Occupational Violence Against Healthcare Workers
Overview
This audit assessed whether the Department of Health and Human Services (DHHS), WorkSafe, Ambulance Victoria (AV) and health services are adequately protecting healthcare workers from the risks and incidence of occupational violence.
All audited agencies have implemented improvements aimed at preventing and reducing occupational violence. However, these improvements are incomplete, inconsistently applied and have not been evaluated to determine effectiveness. We found systemic failures in relation to collecting, analysing, investigating and reporting quality data on occupational violence incidents for the purposes of improvement.
While DHHS has developed an occupational violence policy to guide health services, it has not fulfilled key responsibilities outlined in its policy or monitored whether health services are even using it. DHHS has implemented other initiatives but not assessed their effectiveness.
WorkSafe, as the regulator, has been slow to identify occupational violence in the health sector as an area of high risk. Its education activities are intermittent rather than systematic and comprehensive. It rarely uses its inspection or enforcement tools to address occupational violence incidents in the health sector.
DHHS and WorkSafe need to provide stronger sector-wide leadership to assist audited agencies to fulfil their responsibilities as employers to effectively protect healthcare staff. Health services and AV, as employers, need to make sure improvements are evidence- and risk-based, well resourced, implemented consistently, reviewed, evaluated and integrated as a whole-of-organisation responsibility. The report makes 10 recommendations aimed at better protecting healthcare workers.
Message
Ordered to be published
VICTORIAN GOVERNMENT PRINTER May 2015
PP No 30, Session 2014–15
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report on the audit Occupational Violence Against Healthcare Workers.
This audit assessed whether agencies are fulfilling their occupational health and safety responsibilities to protect and support healthcare workers in regards to occupational violence.
I found that while public health services, Ambulance Victoria, the Department of Health & Human Services and WorkSafe have each implemented initiatives and actions to support healthcare workers, these are intermittent rather than strategic, not always understood or followed by staff, and rarely evaluated to determine effectiveness.
I cannot be assured that the systems and processes in place to protect healthcare workers are as well understood, comprehensive, robust and embedded in the culture of health services as those that have been put in place for patients.
Yours faithfully
John Doyle
Auditor-General
6 May 2015
Auditor-General's comments
 John Doyle
Auditor-General |
Audit team Michele Lonsdale—Engagement Leader Mandy Charman—Team Leader Janet Wheeler—Senior Analyst Jason Cullen—Analyst Engagement Quality Control Reviewer Renée Cassidy |
Healthcare workers are particularly vulnerable to occupational violence. They may be caring for people whose illness or medication can result in aggressive or violent behaviour, and whose family members may also become abusive out of concern for a loved one. Workers often need to respond to patients whose behaviour is fuelled by drugs such as 'ice' or alcohol. Regrettably, there seems to be a misplaced community expectation that healthcare workers—as members of caring professions—should continue to provide care regardless of the risks they may face.
Community expectation also influences healthcare worker attitudes towards occupational violence. Healthcare workers face a dilemma—refusing service may endanger life and calling police may be seen as an overreaction, particularly if the incident is the result of a clinical condition.
In this audit I examined how effectively systems are protecting healthcare workers. I found shortcomings in all audited agencies. Despite an array of related initiatives—and agencies' stated commitment to addressing this problem through policies, procedures and other actions—the current approach to occupational violence against healthcare workers is neither strategic nor coherent. It does not adequately address the 'normalisation' of occupational violence, where healthcare workers are reluctant to report abuse because it is seen to be 'part of the job'.
Healthcare workers find the incident reporting system cumbersome to use. Some do not report incidents because they believe nothing will be done by management. Many are reluctant to report incidents they perceive to be unintentional, such as when a patient with delirium or dementia engages in aggressive behaviour.
Given the seriousness of this risk, neither WorkSafe nor the Department of Health & Human Services (DHHS) have given this matter the priority it needs. WorkSafe rarely uses its inspection or enforcement mechanisms to address incidents of occupational violence. It focuses instead on education initiatives, but these are sporadic and limited and have not been appropriately evaluated. DHHS' activities to support health services are similarly intermittent rather than strategic. It cannot tell if its various initiatives have been effective because it has not evaluated them.
I found that while health services and Ambulance Victoria have policies, procedures and other risk controls in place, these are not always known, accessed or implemented consistently by staff.
I examined the audited health services' incident data. Incidents categorised as 'mild', 'near miss' or 'no harm' included attempted strangulation, kicking a pregnant woman in the stomach, sexually inappropriate conduct, and being punched. How is it that these sorts of incidents can be assessed as only 'mild' or 'no harm'? Obviously, this sort of categorising understates the risks involved.
Training is inadequate across the board, particularly in relation to conducting investigations, and is generally not mandated. Health services advise that the cost of replacing staff during training is a significant barrier. Given that managing challenging behaviours is an integral part of providing care to ill patients, it is concerning that training to prevent and manage occupational violence is not given higher priority.
Healthcare workers need to report any incident that threatens their health and safety, regardless of whether this incident is unintended or intended. It is not just 'part of the job'. Without reporting, how can employers know the true level and impact of occupational violence and take appropriate action?
Health services and Ambulance Victoria as employers need to actively identify and address barriers to under-reporting, make sure their workers are appropriately trained in ways to prevent and manage occupational violence, and constantly monitor and evaluate their actions and initiatives to make sure these are addressing the issue.
DHHS,as the system manager, needs to provide much stronger leadership. It needs to provide more standards and guidance related to expectations to build consistency and economies of scale—such as developing training tools and modules that could be adapted by health services instead of them having to invent their own.
WorkSafe,as the occupational health and safety regulator, effectively supports the return to work of healthcare workers affected by occupational violence, however, it needs to make much better use of the full array of compliance and enforcement tools at its disposal, including inspections. This would strongly reinforce the message that occupational violence against healthcare workers is not acceptable.
The general public need to be more aware of the impact that violence can have on those who are expected to care for them. DHHS and WorkSafe, in conjunction with health services and Ambulance Victoria, need to take a leadership role in campaigning for better community understanding of the impact that violence can have on healthcare workers and of appropriate behaviours in healthcare settings.
I have made 10 recommendations aimed at better protecting healthcare workers. I intend to maintain a strong ongoing focus on the health and safety of healthcare workers and the patients they treat. I will follow up with the audited agencies in two years to determine whether—and how effectively—my recommendations have been addressed.
John Doyle
Auditor-General
May 2015
Audit summary
Background
Healthcare workers, including doctors, nurses and paramedics, provide a critical role in caring for the community. The community has come to expect that healthcare workers will provide care as and when needed. Occupational violence has been recognised as a significant issue for healthcare workers both in Australia and internationally.
Healthcare workers face particular risks because they are at the frontline when it comes to dealing with people in stressful, unpredictable and potentially volatile situations. For example, some of the day-to-day challenges that healthcare workers may experience include dealing with patients whose clinical condition may lead to unintentional violent behaviour, concerned family members who may become agitated in response to a loved one's situation, and individuals whose drug or alcohol-fuelled aggression threatens the safety of paramedics and health professionals.
It is important that healthcare workers are protected from the risks and incidence of occupational violence both for their own health and safety and to protect the continuity and quality of healthcare services provided to the community.
In its 2011 policy, Preventing occupational violence: A policy framework including principles for managing weapons in Victorian health services, the Department of Health & Human Services (DHHS) defines occupational violence as 'Any incident where an employee is abused, threatened or assaulted in circumstances arising out of, or in the course of, their employment'.
In this audit, we examined whether local and statewide systems are sufficiently and appropriately protecting healthcare workers from the risks and incidence of occupational violence. We focused on:
- DHHS' role as manager of the Victorian health system
- WorkSafe's role as the occupational health and safety regulator in supporting employers to reduce and control occupational violence risks through its education and enforcement activities
- Ambulance Victoria (AV) and selected health services—with a particular focus on three hospitals—in their role as employers responsible for identifying, responding to and preventing or mitigating the risk of occupational violence to protect their workers.
As part of the audit, we interviewed 85 staff across the selected health services and AV, and analysed survey information collected from 89 hospitals across the state.
This audit was commenced under the Department of Health. On 1 January 2015, machinery-of-government changes took effect and the responsibilities of the former Department of Health transferred to DHHS.
Conclusion
Victorian healthcare workers face unnecessary—and preventable—levels of risk in regards to occupational violence. Despite all the audited agencies implementing improvements aimed at preventing and reducing occupational violence, the true extent of the problem in our health services and AV is still unknown. Efforts to mitigate risks are incomplete and inconsistent. There is also limited evaluation of the effectiveness of controls in reducing and managing occupational violence.
There have been systemic failures across all audited agencies in relation to collecting, analysing, and reporting quality data for the purposes of continuous improvement.
DHHS has not used the occupational violence data it collects from health services to identify sector-wide trends and issues or to enable health services to compare progress and share better practice. The data it collects is not consistent or comparable, as health services use the reporting system differently. While DHHS has developed a sector-wide dataset through the Victorian Health Incident Management System, it only collects data related to occupational violence incidents against nurses, not against all healthcare workers. This means that DHHS does not have a complete view of the prevalence and severity of occupational violence against healthcare workers in Victoria, and therefore cannot fulfil the role described in its own occupational violence policy. DHHS also does not know if or how its occupational violence policy and limited guidance material are used, or if its initiatives have been effective, because it has not evaluated them.
WorkSafe has been slow to identify occupational violence in the health sector as an area of high risk. Its education activities and initiatives to support the sector are intermittent rather than systematic and comprehensive. As the regulator, WorkSafe rarely uses its inspection or enforcement mechanisms to address incidents of occupational violence. Instead it has chosen to focus more on its education activities, but these are limited and have not been evaluated for effectiveness.
DHHS and WorkSafe need to provide stronger, sector-wide leadership and to work more closely together to assist health services and AV fulfil their responsibilities as employers to effectively protect healthcare staff. As employers, health services and AV need to make sure that their initiatives and controls are evidence based, resourced appropriately, implemented fully and reviewed regularly. They need to make sure that they are promoted as a whole-of-organisation responsibility, and evaluated in the interests of continuous improvement.
Findings
Understanding occupational violence
While recent research studies show high levels of occupational violence against healthcare workers in Victoria, the true extent is unknown. This is partly because there is significant under-reporting of occupational violence incidents in Victoria—as there is nationally and internationally. It is also because health services' occupational violence data is not of sufficient quality and comparability to provide a statewide picture.
We found that the incidents least likely to be reported are those not requiring medical attention—near misses, verbal abuse, and incidents causing mental or psychological distress. Our examination of the audited health services incident reporting data found that incidents routinely categorised as 'mild', 'near miss' or 'no harm' included attempted strangulation, kicking a pregnant woman in the stomach, sexually inappropriate conduct, and being kicked and punched. Categorising these incidents in this way understates the seriousness of these occurrences and does not enable future incidents or risks to be prevented and managed.
One reason for this under-reporting is staff compassion for patients whose aggression arises from a clinical condition. Staff commonly reason that the patient 'couldn't help it'. Despite relevant policies and procedures highlighting the need for healthcare workers to report occupational violence incidents, there is still a widely held view—consistently reported by staff across all the audited agencies—that clinically caused violence is an inevitable 'part of the job'. However, this very predictability should mean it is easier, rather than more difficult, to prevent.
Other factors contributing to under-reporting include:
- cumbersome incident reporting systems
- logistical barriers, such as being required to complete a report after a shift ends or having limited access to a computer
- the perceived inaction of management in responding to all but the most serious of incidents.
There is some evidence of the audited agencies analysing their security responses, clinical patient records, incident data or WorkCover claims to identify and address occupational violence risks, and of better practice resulting from this analysis. However, this is not done routinely, consistently, comprehensively or across all the audited agencies. As the system manager, DHHS does not provide the necessary oversight and management to make sure high quality and comparable occupational violence data is collected and reported.
Investigations of occupational violence incidents are an important means of identifying the risks, the appropriateness of the controls in place, and ways of improving these controls. However, health services investigate only the most serious incidents, and even then these investigations are not always comprehensive. Incidents rated as only 'mild' or a 'near miss' receive limited investigation, despite their potential for harm. AV requires all reported incidents to be investigated, but the quality of these investigations is variable.
While the audited health services and AV have investigation policies in place, there is minimal support—in the form of procedures, guidance or training—for this investigative role. This suggests there needs to be better guidance and training in health services and AV about how to conduct investigations that can be used to improve controls.
Managing occupational violence
All the audited agencies have implemented reforms in recent years aimed at preventing and managing occupational violence. These include the introduction of specific occupational violence policies and procedures, and a Code Grey response—a hospital-wide coordinated clinical and security response to actual or potential aggression or violence. Code Grey activates an internal alert or emergency response.
Other initiatives include specialist support staff such as psychiatric liaison support staff, clinical behaviour assessment and management plans, training programs, and physical design modifications to mitigate the risk of occupational violence.
However, site visits and extensive staff interviews indicate that occupational violence policies are not communicated effectively, or consistently followed by staff members. We found evidence of poorly implemented risk alerts and behaviour management plans. While operational procedures for some occupational violence triggers are in place in some health services, these are not sufficiently informed by incident and trend analysis, which means they may not adequately address the risk. Other clinical behavioural controls are compromised by inconsistent use, inadequate review to ensure currency or effectiveness, and inadequate communication.
Staff interviewed across the audited agencies reported a lack of consistency in definitions of what constitutes occupational violence and what is considered worthy of reporting. They also perceived that the organisational commitment to staff safety is not promoted as strongly and clearly as patient safety. Site visits indicated that in practice responsibility for reporting is left to the discretion of the individual rather than being a strictly enforced requirement and a whole‑of‑organisation responsibility.
All three audited health services have set up occupational violence management committees to address this issue and review serious incidents. Similarly, AV has established a working group to review occupational violence. It has also recently created the role of prevention manager which includes responsibility for reviewing and improving the controls related to occupational violence. However, AV does not allocate more experienced paramedics to known high-risk areas, or match experienced with less experienced paramedics—despite just under half of its staff having less than five years' experience. AV advises this is not logistically possible. AV has established some controls such as the clinical instructor program and infield manager roles. However, these do not necessarily involve a physical presence and given the potentially volatile nature of the sites paramedics visit, do not appear sufficient to mitigate the risks faced by inexperienced paramedics in the field.
The audited health services and AV have made improvements to work environments—most commonly, the addition of security cameras and duress alarms, improvements to the control of entry points, and redesign of reception rooms. However, such improvements are not undertaken or assessed routinely as part of regular environmental audits.
Training for staff—with the exception of staff within mental health and emergency departments—is inadequate and not commensurate with the risk posed by occupational violence. None of the three audited health services evaluated training effectiveness in building staff skill and capacity to manage occupational violence. Assessment of training is largely confined to participant satisfaction.
Even acknowledging the logistical difficulties of providing regular training to a workforce out on the road for much of the time, training for paramedics is also inadequate. AV provides a one-day training course at the beginning of employment that includes theoretical and scenario-based components. No other refresher training is provided. AV is currently reviewing its training.
While both DHHS and WorkSafe have implemented initiatives aimed at supporting health services to address occupational violence, these have not all been underpinned by appropriate and sufficient data or evidence related to health services' needs. WorkSafe in particular has been slow to act and there is only sporadic evidence of collaboration between the two organisations, including a recently developed in-principle agreement to implement a more integrated approach to data collection, analysis and reporting.
The audited health services and AV consistently identified the need for greater public awareness about appropriate behaviour towards healthcare staff. DHHS and WorkSafe, in consultation with the health sector, need to promote messages to the public about the impact of occupational violence, expected standards of behaviour and potential consequences for poor behaviour.
Post-incident support
All the audited agencies are effectively supporting healthcare workers back into the workforce after they have sustained injuries due to occupational violence. Employment assistance programs are readily available and AV has an effective peer support program.
WorkSafe effectively supports staff returning to work and monitors and enforces employers' compliance with relevant legislation.
Alongside a desire to care for the injured staff member, there are financial incentives and penalties to encourage employers to meet their legal obligations and help injured workers return to work early. These incentives include increasing productivity and lowering the cost of the insurance premium.
Recommendations
- That health services and Ambulance Victoria identify barriers to reporting and develop, implement and monitor improvement strategies to address these barriers in collaboration with staff.
- That the Department of Health & Human Services and WorkSafe work together to provide guidance specifically targeted at occupational violence incident reporting and investigation in line with the detailed advice provided for clinical incidents.
- That the Department of Health & Human Services and WorkSafe—in collaboration with health services and Ambulance Victoria—deliver a joint approach to the collection, analysis and use of industry data on occupational violence incidents against all healthcare workers to improve awareness and understanding of the risk.
- That health services and Ambulance Victoria regularly review and evaluate the effectiveness of their controls to prevent and reduce occupational violence.
- That health services and Ambulance Victoria build on, or develop a comprehensive and tiered occupational violence training program, that is tailored to need, delivered as a refresher on a regular basis, delivered flexibly, and reviewed for effectiveness.
- That health services develop, and Ambulance Victoria enhances existing, investigation training and procedures—including root cause analysis—and undertake compliance monitoring in relation to investigative practices.
- That the Department of Health & Human Services reviews its guidance material on occupational violence and evaluates its uptake and usefulness, including gaps in information.
- That the Department of Health & Human Services in collaboration with health services and Ambulance Victoria develops a set of core occupational violence training tools that can be adapted by health services to their local context as required.
- That the Department of Health & Human Services and WorkSafe work with health services and Ambulance Victoria to develop appropriate public messaging to improve community awareness of the impact of occupational violence on healthcare workers and highlight the need for appropriate and respectful behaviour when seeking medical treatment.
- That WorkSafe more proactively uses its full range of tools—including inspections—to assess occupational violence risks and the effectiveness of controls in health services and Ambulance Victoria.
Submissions and comments received
We have professionally engaged with WorkSafe, the Department of Health & Human Services, Ambulance Victoria and the three audited health services throughout the course of the audit. In accordance with section 16(3) of the Audit Act 1994 we provided a copy of this report to those agencies and requested their submissions or comments.
We have considered those views in reaching our audit conclusions and have represented them to the extent relevant and warranted. Their full section 16(3) submissions and comments are included in Appendix A.
1 Background
1.1 Introduction
The Department of Health & Human Services (DHHS) defines occupational violence as any incident where an employee is abused, threatened or assaulted in circumstances arising out of, or in the course of, their employment. Examples of occupational violence include—but are not limited to—verbal, physical or psychological abuse, threats, spitting, biting, throwing objects, racial vilification, sexual harassment or any form of indecent physical conduct. It can be perpetrated by patients, relatives, members of the public, and other employees. In this audit we excluded occupational violence caused by employees.
Violence within the workplace has been recognised as a significant issue for health service providers both in Australia and internationally. The work often involves caring for and dealing directly with members of the public while they are experiencing illnesses that can contribute to violent behaviour, and while they are in stressful, unpredictable and potentially volatile situations.
1.1.1 Impact
Exposure to occupational violence can have serious social, health and economic consequences, not only for those immediately involved, but for the health sector more generally.
There are substantial economic costs to the health sector associated with sick leave, legal action, diminished staff effectiveness, and the recruitment and retention of staff. These impacts have serious consequences given the increased pressure and demand on the health sector due to population growth and ageing.
In addition to the impact on an individual's mental and physical wellbeing, occupational violence also has a negative effect on bystanders—including colleagues, other patients, and visitors—and more broadly on the quality of patient care and outcomes.
1.1.2 High-risk settings
National and international research has identified certain settings where occupational violence is more likely to occur. These include:
- emergency departments
- mental health settings
- drug and alcohol clinics
- paramedic call outs
- aged care settings
- maternity wards
- intensive care units
- other areas where high stress incidents occur or where there are few staff and limited support.
1.1.3 Contributing factors
Common factors contributing to the incidence of occupational violence against healthcare workers include:
- characteristics of some medical conditions—such as dementia, delirium, mental illness or head trauma, where violence or aggression is a potential clinical symptom
- characteristics of individuals—such as the attributes of the aggressor who may have a history of substance abuse or difficulty dealing with stressful situations, or the characteristics of the victims, such as their level of work experience or communication skills
- characteristics of the relationship—such as the nature of the daily routine and relationships with the patient involving rules, limit-setting, practices around visitor and patient movements, and processes for undertaking caring duties
- organisational and environmental factors—such as the physical layout of the environment, procedures and policies, wait times and staffing practices including access to security or other support
- societal factors—such as community acceptance of violence, or attitudes towards authority.
New challenges in the external environment have also emerged, such as the increased use of drugs and alcohol that have been linked to aggressive behaviour and induced psychosis. Victoria's 2015 Ice Action Plan reports that between 2011–12 and 2012–13, the number of methamphetamine-related ambulance attendances increased by 88 per cent in metropolitan Melbourne and nearly 200 per cent in regional Victoria. During this same period, methamphetamine-related emergency department presentations rose 20 per cent. Violence and paranoia are common behaviours of ice‑affected individuals.
1.2 Reviews and inquiries
1.2.1 Victorian Taskforce on Violence in Nursing
The Victorian Taskforce on Violence in Nursing (the Taskforce) was set up by the former Department of Human Services in 2004. In its 2005 report, the Taskforce made 29 recommendations aimed at reducing the incidence of violence against nurses. It sought to:
- define occupational violence and bullying against nurses
- develop approaches to prevent and manage occupational violence
- promote consistent reporting of incidents
- propose a coordinated approach to addressing these issues.
Key issues identified included organisational culture, positioning the prevention and management of occupational violence as an aspect of occupational health and safety (OHS) risk management, education, public awareness, resources, definitional consistency and a whole-of-organisational plan of action.
1.2.2 Aggression Management in Hospitals Intervention and Compliance Campaign
In 2008–09, the Heads of Workplace Safety Authorities initiated a national compliance campaign about aggression management in hospitals to assess the validity of risk assessments and the effectiveness of controls. It involved audits and employee surveys and was undertaken in response to the relatively high risk of injuries due to aggression within the health industry.
It found that budgets, workload issues, and the nature of the patient population were the most common barriers to successfully controlling aggression. While the majority of hospitals had good systems in place and good compliance, the major weakness identified was the lack of review of controls—such as policies, procedures, training and physical or environmental design. It also suggested that under-reporting of aggression is a significant problem and that a large proportion of employees do not believe that management understands the issue and that it is not committed to reducing the risks.
1.2.3 Parliamentary inquiry into violence and security arrangements
The 2011 Parliamentary Inquiry into Violence and Security Arrangements in Victorian Hospitals and, in Particular, Emergency Departments (the Inquiry) was undertaken in response to concerns about increasing violence in emergency departments.
The Inquiry recognised that progress had been made in response to the Taskforce, but that the Taskforce's recommendations had not been adopted consistently or comprehensively across all Victorian health services. The Inquiry found that additional work was needed to make sure that policies, programs and initiatives were fully implemented, adopted and evaluated. It made 39 recommendations aimed at preventing and reducing occupational violence incidents, including introducing a standardised Code Grey response—an alert to elicit a rapid response to a situation where there is anticipated danger or risk to self or others—encouraging the reporting of such incidents and improving the data collection system.
1.3 Previous audit
1.3.1 Occupational Health and Safety Risk in Public Hospitals
In 2013, VAGO's audit of Occupational Health and Safety Risk in Public Hospitals identified similar key systemic flaws as those identified in the earlier Taskforce and Inquiry reports, including:
- insufficient priority being given to, and accountability for, OHS in public hospitals
- a concerning level of violence and aggression against nurses and other healthcare workers
- insufficient training in the management of occupational violence in public hospitals
- inadequacies in the incident reporting system, incident investigation and evaluation of the effectiveness of risk controls.
The audit made seven recommendations aimed at encouraging health services to give higher priority to the management of OHS, and to the Department of Health—now DHHS—and WorkSafe to work more closely together to assist health services in their OHS responsibilities.
1.4 Legislative and policy context
1.4.1 Occupational Health and Safety Act 2004
Under the Occupational Health and Safety Act 2004 an employer must, so far as is reasonably practicable, provide and maintain a working environment that is safe and without risks to health. This includes identifying and eliminating, controlling or reducing risks to health and safety. It also includes keeping information and records relating to the health and safety of employees and monitoring workplace conditions. An employee must also take reasonable care for his or her own health and safety, and have regard for the health and safety of others. Employers in breach of these requirements can be prosecuted for breach of duty of care.
1.4.2 Crime legislation amendments
The recent Sentencing Amendment (Emergency Workers) Bill 2014 provides increased penalties for the assault of paramedics, nurses, doctors and other staff in hospitals that provide or support emergency treatment. Another Bill—the Justice Legislation Amendment (Confiscation and Other Matters) Bill 2014—was introduced into Parliament in August 2014. This Bill amends the Summary Offences Act 1966 to extend this protection to all healthcare workers, regardless of where they are conducting their professional duties. Offenders will face up to six months jail—double the penalty for a common assault.
1.4.3 Workplace Injury Rehabilitation and Compensation Act 2013
The Workplace Injury Rehabilitation and Compensation Act 2013 stipulates employers' responsibilities around workers' compensation, rehabilitation, return to work, dispute resolution, self‑insurance, WorkCover insurance, premiums and the administration of the WorkCover scheme.
1.4.4 Policy and systems
The former Department of Human Services' 2007 policy, Preventing occupational violence in Victorian health services: A policy framework and resource kit, was developed in response to the 2005 Taskforce to assist health services to prevent and manage occupational violence. The framework identifies five strategic directions to provide effective management and prevention of occupational violence. It applies to all staff employed by public health services, including Ambulance Victoria (AV). In 2011, this document was reviewed and refreshed with new material on principles for the management of weapons.
The Victorian Health Incident Management System (VHIMS) is the sector-wide dataset and classification system developed by DHHS to support the systematic collection of clinical incident data, consumer feedback and OHS data within health services. Health services have incident reporting systems, called Riskman or VHIMS central, which are compatible with VHIMS. For the purposes of this audit we will refer to these systems generically as the incident reporting system used by health services.
The 2003 Public Hospital Sector Occupational Health and Safety Management Framework Model is intended to guide health services in developing a comprehensive and integrated approach to managing their health and safety obligations and fulfil their legislated responsibilities as employers. It provides the overarching approach and structure for the prevention of occupational violence as an OHS risk.
The 2014 Better responses, safer hospitals: Standards for Code Grey responses was developed by DHHS to outline best practice principles and minimum practice standards for standardised organisational responses to the prevention and management of clinical aggression in Victorian health services. These standards may also inform how health services respond to incidents of non-clinical aggression, such as those associated with visitors.
1.5 Roles and responsibilities
1.5.1 Department of Health & Human Services
Under the Victorian Government's devolved governance system for health service delivery, DHHS is the health system manager. It is responsible for monitoring the performance of health services, setting strategic priorities, implementing policy and providing overall system-wide guidance and funding. In its Preventing occupational violence in Victorian health services: A policy framework and resource kit, DHHS states its commitment 'to providing all employees with a healthy and safe workplace free from violence' and its 'duty of care to staff and clients and that of health services to their staff and clients'.
1.5.2 WorkSafe
WorkSafe is the regulator of Victoria's OHS system. Its role includes monitoring and enforcing compliance with the Occupational Health and Safety Act 2004 and assisting in preventing workplace injuries. The provision of information and education activities is also a key function of WorkSafe.
1.5.3 Health services and Ambulance Victoria
Health services are the largest employer group in the public sector. Health services and AV are responsible for implementing systematic and integrated approaches to OHS, in line with their obligations under the Occupational Health and Safety Act 2004. Health service boards oversee public health services and AV in accordance with government policy. They are accountable to the Minister for Health for fulfilling their responsibility to maintain a duty of care and commitment as employers to provide and maintain, so far as is reasonably practicable, a working environment that is safe and without risks to health. Health services and AV are responsible for the daily management of OHS risk in public hospitals.
1.6 Audit objectives and scope
The objective of this audit was to assess whether agencies are fulfilling their OHS responsibilities to protect and support healthcare workers in regards to occupational violence.
The audit focused on:
- the role of health services and AV as employers of healthcare workers
- DHHS as the manager of the Victorian health system
- WorkSafe as the OHS regulator.
The selection of health services was based on a number of factors, such as location, size, and range of services offered. We chose three health services and conducted site visits at one hospital in each of these. The hospital selection comprised a large hospital in metropolitan Melbourne, a hospital in outer metropolitan Melbourne and a hospital in regional Victoria.
This audit was commenced under the Department of Health. On 1 January 2015, machinery-of-government changes took effect and the responsibilities of the former Department of Health transferred to DHHS.
1.7 Audit method and cost
Audit methods included:
- reviewing relevant documents, including policies, plans, strategies, data, and reporting on occupational violence against healthcare workers
- site visits
- extensive interviews with DHHS, health service and AV staff
- analysis of WorkSafe data on occupational violence related claims
- a survey of 89 hospitals that focused on their systems, policies and procedures to support occupational violence prevention and management.
The audit was conducted in accordance with section 15 of the Audit Act 1994 and the Australian Auditing and Assurance Standards.
Pursuant to section 20(3) of the Audit Act 1994, unless otherwise indicated, any persons named in this report are not the subject of adverse comment or opinion.
The total cost of the audit was $430 000.
1.8 Structure of the report
The report is structured as follows:
- Part 2 examines what is known about the prevalence and severity of occupational violence and aggression against healthcare workers, and the challenges of gaining a more comprehensive picture.
- Part 3 examines health services' controls, including policies and practices, the introduction of the Code Grey response, and the training and educational guidance and support provided by DHHS and WorkSafe.
- Part 4 examines health services' policies and practices related to employees returning to work, and WorkSafe's compliance and return-to-work activities with individuals and health services.
2. Understanding prevalence and severity
At a glance
Background
Comprehensive incident reporting, monitoring, and investigations are essential to effectively manage the risk and incidence of occupational violence in the health sector.
Conclusion
There have been systemic failures to collect, analyse, and report on quality data for the purposes of continuous improvement across health services, Ambulance Victoria (AV) and the Department of Health & Human Services (DHHS). As a result, health services, AV, WorkSafe and DHHS do not know the actual prevalence and severity of occupational violence experienced by healthcare workers.
Findings
- There is significant under-reporting of occupational violence incidents.
- Barriers include cumbersome reporting systems, reluctance to report the 'unintentional' violence of ill patients and perceived management inaction.
- Analysis of incident data to identify and address occupational violence risks is not comprehensive or consistent across the health sector.
- DHHS only collects data from health services on occupational violence incidents against nurses, not against other healthcare workers, and does not make sure that the incident data provided is comparable and of suitable quality.
Recommendations
- That health services and AV identify and address reporting barriers and implement and monitor improvement strategies.
- That DHHS provides additional guidance specifically targeted at occupational violence incident reporting and investigation.
- That DHHS in collaboration with WorkSafe deliver a joint approach to the collection, analysis and use of high-quality data to drive improvement.
2.1 Introduction
As employers, health services and Ambulance Victoria (AV) collect occupational violence incident data. This data, if analysed and reviewed, can help them identify and address the areas of highest risk. In its 2011 policy, Preventing occupational violence: A policy framework including principles for managing weapons in Victorian health services (occupational violence policy), the Department of Health & Human Services (DHHS) outlines its role in the sector-wide monitoring of occupational violence in healthcare. Through collecting de‑identified data about occupational violence from health services, DHHS stated it would identify statewide trends related to occurrence, impact and effective management of occupational violence. DHHS intended to use this information to promote better practice, establish consistent minimum standards, and identify sector‑wide risks that require a whole-of-sector leadership response.
2.2 Conclusion
While recent studies indicate that the number of occupational violence incidents against healthcare workers is high, it is difficult to determine the true extent because of extensive under-reporting and because health service and AV data is not always reliable or comparable across the sector. There have been systemic failures across health services, AV, and DHHS to collect, analyse, and report on quality data for the purposes of continuous improvement. Without a strong evidence base, it is difficult to make informed decisions about the prioritising and targeting of resources and the effectiveness of interventions.
2.3 Understanding prevalence
In the absence of a comprehensive and accurate data set, we examined a range of data sources to gain greater insight into the extent of the issue in the health sector broadly and in the audited health services and AV specifically. These data sources included:
- findings of key research studies
- WorkCover claims data with a focus on the occupational violence incidents that have resulted in two weeks or more absence from work
- clinical patient incident data which reflects occurrences of occupational violence recorded in the patient incident system
- occupational health and safety (OHS) incident reporting data which reflects incidents of occupational violence recorded on the OHS incident system.
2.3.1 Research studies
Figure 2A provides a sample of recent research studies that have found high levels of occupational violence incidents against healthcare workers in Victoria.
Figure 2A
Recent studies of occupational violence against healthcare workers
|
Source: Victorian Auditor-General's Office.
This research provides some insight into the extent of occupational violence experienced by healthcare workers generally. However, when we sought to understand the level of occupational violence in the three audited health services and AV we found significant barriers.
2.3.2 WorkCover claims
WorkCover claims data represents the most serious occupational violence incidents. It does not reflect 'near misses' or other incidents not resulting in claims.
WorkSafe claims data for 2005–14 shows that:
- 37 per cent of all occupational violence claims are lodged by the healthcare and social assistance industry, with 12 per cent coming from the healthcare industry
- public hospitals account for 94 per cent of claims within the healthcare industry
- registered nurses, welfare and community workers, personal care and nursing assistants, and registered mental health nurses are in the top 10 occupations that are most exposed to incidents of occupational violence
- 10 metropolitan hospitals account for 46 per cent of all public hospital occupational violence-related claims—two of the audited health services are within this group of 10 hospitals, with one of these having a disproportionately high number of claims.
When we examined the WorkCover claims data of the specific health services that were audited, we found discrepancies in the claims data provided by one of the audited health services and AV when compared with that provided by WorkSafe. For example, during 2009–14 WorkSafe reported 17 occupational violence-related WorkCover claims for one audited health service, while the health service reported 75 claims.
This discrepancy reflects the lack of a standardised approach to identifying occupational violence claims. Because the cause of injury is not coded as part of the claim, WorkSafe, health services and AV need to manually identify those claims that relate to occupational violence.
At our request, WorkSafe created a method to identify claims related to occupational violence. It advised us that the cause of injury is not systematically collected and consistently coded by claimants, who may describe an incident in multiple ways. This means an incident may be not be correctly identified as related to occupational violence, and this makes WorkCover claims data problematic as a means of understanding prevalence. However, there is an opportunity for WorkSafe to create consistent standards for identifying occupational violence claims. In the absence of other data sources, WorkSafe could, with only small modifications and enhancements to the current approach, use WorkCover claims data to increase sector knowledge of occupational violence prevalence.
2.3.3 Clinical patient incident data
We also examined health services' clinical patient incident data as a potential source of information about the level of occupational violence.
Healthcare workers can report occupational violence as a clinical patient incident as well as an OHS incident within the incident reporting system. Stakeholders advised that clinical patient incident reporting was more complete than OHS incident reporting because it focuses on all occurrences of occupational violence as an aid to manage clinical symptoms and treatment.
While promising, a range of issues prevents this data from providing clarity on the prevalence of occupational violence. Some of the issues that became apparent through trying to use this data included:
- under-reporting of clinical patient incidents, which is also common
- difficulty of interpretation—it is not possible to know whether high numbers of incident reports in the patient incident records indicate a strong safety culture where reporting is comprehensive, or alternatively a high prevalence rate and therefore an environment where occupational violence risks are poorly managed
- incomparability of data—as it is counted, coded and managed differently across health services and AV. When we sought clinical data from the audited health services and AV we found that:
- in one audited health service there was double counting of clinical patient incidents
- in another health service, the most reliable data on occurrences of occupational violence was considered to be security recording of Code Grey responses, because patient clinical incident reporting was known to be seriously under‑reported. In the absence of any other data, security data was used effectively by this health service to inform its decision-making. However this data is also incomplete and imperfect as it does not capture clinical aggression that did not result in a Code Grey response.
2.3.4 OHS incident reporting
We also examined OHS incident data as a potential source of information about the extent and severity of occupational violence.
Healthcare workers report occupational violence incidents in the OHS incident reporting system. Audited health services and AV have policies and/or procedures that require all occupational violence incidents to be reported, including threats and near misses. This is in line with DHHS' occupational violence policy which specifies that 'encouraging incident reporting is critical to prevention and management of occupational violence and is integral to achieving culture change'. Under this policy, occupational violence is defined as all incidents, threats and near misses where neither intent nor ability to carry out the threat is considered relevant.
AV and the audited health services have training materials that direct staff to report incidents, but these have several issues:
- One health service's training is in draft form and has not yet been rolled out.
- Another health service's training only refers to reporting incidents that occur in conjunction with a Code Black and Code Grey response, which are calls for additional support to manage threatening situations. It does not refer to clinical or OHS occupational violence incidents that occurred without the initiation of a Code Black or Grey.
- One health service advised that it provides ad hoc training in the use of its local incident reporting system to report all clinical and OHS-related incidents—however, no documentation was provided to support this.
- None of the audited health services' training provides guidance on how to complete incident reports. DHHS provides an online training package that outlines how to report an incident in the Victorian Health Incident Management System (VHIMS). However, site visits and staff interviews indicated that there was little knowledge of this information and considerable confusion and difficulty in using the system—hence the inconsistent use of the system within and across health services.
Despite requirements to report incidents—and some support for reporting—extensive under-reporting of occupational violence incidents mean that this data provides only limited insight into prevalence, severity, or the effectiveness of controls.
2.3.5 Under-reporting
Of the 89 hospitals that completed a survey as part of our audit, 58 per cent specified that there was under-reporting of occupational violence incidents. The main reasons given were that it takes too long to report—53 per cent—and that the reporting system is too hard to use—51 per cent.
Extent of under-reporting
While under-reporting is well known, there was limited evidence that health services sought to determine the extent of under-reporting. One health service compared its security data of Code Grey calls with that of the clinical patient record and identified high levels of under-reporting.
Analysis undertaken of AV data indicates a significant discrepancy between the numbers of occupational violence incidents reported by paramedics in the patient information records compared with the number reported in the OHS incident reports. The OHS incident reports show how commonly paramedics are exposed to aggression and violence on site. In 2013–14, there were 3 774 occurrences of patient or bystander aggression recorded in the patient information records. This includes instances where the aggression is directed towards paramedics and incidents where it occurs between others on site. It also includes incidents where the aggression may have occurred well before AV's attendance and there is no threat to the paramedic. Of the 3 774 occasions recorded, only 314 were reported as an OHS incident. Because AV has not analysed its data, it does not know how many of the reported occurrences reflect situations where paramedics were either directly or indirectly confronted by aggression or violence.
Reasons for under-reporting
Site visits and key stakeholder interviews identified a range of reasons for under‑reporting:
- Incident reporting systems are cumbersome:
- AV uses a manual system that is difficult for paramedics to access on the road.
- The incident reporting system used by health services is not suitable for reporting occupational violence incidents, has multiple overlapping codes, insufficient relevant fields and a complex interface. It can take 40 minutes to report a single incident and involves scrolling through multiple redundant fields. DHHS is currently undertaking a project in consultation with health services to simplify and improve the OHS component within VHIMS and assist health services to report occupational violence incidents. DHHS advises that this work is due for completion in the second half of 2015.
- Staff have compassion and sympathy for patients whose aggression arises from a clinical condition—staff report feeling that the patient 'couldn't help it'.
- There is a view that clinical violence is an inevitable part of the job—for example, interviews elicited repeated comments that the frequency of occupational violence incidents meant that if staff reported every incident 'you would be reporting all day'.
- Staff perceive a lack of management action in responding to incidents—our analysis of incident reports highlights poor investigation and response for any but the most serious of incidents.
- There are logistical and equipment barriers to reporting—including being required to complete a report after a shift ends and difficulty accessing computers.
Agencies are implementing specific measures to address these factors, including:
- following up with staff by OHS or quality and risk staff to complete reporting
- providing specific guidance around reporting, such as a 'cheat sheet' to assist staff to complete incident reports
- displaying posters that remind staff about the requirement to report
- providing incident reports to demonstrate to staff that reporting is important
- establishing a dedicated support role to make sure coding and data management practices are consistent.
Figure 2B shows how AV has sought to address incident reporting issues.
Figure 2B
AV improvement to data reporting system
|
An internal risk assessment by AV in 2009 identified under-reporting as an issue. Paramedics need to complete a report manually when they return to work after an incident and these reports are then transferred to an electronic database. AV is in the process of moving from a manual to an electronic system, which is to be piloted in 2015. This system is expected to increase incident reporting since paramedics will be able to report incidents electronically in the field. |
Source: Victorian Auditor-General's Office based on information provided by AV.
This is a positive step by AV but has been slow to occur and needs to be coupled with other strategies to encourage reporting and investigation.
What is reported and by whom
Site visits and interviews across the audited health services identified that the likelihood of an incident being reported within the OHS incident system was influenced by the seriousness of the injury, the perception of the degree of threat, and the patient's intent or capacity to take responsibility for their actions. This practice is in direct contrast to the stated requirements of the health services and AV.
Figure 2C shows the incidents that are most, and least, likely to be reported by healthcare workers.
Figure 2C
Occupational violence incidents that are more and least likely to be reported
|
Incidents more likely to be reported |
Incidents unlikely to be reported |
|---|---|
|
|
Source: Victorian Auditor-General's Office based on interviews at audited health services and AV.
Visits to the audited health services and interviews with staff indicate that healthcare workers in certain areas of a health service are more likely to report occupational violence than others. We were advised that emergency department staff, mental health staff, doctors and support staff are less likely to report. In contrast, ward staff and new paramedics are more likely to report. These differences were explained by stakeholders as being at least partly a result of the degree of exposure and desensitisation—with mental health and emergency department workers more likely to have high exposure to violent behaviour.
2.4 System-wide understanding of occupational violence
In response to a 2005 Victorian Taskforce on Violence in Nursing recommendation, DHHS' occupational violence policy states its role in the system-wide monitoring of occupational violence in healthcare. DHHS collects occupational violence data through a monthly upload from health services' incident reporting systems. Analysis of this data is intended, as outlined in DHHS' policy, to inform the production and dissemination of reports on system-wide aggregated data and to enable system‑wide trends to be monitored.
While DHHS identifies in its policy the importance of reporting occupational violence against all healthcare workers, DHHS' data upload is limited—through specifications established by DHHS in VHIMS—to incident reports of occupational violence against nurses only. Limiting the reporting requirement in this way compromises the stated objective of obtaining a sector-wide understanding of occupational violence trends. Even for this limited data collection, DHHS does not monitor whether health services transmit this data.
2.4.1 Data collection issues
In addition, we identified a range of other issues with the collection of data related to occupational violence.
Inconsistent recording of data by health services
Some health services record occupational violence data in the clinical rather than the OHS component of their incident reporting system. Transmitting data only from the OHS component therefore produces a misleading result.
One of the audited health services was in the process of developing an alternative incident reporting system and advised us that it would be compatible with VHIMS. DHHS does not know how many other health services across the state may have developed alternative systems or the compatibility of these systems with VHIMS.
Staff in the audited health services reported that a lack of specific guidance about how to use the reporting system has resulted in inconsistencies in the way it is being applied. While DHHS provides an online reporting training package, this is poorly known, which suggests that DHHS needs to undertake additional work to communicate, support and assess whether this material is meeting health service needs. It also needs to more actively monitor data reporting practices to make sure the data is capable of being compared across health services.
Inadequate monitoring of occupational violence data submission
DHHS does not review whether health services provide incident data relating to occupational violence. One of the audited health services assumed that DHHS was no longer collecting occupational violence data as it had been unable to transmit its occupational violence data through the reporting system since 2012. The health service itself did not follow up with DHHS about this issue and DHHS was unaware that no data had been received from this health service since 2012.
Insufficient quality control
DHHS assumes health services have assured the quality of the data prior to sending it and does not undertake this assurance itself. This has resulted in a situation where DHHS is unable to distinguish between zero occurrences and a failure to report.
2.4.2 Use of data collected
DHHS has been collecting data on occupational violence incidents since 2010, though this is limited to incidents against nurses only. This means that occupational violence incidents against other healthcare workers are not being captured at the sector level, which further limits DHHS' capacity to gain a sound understanding of the prevalence and severity of occupational violence incidents across Victoria's public health system. Discussions with representatives from the health services highlight their dissatisfaction with DHHS' failure to provide occupational violence data trend reports back to them and the burdensome nature of a reporting exercise that therefore appears to be futile.
In response to the recommendations of VAGO's 2013 Occupational Health and Safety Risk in Public Hospitals audit, DHHS is undertaking a project, in consultation with health services, to improve the OHS component within VHIMS. This is due to be implemented in the second half of 2015. However DHHS has not been able to provide us with sufficient and appropriate evidence regarding:
- how current reporting inconsistencies across health services and VHIMS will be identified and managed
- how health services will be encouraged to take up the improved data collection model
- how adherence will be monitored.
While the project is to be welcomed as it has focused on simplifying the reporting process, it alone is insufficient to address the inadequacies in the data collection system, which is as much a result of inadequate management and oversight as the limitations of the reporting tool.
In the absence of rigorous and systematic data collection to enable analysis, DHHS uses other mechanisms to identify emerging issues—such as the Improving Hospital Safety and Security Ministerial Advisory Committee, health service forums and cross‑sector committees. The value of these mechanisms to adequately inform the understanding of such a significant issue has not been demonstrated and is questionable.
In response to VAGO's 2013 OHS audit and this audit, DHHS and WorkSafe have recently established an in-principle agreement to undertake a joint Health Services Industry Data and Collaboration Initiative. This is expected to provide a more integrated approach to data collection, analysis and reporting of health services' OHS incident data, including occupational violence incidents. This signals a positive development in sector-wide leadership. It is expected that this project will consider issues related to data definition, management, and quality assurance processes to make sure that data is high quality and comparable. This initiative needs to be treated as a priority.
Recommendations
- That health services and Ambulance Victoria identify barriers to reporting and develop, implement and monitor improvement strategies to address these barriers in collaboration with staff.
- That the Department of Health & Human Services and WorkSafe work together to provide guidance specifically targeted at occupational violence incident reporting and investigation in line with the detailed advice provided for clinical incidents.
- That the Department of Health & Human Services and WorkSafe—in collaboration with health services and Ambulance Victoria—deliver a joint approach to the collection, analysis and use of industry data on occupational violence incidents against all healthcare workers to improve awareness and understanding of the risk.
3 Responding to occupational violence
At a glance
Background
Evidence-based controls that are regularly reviewed and evaluated are critical to effectively managing occupational violence. Controls include policies, procedures, specialist staff, clinical behaviour plans, the use of Code Grey response, the physical design of hospitals and training.
Conclusion
All the audited agencies have implemented initiatives to better protect healthcare workers. However, there are still significant and concerning gaps where stronger controls are needed to better reflect the seriousness of the risk to these workers. Neither the Department of Health & Human Services (DHHS) nor WorkSafe is providing ongoing, systematic and robust leadership to assist health services and Ambulance Victoria (AV) to better protect workers.
Findings
- There is insufficient oversight of compliance with relevant policies and procedures, and limited review and evaluation of controls.
- With the exception of staff working in mental health, there is insufficient training for healthcare workers.
- DHHS does not assess the effectiveness of its policy framework or other guidance to identify opportunities for improvement.
- WorkSafe has conducted only sporadic education and limited enforcement activities.
Recommendations
- That health services and AV regularly review and evaluate their controls and implement comprehensive, targeted, flexible training.
- That DHHS reviews its guidance material and evaluates uptake and usefulness.
- That DHHS in collaboration with health services and AV develop a set of core occupational violence training tools.
- That all audited agencies collaborate to develop appropriate public messaging.
- That WorkSafe more proactively uses inspections to educate and enforce.
3.1 Introduction
The 2011 Parliamentary Inquiry into Violence and Security Arrangements in Victorian Hospitals and, in particular, Emergency Departments (the Inquiry) identified a range of controls which, if implemented, would help prevent, or at least reduce, the risk of occupational violence in Victorian health services. Given that it has been three years since the Inquiry, we expected to see the following controls implemented by the audited health services:
- policies and procedures that communicate that violence is unacceptable
- specialist staff support
- clinical behaviour assessment and management plans
- a standard, consistent Code Grey response
- the utilisation of Crime Prevention through Environmental Design principles
- comprehensive and targeted training programs.
3.2 Conclusion
All the audited agencies have implemented initiatives to better protect healthcare workers. However, there are still significant and concerning gaps where stronger controls and actions are needed to better reflect the seriousness of the risk to these workers. Neither the Department of Health & Human Services (DHHS) nor WorkSafe is providing ongoing, systematic and robust leadership to assist health services and Ambulance Victoria (AV) to better protect workers.
3.3 Policies and procedures
DHHS requires all health services and AV to have a current occupational violence policy. However, it does not monitor whether health services or AV are fulfilling this requirement. Of the 89 hospitals that completed our survey, 92 per cent reported that they have a specific occupational violence policy, indicating an organisational commitment to managing this issue. Those who reported having no policy were mainly rural hospitals. All three of the audited health services have specific occupational violence policies and related procedures. While AV does not have a specific occupational violence policy, it does have a set of procedures relating to aggression management, but not all of these have been reviewed or updated in the past four years.
Site visits and staff feedback indicate limited oversight of, and accountability for, making sure these policies are being adhered to across the organisation. A range of issues were identified which highlight noncompliance with relevant policies and procedures. In particular, we found examples of persistent under-reporting—as discussed in Part 2 —poor investigation, and poorly implemented risk alerts and behaviour management plans across all the audited health services and AV.
Staff interviewed across the audited agencies also reported:
- a lack of clarity regarding what constitutes occupational violence and what should be reported
- poor knowledge of policies and procedures
- staff safety not being as clearly and strongly promoted as patient safety
- that it was an individual's choice whether to report an occupational violence incident, rather than a requirement as part of a whole-of-organisation responsibility—this leaves the way open for staff not to report something because it is perceived to be 'unintentional' on the part of a patient or 'just part of the job'.
3.4 Emergency controls—Code Grey
The introduction of Code Grey across many Victorian health services is a positive step. There are nevertheless issues associated with training, staffing of Code Grey teams and inconsistent use and recording of Code Grey incidents.
In 2011, the Inquiry recommended establishing a standard for Code Grey responses in health services. In 2014, DHHS released these standards for Code Grey responses which outline best practice principles and minimum practice standards for organisational responses to incidents of clinical aggression in Victorian health services.
The standards define a Code Grey response as a hospital-wide coordinated clinical and security response to actual or potential aggression or violence not involving a weapon. Code Grey activates an internal alert and a clinically-led emergency response. This means an appropriate clinical response, in coordination with security as required, can be provided to manage the clinical conditions that can commonly result in violence. The standards also allow for the use of a Code Grey response to instances of non-clinical aggression, such as that enacted by visitors.
Our survey and site visits identified that in practice Code Grey responses have a range of other features. These include planned Code Grey responses—and, in some instances, security-led Code Grey responses. While not included in the DHHS standards, planned Code Grey responses were identified as valuable by staff in the audited health services because they have found it to be a useful pre-emptive measure in which a Code Grey team is convened in anticipation of a situation where there is a known high risk of occupational violence.
Of the 89 hospitals that completed our survey, 66 hospitals, or 74 per cent, reported that they have a Code Grey response, with 86 per cent of these hospitals using a clinically-led Code Grey. Sixty per cent—or 40—of those hospitals that report having a Code Grey response also use a planned Code Grey.
All three of the audited health services have a Code Grey in place. One introduced it in 2008, one in mid-2013, and the remaining audited health service is in the process of introducing a clinically-led Code Grey after having a security-led Code Grey since 2008. This is a positive step for this health service as a Code Grey response led by security rather than clinical staff is not considered best practice. This is because security staff are unlikely to have the necessary clinical expertise to respond to the clinical conditions that can result in violence.
Two of the audited health services use a planned Code Grey response, and one is considering introducing it.
Visits to the audited health services highlighted the important role the introduction of Code Grey has played in building momentum around the prevention and management of occupational violence. In two of the audited health services the introduction of Code Grey has generated additional resources and improvements such as the creation of specialist roles and an increased focus on training and other controls. Across the audited health services, staff advised us that they feel safer because of Code Grey and that it is seen as an indication that their safety is being taken seriously by senior management.
However, staff in the audited health services also identified several issues including:
- an over-reliance on security to take the lead in responding to Code Grey calls, rather than clinical staff taking this role
- inconsistent use of Code Grey, pointing to the need for greater training to promote consistent understanding of when and how to call Code Greys—for instance, some staff may wait until after significant escalation to call a Code Grey response, thus increasing the risk to themselves and others
- challenges faced by a Code Grey team in responding to multiple calls at the same time, or trying to balance responding to calls with other duties
- the need for Code Grey teams to have the necessary capability and confidence to manage potentially physical situations
- incomplete reporting of Code Grey calls—resulting in a failure to alert other staff about patients with a high propensity towards violence.
The audited health services do some analysis of Code Grey trends and present this information to internal committees. However, more analysis could be done to identify potential improvements in processes. For example, audits of Code Grey incidents undertaken by one health service informed the development of procedures to assist management of violence triggers, such as restrictions to patients' smoking.
Instead of a Code Grey response, AV uses a duress alarm system for paramedic safety. The response is coordinated by the call centre duty manager and involves police attendance, a second ambulance and an infield manager. Paramedics report that this system works well. However, AV does not record false alarms or analyse their information to inform operational improvements.
3.5 Training and education
Training is critical to building a robust safety culture that protects workers.
We found a high proportion of health services provide training relating to occupational violence management—81 per cent of the 89 hospitals surveyed. However, there is limited evidence of this training being evaluated to determine whether it is targeted appropriately and has given staff the necessary skills and confidence to manage potentially violent or aggressive patients.
All three of the audited health services have well established and comprehensive occupational violence training for mental health services. This is provided every two to three years, with annual refreshers and, in one instance, monthly and weekly tutorials and debriefing. In two of the health services this training was also provided to security staff. Forty-four per cent, or 39 of the 89 hospitals report that training is a mandatory requirement for security staff and staff in mental health and emergency departments.
Two of the health services also have training on the prevention and management of occupational violence for general health staff. The remaining health service has secured funding and resources to deliver such training in 2015.
Two health services currently provide online training and face-to-face courses of between two hours and two days duration. They each have a suite of programs including general online information, courses in managing aggression, and training for home visit risk assessment and Code Grey response. They also provide training targeted to specific groups—including doctors, dental services, hospital in the home, aged care and mental health services. However, site visits and staff interviews highlighted several issues including:
- the reduction of training from half a day to a two hour session in two health services, which was highlighted by key staff as being insufficient to cover the necessary material
- none of the health services evaluated whether their training built staff competency and capacity for managing occupational violence—assessment of training is largely confined to participant satisfaction
- additional refresher training and debriefing are needed for both Code Grey teams and general staff in relation to use of Code Grey responses.
Audited health services and AV have pointed out the challenge of evaluating the effectiveness of training. This is an area where DHHS, as manager of the health system, could step up its sector-wide leadership and provide guidance on effective evaluation techniques.
The audited health services identified the cost of back-filling staff as a significant constraint to training.
DHHS and WorkSafe—as system manager and regulator respectively—could help health services save time and money involved in developing their own training materials by providing sector-wide guidance and tools for training and evaluating training effectiveness. This would provide the basis for consistent, high-quality training and support the evaluation of training effectiveness across the sector.
AV is currently reviewing its training for paramedics. It provides a one day training course at induction that includes theoretical and scenario-based components. No refresher training is provided. AV advises that training is also provided on the job by clinical instructors who mentor new paramedics in all aspects of their duties. This includes managing challenging behaviours and assessing situations to enable safe management of the site. However, paramedics have advised that there are not enough suitably experienced clinical instructors to respond to existing needs—as a result paramedics with only a few years' experience are performing clinical instructor roles. This is a concern given that 50 per cent of AV's workforce has less than five years' experience. While AV advises that it has increased resources in the past 12 months to address this shortage, the issue we identified relates more to the level of experience than the number of clinical instructors. As the bulk of its workforce is on the road, AV needs to more actively explore options for providing flexible or blended training, which may involve combining various styles of training—online, face-to-face and practical.
3.6 Environmental design controls
Audited health services and AV have implemented changes to the environmental design of their workplaces to improve security, but these are not undertaken routinely.
Of the 89 surveyed hospitals:
- only 19 per cent have a formal plan for regular environmental audits
- 58 per cent undertake environmental audits as needed
- 13 per cent undertake no audits of their physical layout.
All the audited agencies have introduced design improvements to mitigate the risk of occupational violence, including:
- signs stating that violence is not acceptable
- the use of closed circuit TV to help deter and identify perpetrators of violent behaviour
- physically separating highly unstable patients from the general patient population
- reducing wait times in emergency rooms through instructions and signage, advising patients of alternative pathways to medical treatment, such as local bulk billing GPs.
Figure 3A shows one health service's initiative to manage challenging behaviour.
Figure 3A
Managing challenging behaviours through the Behavioural Assessment Short Stay Unit
|
In response to the challenging behaviours of some patients who need stabilising—for example, because they are coming off drugs—one audited health service has set up a Behavioural Assessment Short Stay Unit. This is managed within the existing emergency department by a team with specific expertise. The health service's intention is ultimately to change the infrastructure to provide separate, attached facilities. |
Source: Victorian Auditor-General's Office based on information from an audited health service.
In one audited health service there is little provision for the intake or management of patients with aggressive behaviours into the emergency department other than through restraint on a trolley or in a cubicle close to the centre of the emergency department where they can be more closely observed. Efforts to create a separate treating room have not yet been endorsed because of resource limitations. However, the current situation poses significant risk.
A common perception across audited agencies is that reform requires more resources. Figure 3B shows what can be done within an existing built environment without significantly increasing resources.
Figure 3B
Modifying the waiting area to manage occupational violence risk
|
An environmental design modification that has significantly improved management of occupational violence at one of the audited health services was to decommission the existing emergency department waiting area which had been identified as a high-risk environment for occupational violence. A waiting area for all patients has been established within the emergency department itself to improve observation, provide accessibility for rapid triage and identify potential patient escalation for quick response. The previous waiting area is now only used for family members of patients receiving treatment. The health service intends to change its emergency department structural layout to accommodate this new way of managing patients. |
Source: Victorian Auditor-General's Office based on information from an audited health service.
3.7 Other controls
Health services and AV use a range of other controls to prevent and manage occupational violence, including:
- occupational violence and aggression governance committees
- organisational risk ratings and registers
- specialist support and staffing controls
- clinical behavioural controls.
Most of these were identified in recommendations by the Inquiry. The use of these controls reflects significant progress in the management of occupational violence.
3.7.1 Occupational violence management committees
The 2011 Inquiry recommended that hospitals 'should be encouraged to form security and aggression management committees and teams with representation from executive management, security staff, medical, nursing and allied staff including, where relevant, members of mental health and alcohol and drug teams'.
Of the 89 surveyed hospitals, 53 per cent had an occupational violence management committee, including all three of the audited health services. In addition, one audited health service and AV have introduced other working groups to examine occupational violence issues.
However, the occupational violence management committees within the three audited health services have differing levels of executive oversight and scrutiny. The committees are also constrained in what they can achieve by the extensive under‑reporting of incidents, poorly managed data, and the inadequate investigation of incidents.
For example, one health service reported that between 2009 and 2014 they had 136 WorkCover minor and standard claims related to occupational violence. These had cumulative costs of $3 971 281. This is significantly higher than the other audited health services and AV. This would be important information for the occupational violence management committee to assess and act on. However, a review of the relevant committee meeting minutes has not identified a single reference to this high WorkCover claims rate. This is a concern given that WorkCover claims represent the most serious forms of occupational violence that health workers experience. It may be that in the absence of regular and timely sector-wide trend analysis provided by either DHHS or WorkSafe, the health service is unaware of its poor performance in relation to WorkCover claims from occupational violence.
3.7.2 Organisational risk ratings and registers
All the audited health services and AV have determined their organisational risk rating in relation to occupational violence as high or very high. In the past two years, two of the audited health services have changed their risk rating after review, with one increasing the severity from medium to high and the other reducing it from extremely high to high.
However, our review of risk registers showed that understanding of the risks and triggers for occupational violence is not underpinned by sufficiently robust incident data, systematic reviews of past incidents or analysis of incident trends. Despite assessing occupational violence risk as high, audited health services and AV do not identify all the known risks and controls, including common triggers of aggression such as time of day, inexperienced staff and wait times.
3.7.3 Specialist support and staffing controls
Audited health services and AV have established specialist roles to oversee and inform strategies for managing occupational violence. These include occupational violence coordinator and training roles in the health services, and a prevention manager role in AV which includes responsibility for overseeing occupational violence system improvements. Six per cent of surveyed hospitals reported that they have established a specialist occupational violence role. An additional 66 per cent, or 59 hospitals, reported including responsibility for occupational violence in a broader role.
Other specialist roles established in some health services and AV include:
- psychiatric liaison support staff that are considered particularly valuable
- drug and alcohol clinicians in the emergency department
- security standby, where security staff stay with at-risk patients in the emergency department
- personal care attendants to observe patients at risk and raise the alarm as needed
- a peer support program within AV that involves support staff proactively providing guidance to paramedics in challenging situations.
While the audited health services and AV had not reviewed these roles for effectiveness, staff and management advised that they were highly valued. In one health service where psychiatric emergency liaison support was not provided, staff identified an increased risk in the management of challenging behaviours within the emergency department.
However, interviews with management and staff across the health services and AV also highlighted the risk of over-reliance on these roles and a shifting of responsibility for addressing occupational violence on to a few individuals, rather than on the organisation as a whole.
3.7.4 Clinical behavioural controls
Communication alerts placed on patients' files and patient behavioural plans are a critical means of identifying and managing patients at risk of violent behaviour. The absence—or lack of effective use—of these mechanisms was identified as increasing the risk to staff as patients move through the health service. However, these alerts need to be used cautiously, have procedures around their application and be regularly reviewed to ensure patients' rights and privacy are protected. All audited health services and AV use these. One health service also advised us that it uses evictions as a mechanism to protect workers, if the patient's illness is not life threatening. This sends a strong signal about the consequences of continued unacceptable behaviour. In 2013–14, there were 66 instances where patients or visitors were asked to leave by security at this health service.
Staff across all agencies reported a lack of clarity around how to place an alert and the absence of mechanisms to review and update them. Multiple examples were given of failures in the alert system—including failures to place alerts and failures to develop behaviour management plans or provide sufficient information about patients being transferred to other services.
Figures 3C and 3D show the significant risk faced by staff as a result of failure to pass on information effectively.
Figure 3C
Risk associated with failure to update behaviour management plans
|
One nurse unit manager described how a former patient—who had been a known security risk with repeated self-harm and violence incidents—had returned to the health service after release from prison. The nurse unit manager involved reported that no effort had been made to re-establish the behaviour management plan used during the patient's previous visit, which included the ongoing attendance of a security officer. This meant general ward staff were required to manage persistently challenging behaviours and felt at considerable risk. This situation had been raised with senior management and psychiatric services, but no action had been taken at the time of our interview. |
Source: Victorian Auditor-General's Office based on information from an audited health service.
Figure 3D
Risk associated with failure to update Location of Interest system
|
AV uses a Locations of Interest system to indicate premises where occupational violence has been experienced previously. This alerts paramedics to the need for caution and can signal that the location is not to be entered without police attendance. It is critical for patient and worker safety that the information is complete and up to date. Staff advised that paramedics may refuse to enter a site as a result of a Location of Interest alert only to find the alert is out of date. This can compromise the outcome for the patient. Conversely paramedics may unwittingly enter a site known by police to have a high risk of violence, as a result of poor information sharing between agencies. AV recognises these issues and is currently reviewing the system. |
Source: Victorian Auditor-General's Office based on information from an audited health service.
3.8 Investigations and continuous improvement
Incident reviews and investigations are key controls for the prevention and mitigation of occupational violence incidents and are critical to continuous improvement.
All three of the audited health services and AV have policies related to the review and investigation of occupational violence incidents. While audited health services investigate some serious incidents comprehensively, those deemed less serious, mild or near misses were often inadequately investigated. This is despite the fact that many of these mild or near miss incidents—such as assaults—had the potential to cause significant harm.
3.8.1 Investigation policies, procedures and training
Audited health services and AV provide limited procedural guidance on undertaking investigations. With the exception of one audited health service, the guidance provided does not:
- step the investigator through the investigation process
- provide instruction on root cause analysis
- include better practice instruction such as highlighting the need to remain impartial, not to assign blame, interviewing in private, or examining the multiple causes contributing to an incident
- specify that corrective actions introduced in response to investigations need to be reviewed to make sure they are effective.
Similarly, none of the audited health services provide training on how to undertake an investigation, although there are some isolated examples. Recognising inadequacies in this area, AV has recently reintroduced investigation training for managers. However, this does not include better practice principles. The occupational health and safety (OHS) manager in one audited health service has provided root cause analysis training to staff. One staff member at another health service reported undertaking root cause analysis training externally.
Without investigation training, and with only limited documented guidance, those who complete investigations have limited knowledge of what is required, which may result in poor analysis and an ad hoc approach that compromises opportunities for improvement.
3.8.2 Issues associated with investigative practice
Information in the investigation field of the Victorian Health Incident Management System is poorly recorded. Minimal detail is included with fields left blank, and inadequate corrective actions recorded—such as 'discussed with staff member ways to avoid being scratched'. It is unclear whether this is because incidents are not commonly reviewed and investigated or because these actions are poorly recorded in this system. However, this lack of information in the central system undermines the comprehensiveness of the records, analysis and accountability.
Our analysis of incident data also highlighted a potential issue with the way severity ratings are assigned to occupational violence incidents. The DHHS Victorian health incident management policy guide requires that incidents are rated according to severity as determined by their degree of impact, level of care, treatment required and potential for harm, with 1 being the most severe. Analysis of OHS incident data recorded in health services' incident reporting system from January 2014 to June 2014, for all three audited health services showed that:
- large numbers of occupational violence incidents are categorised as either 'mild' —Incident Severity Rating (ISR) 3 or 'no harm/near miss'—ISR 4
- few corrective actions are identified for these incidents other than removal of patients, implementation of a behaviour management plan or support options being provided to the injured staff member.
The types of incidents classified as mild or near miss included:
- being punched in the jaw, face, chest and head
- attempted strangulation
- being kicked in the head
- being hit with object
- being slapped in the face
- sexually inappropriate conduct
- personal threat
- spitting in the eye
- a pregnant staff member being kicked in the stomach.
It appears that the health services categorised incidents based on the level of medical attention needed as a result of the injury. According to staff this is consistent with the ISR rating system. There is also provision within the guide to categorise incidents with high potential for harm as more severe. More severe incidents require more comprehensive investigation to prevent reoccurrence. It is not known why the audited health services did not identify any of the above incidents as having high potential for harm. DHHS needs to examine how the ISR rating system is being interpreted and applied to occupational violence incidents, to assess whether this is appropriate and to take action if required.
3.9 Sector-wide education, support and regulation
While DHHS and WorkSafe have implemented a range of initiatives aimed at supporting health services and AV to address occupational violence, these have not all been underpinned by appropriate and sufficient data or evidence.
The effectiveness of these initiatives is not known as neither DHHS nor WorkSafe has evaluated them. DHHS has not established agreed best practice standards for controls, with the exception of the standards for Code Grey responses.
More consistent and proactive inspection and enforcement by WorkSafe of the adequacy of health services' risk controls could also help raise the level of protection for healthcare workers.
All the audited health services and AV highlighted the critical importance of increasing community awareness of the impact of violent or aggressive behaviours on healthcare workers. They saw this issue as needing a collective response, with the system leaders—DHHS and WorkSafe—working in collaboration with health services and AV to develop appropriate messaging for members of the public to increase awareness and understanding of the issue.
3.9.1 DHHS initiatives related to occupational violence
While DHHS has an occupational violence policy and a range of resources and guides focused on occupational violence and clinical incident management more broadly, it has not assessed the usefulness of these tools. This failure to review or evaluate the uptake and effectiveness of its initiatives means that DHHS has limited evidence to demonstrate that its efforts are appropriately targeted, meeting the highest priorities and are effective, relative to other possible approaches.
While DHHS has used the recommendations provided by The Victorian Taskforce on Violence in Nursing report and the 2011 Inquiry to guide its occupational violence initiatives, these have not been undertaken in a timely way. The Inquiry had 11 recommendations directed toward DHHS that relate to this audit. Of these, DHHS advised VAGO that they had fully delivered nine with the remaining two partially completed or underway. Our review found that DHHS has fully delivered only five of the recommended actions, with the remaining four partially completed or underway and two not fulfilled. This is a poor outcome given that it has been three years since the Inquiry made its recommendations.
A sample of initiatives and resource guides implemented by DHHS includes:
- the 2007 Preventing occupational violence in Victorian health services: A policy framework and resource kit, which was updated in 2011 and renamed Preventing occupational violence: A policy framework including principles for managing weapons in Victorian health services
- Better responses, safer hospitals: Standards for Code Grey responses, released in mid-2014
- funding to improve security systems, including installation of effective duress alarms and closed circuit TV throughout emergency departments
- funding for minor capital works to improve staff safety and patient satisfaction through access control systems, improved waiting room and triage area design, and secure entrances and exits
- Occupational violence incident response: managing incidents in public health services, 2013
- Deter, detect and manage: A guide to better management of weapons in health services, 2009
- High-impact interventions for occupational violence: Building better partnerships between police and health services, 2012.
DHHS has also developed other resources to inform the management of clinical incidents, which it advises are applicable to, and used in, the management of OHS and occupational violence—such as the 2011 Victorian health incident management policy, the 2008 Victorian Health Incident Management System (VHIMS): data set specification, the 2003 Occupational Health and Safety Management Framework Model, and the 2013 Incident reporting instruction.
DHHS' policies and guides provide insufficient guidance about how to review or investigate occupational violence incidents. This is a serious inadequacy given the importance of investigation to the continuous improvement cycle and to managing occupational violence risk. As recommended in Part 2, DHHS needs to provide increased, specifically targeted guidance related to occupational violence incident reporting and investigation requirements.
While DHHS has provided a number of publicly-available progress reports on its initiatives, its approach to implementation has been uncoordinated, fragmented and unaccountable. There is no dedicated project team or unit within DHHS with responsibility for these activities as occupational violence is an issue that crosses a number of divisions within DHHS. There is a risk that this approach limits DHHS' capacity to provide a strategic, coherent and accountable response to the issue.
3.9.2 WorkSafe educational support
WorkSafe has also produced a range of guides and educational materials to support health services to better manage the risk of occupational violence, including the 2014 A guide for employers: Preventing and responding to work-related violence and its 2008 A handbook for workplaces: Prevention and management of aggression in health services—reviewed in 2010.
In 2014, in response to recommendations from VAGO's 2013 Occupational Health and Safety Risk in Public Hospitals audit, WorkSafe began a project aimed at raising the awareness of health service boards about their responsibilities in relation to OHS.
WorkSafe has undertaken some reviews of its guidance and projects, although it has not evaluated their effectiveness. Worksafe has recently developed a research strategy that will direct evaluation of its programs through its research partnership with the Institute of Safety Compensation and Recovery Research.
WorkSafe has not been systematic or consistent in its work on occupational violence and has undertaken relatively few projects focused on it. WorkSafe acknowledges this limitation and through its 2014 review of its Health and Safety Risk Based Strategic Framework has identified that occupational violence in health services needs to be a higher priority in the future.
Key factors that informed this decision were WorkSafe's recognition of its insufficient and intermittent focus on this area in the past, an increase in drug-related behavioural issues in the community, and intense public focus and concern. This re‑prioritisation is a positive step that more fully reflects the reality that the true prevalence of occupational violence is unknown—with injury or harm resulting from occupational violence un-reported and the potential for serious injury or harm largely unacknowledged. No agency is in a position to be assured that they are effectively managing the risk and protecting staff. This is a situation in which strong sector-wide leadership from the regulator is needed.
In response to VAGO's 2013 OHS audit, DHHS and WorkSafe have initiated several collaborative projects. These are still in the early stages and so are not able to be assessed but they are a positive development:
- An OHS Governance Group has been developed. It will be a forum for discussion of OHS issues that will formalise collaboration between DHHS, WorkSafe and health services.
- WorkSafe has agreed to issue annual results of inspections and an annual report on the top five OHS risks for public health services to DHHS from April 2015.
- DHHS and WorkSafe are currently exploring the feasibility of a joint Health Services Industry Data and Collaboration Initiative—there is in-principle agreement between DHHS and WorkSafe on a shared approach to the collection and analysis of health services incident data.
3.9.3 WorkSafe inspection and enforcement
It is questionable whether WorkSafe is using its powers sufficiently to inspect or investigate and prosecute health services compliance with, or breaches of, the Occupational Health and Safety Act 2004 in relation to occupational violence. WorkSafe inspection of health services in relation to occupational violence is limited and WorkSafe rarely uses the enforcement mechanisms available to it, advising us that it focuses more on its education activities. However these are also not extensive.
WorkSafe inspections and enforcement activities related to occupational violence between 2009 and 2014 included:
- visiting 134 health service sites where occupational violence issues were raised
- between 20 and 32 inspection visits per year
- issuing 16 improvement notices
- undertaking two comprehensive investigations of occupational violence matters—in 2010 and 2013—which were requested by members of the public.
WorkSafe advised that its compliance and enforcement activities in relation to occupational violence have been limited for various reasons:
- WorkSafe has finite resources and must direct them to the highest risks, given its responsibility for all workplaces across Victoria. Using its evidence base of claims data, WorkSafe had, until 2014, assessed occupational violence in health services as less prevalent than other risks in other industries.
- Investigations in relation to occupational violence, as with all Occupational Health and Safety Act 2004 investigations, require proof that the employer did not take all reasonably practicable steps to provide and maintain a working environment that was safe and without risks to health. WorkSafe has advised the audit team that in the cases of occupational violence it investigated, employers had taken all reasonably practicable steps to provide and maintain a safe working environment.
- Causes of occupational violence are often multi-faceted and difficult to conclusively isolate.
While recognising the difficulties associated with successful enforcement in relation to occupational violence incidents, we have not gained assurance that WorkSafe is using investigations sufficiently as a tool to drive organisational improvement. WorkSafe should, for example, be assessing the quality of a health service's investigation of serious incidents and their subsequent actions to prevent or manage future occurrences. WorkSafe advises that its orientation program for new inspectors will include training in supporting employers in dealing with occupational violence issues. This additional training and support would be valuable, however, it is concerning that this gap has not been addressed earlier. WorkSafe's handbook for workplaces provides an audit tool that could be further built on for use by inspectors.
WorkSafe can provide leadership through increased inspections and greater use of investigations and prosecution where appropriate. Given the limitations of health services' current investigation and control improvement practices, WorkSafe should also use its inspection role to assess these investigations and control improvements that health services implement as a result of serious occupational violence incidents.
Recommendations
- That health services and Ambulance Victoria regularly review and evaluate the effectiveness of their controls to prevent and reduce occupational violence.
- That health services and Ambulance Victoria build on, or develop a comprehensive and tiered occupational violence training program, that is tailored to need, delivered as a refresher on a regular basis, delivered flexibly, and reviewed for effectiveness.
- That health services develop, and Ambulance Victoria enhances existing, investigation training and procedures—including root cause analysis—and undertake compliance monitoring in relation to investigative practices.
- That the Department of Health & Human Services reviews its guidance material on occupational violence and evaluates its uptake and usefulness, including gaps in information.
- That the Department of Health & Human Services in collaboration with health services and Ambulance Victoria develops a set of core occupational violence training tools that can be adapted by health services to their local context as required.
- That the Department of Health & Human Services and WorkSafe work with health services and Ambulance Victoria to develop appropriate public messaging to improve community awareness of the impact of occupational violence on healthcare workers and highlight the need for appropriate and respectful behaviour when seeking medical treatment.
- That WorkSafe more proactively uses its full range of tools—including inspections—to assess occupational violence risks and the effectiveness of controls in health services and Ambulance Victoria.
4 Supporting post-incident return to work
At a glance
Background
Under the Workplace Injury Rehabilitation and Compensation Act 2013, health services and Ambulance Victoria (AV), as employers, are required to provide suitable systems for the effective rehabilitation, determination of claims and compensation, and return to work (RTW) of injured workers. WorkSafe, as the occupational health and safety regulator, has a critical role in facilitating workers' RTW, including providing guidance, implementing strategies and enforcing compliance with legislation.
Conclusion
The three audited health services and AV support healthcare workers to get back into the workforce after occupational violence incidents.
WorkSafe effectively supports RTW, and monitors and enforces employers' compliance with relevant legislation.
Findings
- Health services and AV have appropriate processes in place to manage workplace injuries, including RTW coordinators and RTW plans.
- WorkSafe uses a range of services, initiatives and strategies to promote continued improvement in RTW rates, and fulfils its legislative responsibilities to assist healthcare workers after occupational violence incidents.
- WorkSafe evaluates its RTW activities through a range of mechanisms, which indicate it has been effective in managing RTW.
4.1 Introduction
Employees injured as a result of work—including occupational violence incidents—are entitled to compensation, including payment of wages and/or reasonable medical and other expenses. Under the Workplace Injury Rehabilitation and Compensation Act 2013 (the Act), health services and Ambulance Victoria (AV), as employers, are required to provide suitable systems for the effective rehabilitation determination of claims and compensation, and return to work (RTW) of injured workers. This includes making sure injured workers can safely remain at work, return to their pre-injury role, and take up modified duties at the earliest opportunity, consistent with medical advice.
WorkSafe, as the occupational health and safety regulator, has a critical role in promoting continued improvement in RTW rates through its policies and practices. This is underpinned by a legislative framework that places obligations on employers and workers, which is monitored and enforced by WorkSafe.
4.2 Conclusion
The three audited health services and AV adequately support healthcare workers to get back into the workforce after absences due to occupational violence incidents. Employment assistance programs are readily available and AV has an effective peer support program.
WorkSafe has improved RTW rates through its policies and practices, and effectively monitors and enforces employers' compliance with relevant legislation.
4.3 Legislative functions
Key functions under the Act relating to RTW for health services, AV and WorkSafe are shown in Figure 4A.
Figure 4A
Key functions under the Act related to return to work
|
Agency |
Key roles and responsibilities |
|---|---|
|
Health services and AV |
|
|
WorkSafe |
|
Source: Victorian Auditor-General's Office from the Workplace Injury Rehabilitation and Compensation Act 2013.
4.4 Effectiveness of return to work processes
4.4.1 Supporting injured workers
The three audited health services and AV have policies and procedures setting out how to support injured workers—including those related to occupational violence incidents—to remain at work or RTW as soon as it is safely possible. They each have RTW coordinators who prepare a RTW plan and liaise with all the relevant parties. RTW plans were prepared for the 20 WorkCover claims we examined. Interviews with staff members who had undertaken the RTW process identified high satisfaction with the process and outcomes.
Employment assistance programs are readily available at the health services and AV has an effective peer support program. AV's peer support program is available 24 hours a day, seven days a week for employees who are in distress and require immediate or urgent assistance. Interviews with staff who had returned to work after an occupational violence injury reported that the peer support program had provided effective support. Recent surveys of staff who have received this service also indicate high satisfaction.
It is important for health services and AV to manage RTW effectively after occupational violence incidents because the length of absence from work not only negatively affects the worker—it is known that the more time lost the more difficult it is to return—but it also has an impact on claim costs. The premiums that employers pay to WorkSafe are influenced by their claim's performance rating relative to other employers operating within the same industry. An employer's RTW rate is the main factor affecting calculations used by WorkSafe to estimate premium levels.
WorkCover claims relating to occupational violence can often include psychological and back injuries, which may result in longer absences from work. One audited health service has identified this and taken action to reduce this risk through escalating the issue to its board and implementing various initiatives. Figure 4B shows how this health service used WorkCover claims data to drive this improvement.
Figure 4B
Health service response to increase in occupational violence WorkCover claims
|
Based on data that showed a 10-fold increase to the cost of premiums as a result of seven WorkCover claims—from $51 000 to $500 000 over a three-year period—one audited health service increased the risk rating of occupational violence on its organisational risk register from medium to high. This led to greater management oversight and more resources being allocated to controls. This health service has also introduced a designated occupational violence role and has commenced introduction of an occupational violence and aggression training program. |
Source: Victorian Auditor-General's Office based on information from an audited health service.
An example of an injured worker successfully returning to work at one of the audited health services is shown in Figure 4C.
Figure 4C
Return to work case study
|
After being assaulted by a patient, an acting nurse unit manager attended the emergency department for treatment. The nurse was supported by senior managers, including receiving follow-up phone calls when she went home. The nurse submitted a WorkCover claim and trauma counselling was provided by the health service. The incident was also reported to the police. The nurse was absent from work for almost two weeks and was provided with alternative duties before gradually moving back to her original role. Prior to the assault, the nurse had observed a number of occupational violence incidents. The accumulated stress of this exposure had manifested in a high level of anxiety for the nurse while performing her duties. When this was identified by senior staff, the nurse was offered an alternative temporary non-clinical role. The nurse reported that the RTW process had been a positive experience and that she felt well supported by the health service. |
Note: Based on a real incident with identifying details omitted to maintain confidentiality.
Source: Victorian Auditor-General's Office based on information from an audited health service.
AV has quarterly and annual RTW targets of 76 per cent of staff returning to work after three months. It uses these targets to monitor all WorkCover claims—including those involving occupational violence. The targets have been in place since 2011–12 and while quarterly targets are not always met, annual targets have consistently been met.
4.4.2 WorkSafe
WorkSafe fulfils its legislative responsibilities to assist healthcare workers to RTW after occupational violence incidents. RTW is one of WorkSafe's strategic priorities and a key organisational performance indicator. The economic viability of the RTW scheme is dependent on WorkSafe's ability to keep the cost of premiums contained. WorkSafe supports RTW—including claims involving occupational violence incidents—by:
- setting policy and overseeing the performance of insurance agents
- providing specialist support staff in occupational rehabilitation
- supporting employers with resource guides and through RTW inspectors
- offering an advisory service for stakeholders
- disseminating relevant messages through television campaigns
- using an expert group of industry representatives to provide comment on emerging issues and feedback from members, and to identify trends.
WorkSafe data indicates the RTW system, in relation to occupational violence WorkCover claims, is working effectively. The RTW rate for healthcare workers affected by occupational violence is considerably stronger than workers affected by occupational violence in other occupations—92.17 per cent compared to 85.93 per cent for all occupations.
Worksafe evaluates its RTW activities—including those related to occupational violence—through a range of mechanisms, which indicate effectiveness in managing RTW. These include:
- participation in Safe Work Australia's National RTW biennial survey to measure RTW outcomes and better understand the factors that may affect injured workers' RTW—in the 2013–14 survey, Victoria registered a RTW rate of 75 per cent, which compares well with other jurisdictions.
- comparative study of RTW impacts—to investigate the impact of compensation system policies on RTW outcomes in Australian and selected international jurisdictions, with the aim of improving RTW performance.
Appendix A. Audit Act 1994 section 16 — submissions and comments
Introduction
In accordance with section 16(3) of the Audit Act 1994, a copy of this report, or part of this report, was provided to WorkSafe, the Department of Health & Human Services, Ambulance Victoria and the three audited health services.
The submissions and comments provided are not subject to audit nor the evidentiary standards required to reach an audit conclusion. Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
RESPONSE provided by the Acting Chief Executive, WorkSafe

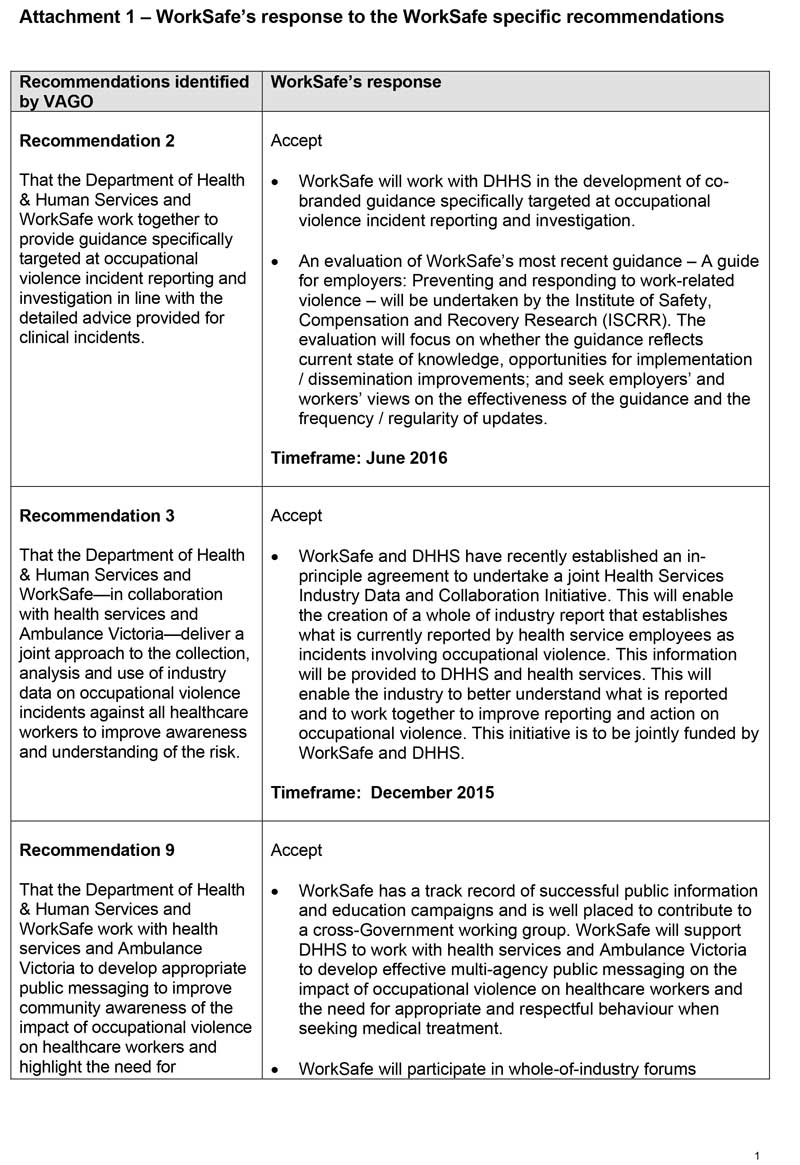
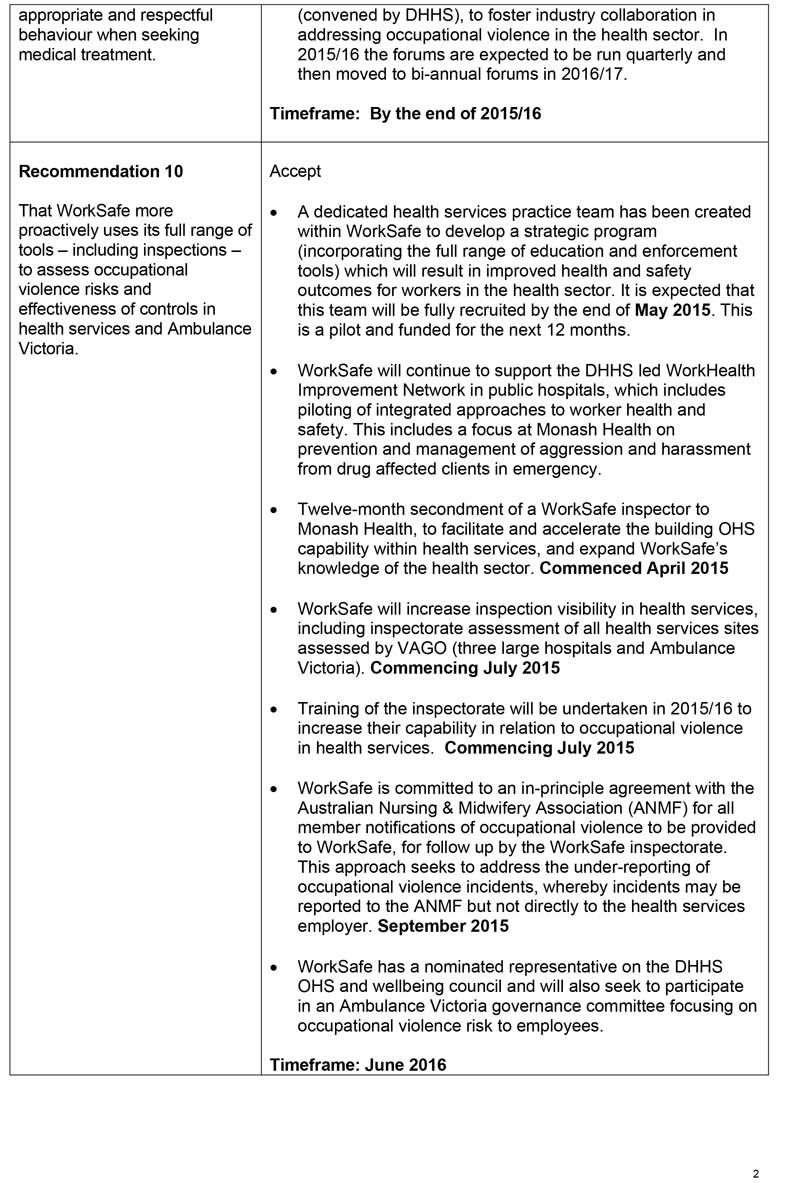
RESPONSE provided by the Secretary, Department of Health & Human Services
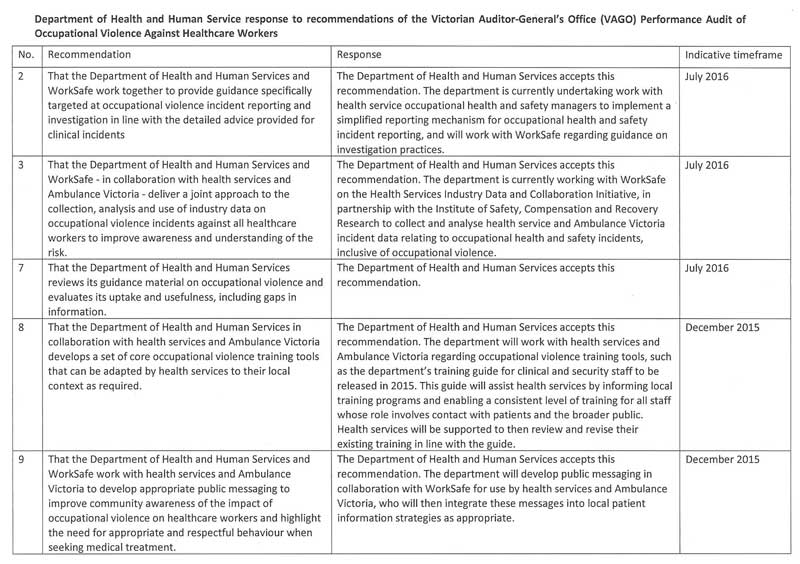
RESPONSE provided by the Administrator, Ambulance Victoria