiting list who received invitations to an introductory session, 55 per cent took up the offer. Nearly all (98 per cent) of these patients opted to start a general course of care, reflecting a commitment to improve their oral health.
Patients' self-reported service literacy and oral health literacy also consistently improved, from 'basic knowledge' before the session to 'confident' after the session. Additional verbal feedback from participating patients includes reports of being more informed and educated about their healthcare options and having a better understanding of good oral hygiene habits (such as correct brushing and flossing techniques).
DHSV waiting list initiative
In February 2018, DHSV began work on a project to further develop and implement the Bendigo Health model with CDAs who have long waiting lists. It plans to eventually rollout this model statewide, making it standard operational practice for all CDAs.
In May 2018, the state government announced an additional $12.1 million in funding in part to help reduce dental waiting lists across the state. Of this, it allocated $5 million to target people on the tail end of CDA general care waiting lists, using the Bendigo Health model. DHSV state that they reviewed waiting lists to identify patients waiting longer than 23 months, which was the SoP target for 30 June 2018. On this basis, DHSV offered 25 CDAs funding to take part in this initiative. CDAs had to implement the Bendigo Health model by the end of September 2018, with all offers of care made by the end of December 2018.
A review of the DHSV initiative shows considerable variability across the 25 CDAs. Some of this is due to differences in the size of CDAs. Variances included the:
- number of patients on the waiting list at start of the initiative (from 883 to 13 307)
- number of patients removed from the waiting list (28 to 4 479)
- reduction in longest waiting time (two to 41 months)
- percentage of patients who took up offer of care (12 to 54 per cent)
- number of patients treated (nine to 1 947).
This initiative enabled CDAs to offer care to a total of 28 146 patients. This represents 26 per cent of the patients who were on the general waiting list of the 25 participating CDAs at the start of the initiative. However, only 10 484 (38 per cent) of these patients took up the offer and received treatment. DHSV acknowledges that this result is lower than expected given the demonstrated success of the Bendigo Health model.
DHSV advised that this could be because the initiative targeted patients who had been waiting the longest. As such, these patients may no longer be contactable, or may have already received some form of care during their wait. DHSV's agency relationships team is working with CDAs to implement the introductory session model, as it considers it to be capable of achieving sustainable waiting list management. To achieve this, DHSV needs to identify and address the barriers that limited the success of the pilot of Bendigo Health's introductory session model.
Assessment of patient oral health need and risk
A key component of the new MoC based on VBHC principles is a risk and need assessment of all new patients, the results of which inform a patient's care pathway. DHSV initially developed a rapid assessment tool to enable this assessment. Testing of this tool as part of the general dental care proof of concept at RDHM identified the need for modifications. This subsequently resulted in the development of the Oral Health Questionnaire (OHQ) in early 2019. The OHQ captures the medical, dental and social history of the patient as well as a set of patient‑reported outcome measures that cover aspects of their oral hygiene and habits. As discussed in Section 4.2, the OHQ has progressed through DHSV's collaboration with the International Consortium for Health Outcomes Measurement (ICHOM) working group. Once the standard set of measures are public, the measures will undergo validation testing. When this is complete and the OHQ is available to CDAs, DHSV can determine the extent to which the OHQ helps improve their waiting list management.
Regional collaboration between CDAs
Recommendation 4
|
|
That the Department of Health and Human Services and Dental Health Services Victoria work with community dental agencies to identify where collaboration between regional public dental services could address barriers to access and pilot related projects to test their effectiveness in improving oral health and in identifying resourcing requirements. |
DHSV advised us that it established and continues to promote mechanisms to communicate innovative initiatives and practices by CDAs. These include its annual regional and metropolitan CDA forums, and the Public Oral Health Innovations Conference.
In March 2019, DHSV prepared a high-level summary of examples of collaborative initiatives by CDAs aimed at addressing access barriers. Many of these included presentations at annual regional forums between 2016 and 2019. Examples include:
- West Wimmera Health Service extending its service reach beyond the catchment region to support local communities, including sharing a mobile dental clinic with Wimmera Health Care Group
- Link Health and Community providing oral health services for residential aged-care residents within their facilities, as part of the Graceful Smiles project
- Sunbury Community Health Service working with Hepburn Health Service to undertake fluoride varnish applications at kindergartens in partly and non‑fluoridated areas participating in the Smiles 4 Miles program within the Macedon electorate.
DHSV has not actively worked with CDAs to identify potential collaboration opportunities. It also does not regularly review collaborative activities to identify and disseminate key learnings and using these to identify suitable collaborative models for piloting or scaling up.
During our visits to CDAs, we identified examples of collaborations that address access barriers and saw how greater DHSV engagement would be valuable for CDAs. One CDA has worked with a community health service, the regional city council and a multicultural council to meet demand for oral healthcare among its refugee community—a priority access group. This collaboration resulted in the co-design of a culturally appropriate and safe refugee clinic, including on-site interpreters. This model is now an integral part of the CDA's service provision.
Another CDA we visited had collaborated with two smaller CDAs in the region to address access barriers due to their relatively isolated communities, and limited access to local dental services and public transport:
- From October 2017 to June 2018, it provided a CDA with an oral health screening (by a dentist and dental assistant) and a prosthetist visiting the service on alternative weeks. The screening service focused on a limited exam, with strong emphasis on oral health instruction and preventive education. The prosthetist serviced targeted people who had partial dentures.
- From March to December 2018, it assisted another CDA with an extended waiting list by providing direct clinical care, which involved sending two oral health therapists twice a week.
Geographical barriers to service access
DHSV itself has developed initiatives and worked collaboratively with organisations to address barriers to service access in regional Victoria. Two key examples include the Royal Flying Doctor Service and teledentistry.
The Flying Doctor Dental Clinic
In 2016, DHSV signed a collaborative partnership agreement with the Royal Flying Doctor Service Victoria and the Australian Dental Association Victorian Branch to establish the Mobile Dental Care Program (known as the Flying Doctor Dental Clinic). The program aims to provide a sustainable mobile model of oral health education, screening and treatment for people living in rural communities with limited access to public oral health services.
Key findings from stakeholder feedback as part of an evaluation of the program during 2017–18 included that the:
- main strengths of the program were the travel time saved by patients through being able to access a local dental service, the high quality of the service, and the competency of program staff
- ability to access the program had increased patients' understanding of how to manage their own oral health and improved their health and wellbeing.
Teledentistry
In January 2015, DHHS allocated $369 000 to DHSV for a telehealth program to allow patients to receive specialist advice and advanced care through a clinical alliance between dentists at CDAs and the RDHM. The program focuses on removing barriers to service access for individuals in remote or at‑risk communities and improving health outcomes.
The results of an initial pilot of the program during 2015–16 at four CDAs were positive. Identified program benefits included creation of a patient-centred MoC, and an ability to treat patients near their home and provide more integrated care. These results have informed the progressive rollout of the program across the state. As at 2017–18, 36 CDAs had participated in this program, most of which are located in rural areas.
Oral health promotion
Recommendation 5
|
|
That the Department of Health and Human Services and Dental Health Services Victoria work with community dental agencies to identify how community dental agencies can take greater responsibility for promoting oral health, supported by adequate funding. |
Draft action plan to prevent oral disease
DHHS and DHSV collaborated to develop a draft action plan to prevent oral disease (the draft action plan). The draft action plan has four objectives, including that Victorians:
- benefit from settings and environments that support good oral health
- have knowledge, skills and resources to improve their oral health
- have access to oral health promotion programs, screening, early detection and preventive services
- have improved oral health through policies and practices based on enhanced data and research.
In developing the draft action plan, DHHS and DHSV conducted extensive consultations during 2017–18 through public regional forums, round table discussions and online submissions. They received feedback from over 500 people and key stakeholders, including consumers, oral health staff from CDAs, and representatives from the health, early childhood, education, social services and local government sectors.
The Victorian Oral Health Promotion Advisory Group (formerly the DHSV Population Health Committee) is responsible for oversight and implementation of the draft action plan, as well as development of a four-year work plan.
Our 2016 audit identified a number of barriers to CDAs taking on more responsibility for oral health promotion. Examples include a workforce that is not equipped to deliver oral health promotion activities, and a lack of coordination between oral health and general health services. The draft action plan addresses some of these barriers:
- Improving oral health literacy will involve initiatives such as the creation of a new workforce of dental assistants with Certificate IV qualifications to assist consumers to manage their own oral health.
- Oral health promotion programs such as screening, early detection and preventive services will enhance the skills of health, early childhood and social service workers and strengthen referral pathways to oral health professionals.
- Creating settings and environments will support good oral health and involve partnering with organisations working with at-risk groups, such as aged-care facilities, diabetes educators and maternity services.
Oral health promotion activities by CDAs
All three CDAs that we visited engaged in oral health promotion activities, including established programs such as Smiles 4 Miles. This program, based in early childhood settings, focuses on promoting good oral health habits and healthy eating, as well as increasing access to dental services. CDAs provide a range of other oral health promotion, education and screening services to organisations and groups in different settings. Many of these are undertaken on an outreach basis. Examples include:
- working with other health professionals/services (such as dieticians, hospital emergency departments, mental health recovery hubs)
- operating a stall at local supermarkets
- working with a special-needs dentist at a school for students with intellectual disabilities
- Aboriginal cooperatives
- humanitarian settlement programs
- young mothers' groups
- agricultural field days/sheep and wool days
- aged-care facilities
- housing crisis services
- local council immunisation sessions and maternal and child health staff.
Oral health workforce regulatory changes
Under the Drugs, Poisons and Controlled Substances Regulations 2017, fluoride varnish is a schedule 4 poison, which can only be applied by registered dental practitioners (dentists, dental therapists, dental hygienists and oral health therapists). DHSV contributed to amending these regulations, and the Drugs, Poisons and Controlled Substances Amendment (Dental Assistant) Regulations 2018 now allows dental assistants to administer fluoride varnish as registered oral health professionals.
Monitoring the impact of this regulatory change will help DHSV understand the extent to which it helps CDAs take greater responsibility for promoting oral health.
Development of oral health prevention tools
Fluoride varnish programs
DHSV worked with a number of CDAs during 2017–19 to pilot fluoride varnish preventive programs and provide oral health screening among preschool and school-aged children. These include:
- Latrobe Community Health Service
- Sunbury Community Health and Hepburn Health Service
- Bendigo and District Aboriginal Co-operative.
The results of completed pilots show good participation by children in screening and fluoride varnish application, and the ability to engage with families to promote important oral health messages. However, these pilots are too short to demonstrate improved oral health outcomes. The workforce regulatory changes discussed below should facilitate improvements to the sustainability of fluoride varnish application.
Oral health prevention packages
DHSV developed content for a number of oral health prevention packages in partnership with other organisations, including:
- a website ('Supporting Every Smile') that provides information for support workers and service users to promote good oral health in disability services
- a smoking cessation program ('Smokefree Smiles') that helps oral health professionals provide brief interventions about smoking with patients and facilitates referrals to Quit Victoria's Quitline
- an online aged-care oral health package to support managing the oral health of older people and aged-care residents.
Monitoring the uptake and effectiveness of these prevention packages will help DHSV understand the extent to which they improve the oral health of the target groups.
Oral cancer screening and prevention program
Funded by DHHS under the Victorian Cancer Plan 2016–20, the oral cancer screening and prevention program aims to help reduce the impact of oral cancer on Victorians. DHSV leads the program in partnership with DHHS, Melbourne Dental School, the Australian Dental Association Victorian Branch and La Trobe University Department of Dentistry.
Piloting of the program, including training for oral health professionals to detect early signs of oral cancer, is happening in 15 sites across Victoria. This will inform the planned rollout of the program to all Victorian oral health professionals.
4 Measuring and reporting performance
Collecting appropriate data on public dental service patients is critical for monitoring and reporting on whether services are improving oral health outcomes.
Our 2016 audit found that DHSV collected limited data about the clinical oral health of eligible adults on entry to services. It does not collect this data when care had been completed, or when a patient returns to the service to determine whether their oral health has improved.
DHSV's SoP reports dental health program KPIs, against which DHSV and CDAs are held accountable. Our 2016 audit found that none of these indicators showed whether access to care had improved oral health outcomes. In addition, reporting by DHHS on the dental health program through the BP3 was output‑focused. This meant it did not provide information on the outcomes of service provision. We concluded that neither DHHS or DHSV provide a comprehensive picture of program impact in their reporting on public dental services.
In this Part, we look at current measurement and public reporting on the performance of public dental services.
4.1 Conclusion
DHSV have developed oral health outcome indicators with an international consortium, but they are not yet implemented. If adopted, these outcome measures will enable reporting about the extent to which access to care improves oral health. DHHS updated both the SoP and BP3 measures and while they are an improvement, they do not yet provide a comprehensive picture of the impact of programs.
4.2 Measuring performance
Our 2016 audit made one recommendation in relation to oral health data on people who are eligible for public dental services. This concerned a lack of data to enable assessment of whether access to care has improved oral health outcomes.
Collect data on eligible patients
Recommendation 6
|
|
That the Department of Health and Human Services and Dental Health Services Victoria work with community dental agencies to collect data on people who are eligible for public dental services as a subset of its broader oral health outcomes measures based on the whole population. |
DHHS and DHSV have focused their efforts on participating in two population‑based surveys:
- The annual Victorian Population Health Survey (based on a random sample of 7 500 adults) added three oral health questions to the 2016 and 2017 surveys—self-reported dental health, when they last visited a dental health professional, and whether cost had an impact on this.
- The Victorian component of the National Study of Adult Oral Health (based on a random sample of adults), which was most recently conducted in 2016–18, has only been conducted twice before (1987–88 and 2004–06). It comprises a telephone survey and oral epidemiological examinations. Of the national sample of 10 220 adults, DHSV managed oral examinations of 1 421 Victorians, which were conducted in CDAs.
These population surveys do not target individuals who are eligible for public dental services—they provide information about the pattern of oral disease and use of dental services in the general adult population.
Data collection by CDAs
The DHSV dental health program dataset defines the data that CDAs are required to record for patients accessing their services. Data on patient clinical oral status includes the number of decayed, missing and filled teeth, and a rating of prosthetic status. CDAs are not required to collect data on returning patients, such as whether they have less tooth decay or improved oral health.
In future, it will be important that DHHS and DHSV enable CDAs to collect relevant data from patients pre and post access to services. CDAs will need support and resources to put the required processes and systems in place to collect the data. This data will provide an assessment of whether the oral health of patients accessing public dental services has improved.
In two of the CDAs we visited, we observed that they had begun to collect some patient self-reported data on the impact of some of its services and activities. This includes pre and post assessment of patient-reported levels of service and oral health literacy, as well as oral hygiene habits and health behaviours. This information is used to inform ongoing improvement of service provision. We do not know the extent to which other CDAs across the state have adopted such practices.
International Consortium for Health Outcomes Measurement
In our 2016 audit, we reported that DHSV had begun work on developing oral health outcome indicators through its participation in the ICHOM oral health working group. This group was established to develop an internationally agreed standard set of oral health outcome measures.
Since 2016, this work has continued to progress. The ICHOM working group identified 23 key outcome measures to include in an adult oral health standard set. DHSV is leading the implementation of the ICHOM standard set consumer validation survey in Australia. Based on feedback from clinicians, work is now underway to determine the most important questions in the adult oral health standard set to develop a shorter set.
While the ICHOM adult oral health standard set has not yet been released, DHSV plans to incorporate its use as part of its transition to MoC based on VBHC principles.
Oral health data management
DHSV recognises the need to improve its information and communications technology (ICT) platform to support data collection to monitor and track the experiences and oral health outcomes for each patient.
DHSV's Digital Strategy 2018–21 sets out its plan to put in place the required ICT platform to help enable its transition to VBHC.
In June 2019, consultants completed a business case for a solution to improve DHSV's oral health record management. The preferred option is to adopt a statewide electronic oral health record that has the capacity to both analyse and report and track patient experience.
The business case sets out a program of work scheduled to begin in January 2020 and finish by February 2022. DHSV advised that the business case is yet to be presented to its board.
4.3 Reporting performance
Our 2016 audit made two recommendations in relation to reporting on the performance of public dental services. These concerned the usefulness, relevance and appropriateness of KPIs in the BP3 and in DHSV's SoP.
Statement of Priorities
Recommendation 10
|
|
That the Department of Health and Human Services, in consultation with Dental Health Services Victoria, review the relevance and appropriateness of current key performance indicators in the Statement of Priorities and identify more relevant indicators for providing a comprehensive picture of the impact of the dental health program. |
The SoP is a document signed by DHSV and the Minister for Health that holds DHSV accountable for achieving KPIs for the dental program and targets set by the government in the financial year.
DHHS did a review of the SoP KPIs as part of its review of KPIs in the 2017–18 Budget Papers. This identified two new performance measures, both of which are included in the 2018–19 SoP. This review is discussed further below.
The 12 KPIs in the 2018–19 SoP that focus on access and timeliness of care include measures related to treatment of emergency triage patients, recall interval and waiting times for general and denture care, and numbers of patients treated. The 2018–19 SoP does not include any performance indicators for improved oral health outcomes.
Given DHSV's transition to a VBHC approach, and its work with ICHOM to develop a standard set of oral health outcome measures, it should consider including appropriate outcome performance measures in its SoP. This will help improve the comprehensiveness of its reporting on the impact of the dental health program.
State Budget Paper 3
Recommendation 11
|
|
That the Department of Health and Human Services, in consultation with Dental Health Services Victoria, review the usefulness of the current key performance indicators in the State Budget Paper 3: Service Delivery and identify more relevant indicators for providing a comprehensive picture of how public dental services are delivered. |
The BP3 KPIs include the actual and targeted annual performance of the dental health program against specified activity-based measures.
Following our 2016 audit, DHHS undertook two reviews of the dental health program performance measures, one of which was externally commissioned, followed by an internal review. These reviews informed changes to the 2017–18 BP3 measures, including:
- discontinuing the measure 'ratio of emergency to general courses of dental care', because it does not show whether emergency care has been timely, as reported in our 2016 audit
- adding a replacement measure, 'percentage of dental emergency triage category 1 clients treated within 24 hours'. While this measure only includes one of three categories of emergency patients, it is the most important performance measure as it represents the most urgent need
- adding a new measure, 'number of priority and emergency clients treated', which shows the extent to which public dental services are achieving the policy intent of treating priority patients. DHHS considers that this helps improve the comprehensiveness of reporting on public dental service delivery.
The 2019–20 BP3 measures also include the 'number of children participating in the Smiles 4 Miles oral health promotion program'. This measure increases the profile of oral disease prevention activity by CDAs. It is also aligned with the new VBHC approach to public dental health service delivery.
Compared with earlier reporting periods, the current BP3 measures have a greater focus on the timeliness of public dental service for the most urgent emergency patients and the extent of service delivery to priority groups. This enhances the usefulness of the suite of KPIs. However, as reported in our 2016 audit, the current BP3 measures still do not provide a comprehensive picture of public dental service delivery because there are no indicators that enable an assessment of how well services objectives have been met. We note that DHHS is continuing to review and trial further measures.
Appendix A. Submissions and comments
We have consulted with DHHS and DHSV and we considered their views when reaching our audit conclusions. As required by the Audit Act 1994, we gave a draft copy of this report, or relevant extracts, to those agencies and asked for their submissions and comments.
Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
- DHHS
- DHSV
RESPONSE provided by Deputy Secretary, Health and Wellbeing, DHHS
RESPONSE provided by the Chief Executive Officer, DHSV