Access to Mental Health Services
Overview
Nearly half (45 per cent) of Victorians will experience mental illness in their lifetime. Annually, one in five Victorians, or 1.2 million, suffer from a mental illness. Mental illness affects not only an individual's wellbeing and quality of life, but also their physical health and engagement in employment, education and community. Mental illness also has flow-on effects to the human services, general health and justice systems.
This audit determined if people with a mental illness have timely access to appropriate treatment and support services. We examined how the Department of Health and Human Services (DHHS) oversees the mental health system and whether it promotes increased accessibility. We examined DHHS's mental health policies, strategies and plans, the data it collects, and how this informs planning for funding, infrastructure and the workforce.
Transmittal letter
Independent assurance report to Parliament
Ordered to be published
VICTORIAN GOVERNMENT PRINTER March 2019
PP No 19, Session 2018–19
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report Access to Mental Health Services.
Yours faithfully
Andrew Greaves
Auditor-General
21 March 2019
Acronyms
| AMHS | area mental health service |
| AIHW | Australian Institute of Health and Welfare |
| CCU | community care unit |
| CMI/ODS | Client Management Interface/Operational Data Store |
| DHHS | Department of Health and Human Services |
| ED | emergency department |
| LOS | length of stay |
| KPI | key performance indicator |
| MHCSS | Mental Health Community Support Services |
| MHET | Mental Health Expert Taskforce |
| MHNIP | Mental Health Nurse Incentive Program |
| PHN | primary health network |
| NDIS | National Disability Insurance Scheme |
| PAPU | psychiatric assessment and planning unit |
| PARC | prevention and recovery care |
| PBS | Pharmaceutical Benefits Scheme |
| SECU | secure extended care unit |
| SoP | statements of priorities |
| VAGO | Victorian Auditor-General's Office |
Audit overview
One objective of the Health Services Act 1988 is to 'ensure that an adequate range of essential health services is available to all persons resident in Victoria, irrespective of where they live or whatever their social or economic status'. Mental health care is one such service.
Mental illness affects not only an individual's wellbeing and quality of life, but also their physical health and engagement in employment, education and community; with flow-on effects to the human services, general health and justice systems.
With 45 per cent of the Victorian population experiencing mental illness in their lifetime, ensuring access to mental health care is vital to supporting a healthy and productive Victorian population. The demand for mental health care is growing, driven by multiple factors—including population growth, a reduction in stigma around seeking help, changes in legal and illegal drug use patterns, and increasing levels of social isolation in our community.
In 2009 the imminent gap in meeting demand for mental health services was forecast in the previous decade-long mental health plan titled Because mental health matters: Victorian Mental Health Reform Strategy 2009–2019, which stated that:
Action is needed not only to address the current needs of the Victorian population but to plan for the projected numbers of people likely to be seeking help for mental health problems in ten years' time.
In 2015, the Department of Health and Human Services (DHHS), the agency responsible for managing Victoria's public mental health system, acknowledged in Victoria's 10-year mental health plan (10-year plan), that:
...increasing and sustained demand pressure on services has not been matched with increasing resources. Shifting population and growth has left some services under even greater pressure. The result is longer waiting times to access services and higher thresholds for entry. The increased pressure on services creates a risk that people may receive treatment that is less timely, less intensive and shorter in duration than they want or need.
Given this acknowledgement, in this audit we assessed whether DHHS's current 10-year plan and supporting activities have started to address known access problems. Our audit objective was 'to determine if people with mental illness have timely access to appropriate treatment and support services'.
Conclusion
DHHS has done too little to address the imbalance between demand for, and supply of, mental health services in Victoria.
The lack of sufficient and appropriate system-level planning, investment, and monitoring over many years means the mental health system in Victoria lags significantly behind other jurisdictions in the available funding and infrastructure, and the percentage of the population supported.
While DHHS understands the extent of the problem well and has been informed by multiple external reviews, the 10-year plan outlines few actions that demonstrate how DHHS will address the demand challenge that the 10-year plan articulates:
- there are no clear targets or measures to monitor progress in improving access
- there are no forward plans for the capital infrastructure needed
- the workforce strategy does not address the particular issues in regional and rural areas and fails to articulate specific targets
- there is no work to address barriers to access created by geographic catchment areas.
DHHS has made little progress closing the significant gap between area mental health services' (AMHS) costs and the price they are paid by DHHS to deliver mental health services; and in addressing historical inequities in funding allocations that do not align to current populations and demographics. This means many people wait too long or miss out altogether on services, and for those that do receive services, their clinical care can be compromised by the need to move them quickly through the system.
Real progress is unlikely within the life of the plan unless DHHS accelerates and directs effort towards the fundamentals: funding, workforce and capital infrastructure. Until the system has the capacity to operate in more than just crisis mode, DHHS cannot expect to be able to make meaningful improvements to clinical care models or the mental health of the Victorian population.
The Royal Commission into Mental Health will undoubtedly highlight many areas for improvement across the system. However, the need for planning and investment to meet demand is already known and as such work to address this should not await the Commission's recommendations. Further delay will only amplify the problems the Commission seeks to address.
Findings
Victoria's 10-year mental health plan
Developing and implementing the 10-year plan
DHHS developed the 10-year plan through thorough sector and consumer consultation. The Mental Health Expert Taskforce (MHET) oversaw implementation. The group consisted of expert representatives from service providers, peak bodies, consumer groups, and academia.
Health services consistently raised that difficulty accessing services and coping with demand was a challenge. The 10-year plan reflects this and stresses the issue of 'higher demand and unmet need'. One of the 10-year plan's four focus areas is 'the service system is accessible, flexible and responsive to people of all ages, their families and carers and the workforce is supported to deliver this'.
However, little within the 10-year plan directly addresses improving access. It talks largely about the way services should be designed and delivered, such as through co-production with consumers, focusing on early intervention, integrating services, and implementing evidence-based practice. The AMHSs we audited expressed their disappointment in the plan because it is generic and lacks clear actions to address the demand and supply imbalance.
A role of the MHET was to inform 'waves of reform'—areas for DHHS to prioritise. The priority reform areas do not adequately reflect the underlying issue of lack of system capacity. Of the nine priority areas for the first two waves of reform, only two clearly relate to improving access; the development of a workforce strategy, and an action around 'managing clinical demand'. As such, while focusing action on useful activities—such as the development of frameworks for suicide prevention and supporting Aboriginal mental health, forensic service planning, and setting outcome measures—DHHS has made almost no progress in addressing the supply and demand imbalance.
DHHS has completed and released its workforce strategy, and through the 2018–19 budget secured funding for some new mental health workers. However, the workforce strategy does not include targets for the types or numbers of workers it aims to attract or retain and does not set action to address the significantly greater staffing challenges that regional and rural areas face. Further, the strategy is not integrated with service or infrastructure planning.
DHHS also completed a draft Clinical mental health services action plan 2018–2023, which better addresses the need of AMHSs and stakeholders to understand DHHS's direction in improving supply and access. The action plan informed DHHS's 2018–19 budget bid for mental health services, which secured growth funding for the sector. However, despite the investment of three-years' work in the plan, DHHS does not intend to release it publicly, which misses an opportunity to communicate DHHS's work in this area to the sector and stakeholders, and for stakeholders to hold DHHS to account for completing the work the action plan outlines.
Monitoring and reporting on progress
Other functions of the MHET were to develop a work program and advise the Minister for Mental Health on performance measures and targets. The MHET, though it considered and advised on progress indicators, did not develop a clear work program of actions, timeframes, or targets and subsequently neither the MHET nor DHHS have monitored plan progress against any agreed deliverables.
The MHET was disbanded in February 2018 as intended. The 10-year plan progress oversight now sits with the DHHS mental health branch. The mental health branch has reported only once to the DHHS Executive Board via the Health Reform Sub Committee—on the draft Clinical mental health services action plan 2018–2023. The lack of timely internal progress reporting significantly reduces accountability for achievement against the 10-year plan.
There are few measures in the outcomes framework for the 10-year plan that directly capture performance against providing access to services or increasing service reach—this is despite the acknowledged performance problems in this area—which shows a lack of focus on the most pressing issue the system faces.
Understanding and meeting demand
As system manager, DHHS has a responsibility to ensure service access by supporting the foundations of the system: funding, capital infrastructure and service distribution, and understanding demand and system performance to guide proper investment. In each of these areas, DHHS has done too little and now requires significant, prompt action if it is to make real progress against the 10-year plan.
Funding
Australian Institute of Health and Welfare (AIHW) data shows that between 2011–12 and 2015–16 national recurrent expenditure per capita on specialised mental health services grew an average of 0.7 per cent annually, while over that time in Victoria it declined by 0.3 per cent annually. In 2015–16, Victoria's per capita recurrent expenditure was $197.30, the lowest in Australia, with a national average of $226.52.
AMHSs advise that the allocation of growth funding over the last three state budgets has been partially directed to closing the existing gap between their service costs and the price DHHS pays, therefore AMHSs are not fully providing additional services. DHHS is aware of the price gap. A DHHS-commissioned review showed that DHHS pays 65 per cent of AMHS bed costs compared with more than 80 per cent of costs for general health beds.
DHHS has commenced funding reform, funding 'packages of care' to incentivise AMHSs to provide more community-based treatment services. However, without an adequate quantum of funding, the intended outcome is at risk.
DHHS's advice to government states that the new funding reform and four-year growth funding from 2018–19:
- provides each new community-based client with a maximum of six hours treatment per annum—the nationally recommended level is 72 hours
- enables DHHS to provide mental health services to 1.2 per cent of the population—a marginal improvement on the current 1.16 per cent—compared to the estimated 3.1 per cent of the Victorian population with a severe mental illness
- increases the price paid to only 67 per cent of AMHSs' costs.
DHHS also advises that the budget provides additional services for the most unwell patients, to be achieved within five years, but has not quantified this additional service provision.
DHHS has also moved bed funding to a slightly higher single price for all beds regardless of location or severity of illness, with the aim to begin addressing historical funding inequities. However, this does not account for the inherently higher operating costs that rural AMHSs face.
Planning to meet demand
Increasing demand combined with current service shortfalls are placing the whole mental health service under substantial stress. In 2017, DHHS commissioned an external review of the mental health system and the resultant report, Design, Service and Infrastructure Planning Framework for Victoria's Clinical Mental Health System: Developing excellence in clinical mental health care for Victoria (Design, Service and Infrastructure Planning Framework for Victoria's Clinical Mental Health System), highlights that:
- emergency department (ED) presentations have increased 9 per cent from 2015–16
- acute hospital admissions have grown at an annual rate of 2.4 per cent
- length of stay (LOS) in hospital trends down from 14.7 days to 11.2 days from 2009 to 2017 (with LOS stay in 2017–18 at 9.6 days)
- unplanned readmission rates for adult mental health patients at 14.4 per cent in 2017–18
- community mental health contacts per 1 000 people declining at a rate of 2.5 per cent per annum over the last 10 years.
These demand pressures have lifted the thresholds for access to services so that AMHSs only see the most unwell, which creates a flow on effect. AIHW reports the number of Victorian mental health patients that accessed acute services through police, ambulance and self-presentations to hospital EDs increased from 28 757 in 2004–05 to 54 114 in 2016–17.
To understand and respond to demand and access issues, DHHS needs data to reflect current service capacity and to calculate unmet demand. While it has developed a model to forecast service demand, it relies largely on historical activity data, which creates significant limitations to its use. DHHS is missing available information to understand unmet demand. It does not collate, assess and input to its forecasting model:
- data from mental health triage services to identify the number of people who contact triage but are not provided access to services
- people accessing services that are not registered with an AMHS.
Given DHHS acknowledges there is significant unmet demand, estimating this demand is critical to inform any future planning for the mental health system.
Capital infrastructure
Victoria has one of the lowest mental health bed bases nationally. As a result, all major acute psychiatric units continually operate at or above 95 per cent capacity—well above desirable levels of 80 to 85 per cent that would permit AMHSs to admit acutely ill patients as needed. A review commissioned by DHHS advised that Victoria's bed base needs to grow by 80 per cent over the next decade to reach levels of service provision of other Australian jurisdictions.
There are 53 new acute adult beds funded in 2018–19, with 21 now open and 34 in planning. There are also 24 sub-acute beds in the planning phase, and 10 mother and baby unit beds will operate seven rather than five days a week. While helpful, the additional beds will not meet the unmet demand nor shift Victoria towards the recommended bed numbers.
There are no further new beds in the capital pipeline, and while DHHS aims to complete a 'Detailed services and infrastructure plan for Victoria's clinical mental health system over the next 20 years' it will likely take DHHS some time to complete the plan; secure and allocate funding; and then plan and build infrastructure. DHHS should anticipate that Victorians with mental health issues will continue to face barriers accessing mental health beds across the remaining life of the 10-year plan, and that this will impact the effectiveness of any changes to funding or the service delivery model.
Catchment areas
Clinical mental health services are provided in geographic catchment areas that were established in the 1990s. The consumer's place of residence determines which service or services they can access, which causes practical problems that hinder service access:
- the catchment areas are not aligned with other health and human service areas, or local government area boundaries, which makes service coordination difficult
- the geographic catchments do not align with age-based service groupings
- there is a lack of coordination between catchment areas when patients need to access services across catchment borders
- there is misalignment between service levels and types within a catchment and population growth and demographic changes in that area.
Despite understanding these issues for many years, and commissioning work to examine them and make recommendations, DHHS has taken no action to address them.
Figure A
Key numbers about the Victorian mental health system
Source: VAGO.
Recommendations
We recommend that the Department of Health and Human Services:
1. complete a thorough system map that documents its capacity, including capital and workforce infrastructure, geographical spread of services, and estimated current and future demand, including current unmet demand
2. use this map to inform a detailed, public, statewide investment plan that integrates service, capital and workforce planning; setting out deliverables and time frames
3. set relevant access measures with targets, which reflect the intended outcomes of the investment plan, and routinely report on these internally and to the public
4. undertake a price and funding review for mental health services, which includes assessing funding equity across area mental health services, and provide detailed advice to the Minister for Mental Health on the results and use this information to inform funding reforms
5. resolve the known catchment area issues of misaligned boundaries that prevent people from accessing services
6. re-establish routine internal governance and reporting against mental health system priorities, activities and performance that ensures senior executive level oversight and accountability.
Responses to recommendations
We have consulted with the DHHS, Bendigo Health, Melbourne Health, Monash Health, Latrobe Regional Hospital, Peninsula Health, and South West Healthcare and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report to those agencies and asked for their submissions or comments. We also provided a copy of the report to the Department of Premier and Cabinet.
DHHS provided a response. The following is a summary of its response. The full response is included in Appendix A.
DHHS accepted each of the six recommendations, with two accepted in‑principle pending the outcomes of the Royal Commission into Mental Health. The department will undertake statewide mapping and assessment of current and future demand, develop a performance and accountability framework for mental health services, undertake a price review of clinical mental health services, and re-establish the MHET.
1 Audit context
1.1 Overview of Victoria's mental health services system
Nearly half (45 per cent) of Victorians will experience mental illness in their lifetime. Annually, one in five Victorians, or 1.2 million, suffer from a mental illness1. Of these 1.2 million people, based on 2017 population figures:
- 11 per cent will experience mild mental illness (670 000)
- 6 per cent will experience moderate mental illness (346 000)
- 3 per cent will experience severe mental illness (184 000).
The Victorian Government funds public mental health services covering clinical assessment, treatment, and case management in community and inpatient settings as Figure 1A shows.
A number of publicly funded specialist clinical mental health services are also delivered on a statewide basis, such as mother and baby services, eating disorder services, and forensic mental health services.
1.2 Agency roles and responsibilities
The Department of Health and Human Services
In relation to mental health services, DHHS is responsible for:
- funding
- developing policies and plans
- encouraging safety and quality of care
- monitoring and reviewing service provision
- developing performance measures to enable service comparison
- collecting and analysing data to support these functions.
These functions are undertaken by the mental health branch and other business units within DHHS.
Figure 1A
Organisation of mental health services
Note: CCU = community care unit, SECU = secure extended care unit, HDU = high dependency unit, PARC = prevention and recovery care, PAPU = psychiatric assessment and planning unit, MHCSS = Mental Health Community Support Services, PHN = primary health network, ATAPS = Access to Allied Psychological Services, MHNIP = Mental Health Nurse Incentive Program, MBS = Medicare Benefits Schedule, PBS = Pharmaceutical Benefits Scheme.
Note: Services such as CCU, SECU and PAPU are described further in the next section.
Source: VAGO, based on Design, Service and Infrastructure Planning Framework for Victoria's Clinical Mental Health System, DHHS, 2017.
DHHS's 2018–19 mental health services budget was $1 605.7 million, or 6.4 per cent of its total budget. DHHS distributes the funding as set out in its annual policy and funding guidelines and annual statements of priorities (SoP)—the key accountability agreements between the government and health service providers. SoPs outline expected services and activity levels, performance measures and targets, and policy directions and requirements. DHHS monitors health services' performance against their SoP.
DHHS groups Victoria's clinical mental health services into age and regional cohorts. Aged-based service groupings are: child and adolescent mental health services (0–18 years), adult mental health services (16–64 years), and mental health services for older people (65+ years). Geographically, DHHS arranges services within catchments. The consumer's place of residence determines which service(s) they can access. The current range of services provided throughout Victoria includes:
- 13 child and adolescent mental health services, provided in five metropolitan and eight rural catchments
- 21 adult mental health services, provided in 13 metropolitan and eight rural catchments
- 17 aged persons mental health services provided in nine metropolitan and eight rural catchments.
Area mental health services
AMHSs provide a range of clinical mental health assessment and treatment services, and are managed by general health facilities such as hospitals. This audit focuses on the mental health services provided through these general health facilities—including:
- acute community intervention services (ACIS)—urgent response service providing telephone triage, community outreach, and support to EDs
- acute inpatient services—bed-based care for people acutely unwell, often provided within general hospitals
- community care units (CCU)—clinical care and rehabilitation in a home-like environment
- secure extended care units (SECU)—inpatient treatment and rehabilitation for people with unremitting and severe mental illness
- prevention and recovery care (PARC) services—short-term residential treatment services with a recovery focus
- psychiatric assessment and planning units (PAPU)—short-term (up to 72 hours) specialist psychiatric assessment and treatment for people experiencing an acute episode of mental illness
- clinical mental health services delivered in the community.
Figure 1B shows where the AMHSs are located across Victoria.
Figure 1B
Spread of AMHSs across Victoria against local government area boundaries
Regional and rural services
Metropolitan services
Source: Victoria's Clinical Mental Health System Plan, DHHS, 2016.
1.3 Relevant legislation and policies
Mental Health Act 2014
The Mental Health Act 2014 (the Act) provides a legislative framework for the assessment of Victorians who appear to have a mental illness, and for the treatment of people with mental illness. The Act requires that people receive assessment and treatment with as few restrictions on human rights and dignity as possible. The Act has core principles and objectives, including:
- assessment and treatment is provided in the least intrusive and restrictive way
- people are supported to make and participate in decisions about their assessment, treatment and recovery
- individuals' rights, dignity and autonomy are protected and promoted at all times
- priority is given to holistic care and support options that are responsive to individual needs
- the wellbeing and safety of children and young people is protected and prioritised
- carers are recognised and supported in decisions about treatment and care.
Policies
Several policies enable the provision of services to respond to the intent of the Act.
Victoria's 10-year mental health plan
DHHS published the 10-year plan in November 2015 in response to government election commitments. It is a long-term plan that sets the mental health agenda for the next decade that is intentionally ambitious, and outcome focused. The 10-year plan's goal is that all Victorians experience their best possible health, including mental health. The 10-year plan is not designed to document all the activities and initiatives needed to address the issues in the mental health system, but it aims to give strategic direction in mental health policy, funding and program development.
Victorian Government Suicide Prevention Framework 2016–25
The Victorian Government Suicide Prevention Framework 2016–25 aims to halve Victoria's suicide rate by 2025 and supports the Commonwealth's Fifth National Mental Health and Suicide Prevention Plan (the Fifth Plan).
Balit Murrup: Aboriginal social emotional wellbeing framework 2017–2027
Balit murrup, meaning 'strong spirit' in the Woi-wurrung language, aims to reduce the health gap attributed to suicide, mental illness and psychological distress between Aboriginal Victorians and the general population. The framework sets out principles, strategic priorities and new investments to achieve this. In relation to access, one of four 'domains' included in the framework is 'improving access to culturally responsive services', with priorities for more Aboriginal people to engage in appropriate treatment and care, and for those services to be culturally safe and free from racism.
1.4 Why this audit is important
Mental health is an integral part of a person's capacity to lead a fulfilling life, including the ability to form and maintain relationships, to study, work, pursue recreational interests, and to be able to make a positive contribution to society by making day-to-day decisions about education, employment, housing or other choices.
Disturbances to a person's mental wellbeing can negatively impact their capacity and the choices they make, leading not only to diminished functioning at the individual level but also to broader societal and welfare losses. There is significant flow on effect to other services if the mental health system is not functioning well, such as housing, justice and other health and community services.
Victoria's mental health system faces significant challenges and the 10-year plan is intended to set a pathway to address them. As DHHS is currently three years into this plan, it is timely to assess its progress in meeting one of the key challenges to the system: providing timely access to services in the face of increasing demand.
1.5 What this audit examined and how
Our audit objective was to determine if people with mental illness have timely access to appropriate treatment and support services.
DHHS and the broader mental health sector notes that Victorians with a mental illness do not have timely access to appropriate treatment and support services as expressed in the 10-year plan. For this reason, our audit focused on analysing whether the 10-year plan and supporting activities will start to address the existing access problem.
We examined how DHHS oversees the mental health system and whether it promotes increased accessibility. We examined DHHS's mental health policies, strategies and plans, the data it collects, and how this informs planning.
Alongside DHHS, we gathered evidence from six health services:
- Bendigo Health
- Melbourne Health
- Monash Health
- Latrobe Regional Hospital
- Peninsula Health
- South West Healthcare.
Pursuant to section 20(3) of the Audit Act 1994, unless otherwise indicated, any persons named in this report are not the subject of adverse comment or opinion.
We conducted our audit in accordance with Section 15 of the Audit Act 1994 and the Australian Auditing and Assurance Standards. The cost of this audit was $760 000.
1.6 Report structure
The rest of this report is structured as follows:
- Part 2—Victoria's 10-year mental health plan
- Part 3—Meeting demand for mental health services.
1 Reform of Victoria’s specialist clinical mental health services: Advice to the Secretary, Department of Health and Human Services, by A.Cockram, S.Solomon, H.Whiteford, 2017, page 20.
2 Victoria's 10-year mental health plan
DHHS published the 10-year plan in November 2015 in response to government election commitments. Service accessibility is one of the primary considerations within the 10-year plan. Accessible mental health services mean they are available in the right place, at the right time and delivered by the right people with the right skills.
Demand for mental health services in Victoria is rising. The number of Victorians who require services, and the severity of illness, has increased. Population growth, different legal and illegal drug use patterns, and better mental health awareness are all driving this increased demand.
Without high quality and accessible services, many Victorians with mental illness are unlikely to receive timely help and support. Alongside the significant human cost, the lack of timely access to services has a substantial economic impact, and negative flow-on effects to other government services such as housing and justice services.
This part examines the extent to which the 10-year plan focuses on addressing demand.
2.1 Conclusion
While the 10-year plan clearly outlines the significant service demand and access issues facing the system, little within it directly addresses these issues. While effort has been directed to worthy activities such as new frameworks for suicide prevention and Aboriginal mental health and planning for forensic mental health services neither these initiatives, nor core services, can succeed while the system is overwhelmed. The priorities established in the 10-year plan do not reflect the most pressing challenges facing mental health services and their users.
DHHS's draft Clinical mental health services action plan 2018–2023, building on the 10-year plan, goes some way to addressing the challenges. The action plan details system changes to improve access to mental health services. However, while DHHS is using elements of the draft action plan to inform new initiatives, many of which government funded as four-year initiatives from 2018–19 onwards, it advises it is unlikely to finalise and release it. This misses the opportunity to communicate to stakeholders, who are in need of support, DHHS's goals for improving access, and also limits the ability of AMHSs, service users, and the public to hold DHHS to account in achieving its aims.
A completed 10-year plan priority action relevant to access is DHHS's workforce strategy. It includes new approaches to recruitment advertising and professional development, and helped inform a successful bid to government for funding for new mental health workers in 2019. However, the strategy has no concrete actions to address regional and rural workforce gaps, is isolated from service and capital planning, and has no measures or targets to show what DHHS hopes to achieve.
DHHS has not articulated any targets to measure progress against the 10-year plan's key challenge—providing timely access to the right services in the face of growing demand. Current measures that DHHS has aligned to the outcome of 'right services at the right time' either indirectly measure access, or do not measure access at all. While the measures focus on providing the 'right service', there are no measures addressing the 'right time' part of the outcome. If the focus of effort is truly to be on improving access, then DHHS must set relevant access measures and targets to drive performance and against which to publicly report progress. Compounding the lack of targets and measures is a lack of routine, senior level oversight of, and reporting against, the 10-year plan within DHHS, limiting senior executive attention to this high priority service.
2.2 Developing and implementing the 10-year plan
10-year plan aims
Victoria's 10-year plan is a high-level, outcome-focused framework for mental health service reform. DHHS's vision for mental health as outlined in the 10-year plan is that 'all Victorians experiencing mental illness get the best possible treatment and support, so they can live meaningful and fulfilling lives of their choosing'. The vision reflects one of the main objectives of the Health Services Act 1988, that 'an adequate range of essential health services is available to all persons, resident in Victoria irrespective of where they live or whatever their social or economic status'.
The 10-year plan aims to achieve its vision through four focus areas that contribute to sixteen outcomes as per Figure 2A.
Figure 2A
10-year plan focus areas and outcomes
Source: Victoria's Mental Health Services Annual Report 2016–17, DHHS, 2017.
The fourth focus area, describing an accessible system, is particularly relevant to meeting demand. The 10-year plan links these outcomes to the statements:
- Universal access to public services—people with mental illness and their families and carers have access to high-quality, integrated services according to their needs and preferences.
- Access to specialist mental health services—people with mental illness, their carers and families have access to the public treatment and support services they need and choose, appropriate to their age and other circumstances, where and when they need them most.
While the 10-year plan articulates these overarching goals, the outlined approaches focus on the way services are provided and developed and do not highlight actions to address the unmet demand that the plan acknowledges exists.
Stakeholder engagement
DHHS consulted with a wide range of stakeholders in developing the 10-year plan, including six rural and regional public workshops and gathering input from more than 1 000 consumers, carers, workers and other sector stakeholders. Our review of the records of public consultations notes diverse issues and opinions. Access to mental health services was a key issue highlighted in all public consultation records reviewed, including the gap between the number of people needing public mental health services and the capacity of specialist clinical services and community mental health support services to meet those needs.
DHHS prepared discussion papers to assist with developing the 10-year plan that included diverse groups, including Aboriginal communities, refugees and asylum seekers, and lesbian, gay, bisexual, transgender and intersex persons. Consultation questions included 'How do we configure the way specialist mental health treatment services are delivered to improve access and responsiveness to the needs of...'. However, though access was a key issue put forward during these consultations, improving access, including for diverse groups, has not been adequately reflected in the 10-year plan.
Each of the audited mental health services were critical of the 10-year plan. These stakeholders all said that while the 10-year plan includes many relevant issues, there are too many generic statements in response to these issues. Each service would like practical guidance and a plan that clearly outlines the key deliverables. They indicated they would like DHHS to engage more with them and develop a plan that is achievable and aligned with contemporary practice. Access and demand issues were discussed strongly by each of the audited AMHSs, with issues such as workforce capacity and geographic reach identified as barriers to addressing access.
Governance arrangements
The MHET was established to monitor the 10‑year plan's progress, as outlined in Figure 2B, and to provide guidance and advice on its implementation in the first two years.
Figure 2B
Initial governance structure for the 10-year plan
Note: LGBTI = lesbian, gay, bisexual, transgender and intersex; DJR = Department of Justice and Regulation; DET = Department of Education; DPC = Department of Premier and Cabinet; DTF = Department of Treasury and Finance.
Note: On 1 January 2019, a number of machinery of government changes came into effect, and consequently the Department of Justice and Regulation (DJR) became the Department of Justice and Community Safety.
Source: VAGO, based on information from DHHS.
The MHET included members representing service providers, peak bodies and other stakeholder organisations. The MHET's terms of reference included to:
- advise the minister on actions to achieve intended outcomes
- identify priorities and develop a work program of actions
- advise the minister on measures and targets to demonstrate achievement towards intended outcomes
- plan implementation activities.
Minutes from the MHET's meetings show discussion of a range of mental health issues, including taskforce priorities and updates on government activity. However, these documents do not show substantive discussion about access and demand. The taskforce also did not develop a clear work program of actions, with timeframes, and subsequently did not monitor progress against any agreed deliverables. The MHET, while considering and advising on progress indicators, did not set targets for them.
The MHET was disbanded in February 2018, at the completion of its fixed two‑year term. Oversight for progress against the plan now sits with the mental health branch within DHHS, which reports only to higher levels within DHHS—the Executive Board via the Health Reform Sub Committee—on an ad hoc basis. Since the MHET disbanded, the mental health branch has reported to the executive once about just one of the four priority areas within the 10-year plan. This lack of internal progress reporting significantly reduces accountability for achieving against the plan.
Implementing the 10-year plan
DHHS and other stakeholders have directed significant resources to implementing the activities underpinning the 10-year plan; however, there is no evidence of activity milestones, nor these being met.
A key DHHS focus was to create short and long-term implementation activities to achieve the plan's outcomes by identifying waves of reform that operate alongside other reform activities, shown in Figure 2C. The waves describe the order of priority actions over the first three years of the 10-year plan, as set out by the MHET. Key focus areas that are particularly relevant to access include the Workforce Strategy (Wave 1), Managing Clinical Demand (Wave 2), and in Wave 3, 'Diversity—ensuring that mental health services respond to diversity, particularly through identifying the specific needs of high-risk groups and tailoring mental health services to meet the needs of diverse communities'. Victoria's Mental Health Services Annual Report 2017–18 (2017–18 Annual Report), published by DHHS, outlines several actions commenced to support access for diverse consumers including:
- the development of guidelines for interpreters working in mental health settings
- work to engage and support young people from refugee and asylum seeker backgrounds
- a grants programs to fund initiatives that support lesbian, gay, bisexual, transgender and intersex young people.
Figure 2C shows the priorities by wave, when DHHS identifies that it started to act on them, and priorities they report as completed (shown with a tick).
Figure 2C
Waves of reform
|
Priority reform actions |
2016–17 |
2017–18 |
2018–19 |
|---|---|---|---|
|
Wave 1 priorities |
|||
|
Workforce strategy |
✓ |
||
|
Child and youth mental health services |
|||
|
Suicide prevention framework |
✓ |
||
|
Aboriginal social and emotional wellbeing—engagement phase |
✓ |
✓ |
|
|
Outcome measures development |
✓ |
||
|
Wave 2 priorities |
|||
|
Forensic mental health services |
|||
|
Managing clinical demand |
|||
|
Primary prevention |
|||
|
Aboriginal social and emotional wellbeing—strategy development |
✓ |
✓ |
|
|
Wave 3 priorities |
|||
|
Co-production—engaging Victorians with mental illness and their families and carers in the co-production and co-design of services |
Until June 2023 |
||
|
Service innovation—improving mental health services through a commitment to innovation and the adaptation of new technologies and service models |
Until June 2023 |
||
|
Choice—increasing choice in mental health services for Victorians with mental illness, their families and carers |
Until June 2023 |
||
|
Economic and social participation—improving opportunities for Victorians with mental illness for both economic and social participation, including the reduction of stigma and discrimination that acts as a barrier to participation |
Until June 2023 |
||
|
Service integration—ensuring mental health services are integrated with each other and relevant health, human, education and other services to meet the specific needs of clients |
Until June 2023 |
||
|
Diversity—ensuring that mental health services respond to diversity, particularly through identifying the specific needs of high-risk groups and tailoring mental health services to meet the needs of diverse communities |
Until June 2023 |
||
Source: VAGO, based on information from MHET planning material and interviews with DHHS staff.
We developed this progress report as DHHS does not track and report progress against the wave priorities.
2.3 Monitoring progress of the planin improving access
DHHS's outcomes framework for the 10-year plan sets indicators against the planned outcomes. Figure 2D shows the indicators DHHS has aligned to the outcome related to access: 'the treatment and support that Victorians with mental illness, their families and carers need is available in the right place at the right time', and results against these indicators, as reported publicly by DHHS.
Figure 2D
Results against mental health 'access' indicators 2014–15 to 2016–17
|
Indicator |
2014–15 |
2015–16 |
2016–17 |
2017–18 |
|---|---|---|---|---|
|
Rate of pre-admission contact—reflecting whether the person is appearing for the first time to an acute facility |
59.4% |
57.2% |
51.8% |
59.4% |
|
Rate of readmission within 28 days—indicating that the discharge from inpatient services may have been too soon, or the treatment or discharge planning may not have fully addressed the issue |
13.8% |
13.9% |
13.4% |
13.8% |
|
Rate of post-discharge follow-up—an important service to support transition back into the community |
85.7% |
84.2% |
77.7% |
87% |
|
New registered clients accessing public mental health services (no access in the last five years) |
36.3% |
35.7% |
36.6% |
36.8% |
|
Proportion of consumers reporting the effect the service had on their ability to manage their day-to-day life was very good or excellent—indicating general consumer satisfaction with the outcomes of the care provided |
N/A |
N/A |
53.5% |
55.2% |
Note: No data is available for the 'consumer' indicators for 2014–15 and 2015–16.
Note: The result for post-discharge follow up for 2016–17 was impacted by industrial issues.
Source: Victoria's Mental Health Services Annual Report 2016–17 and the 2017–18 Annual Report, DHHS.
Except for the measure regarding new registered clients, these indicators only provide an indication of whether consumers received the 'right service'. The lack of improvement in the readmission rate suggests ongoing challenges in providing the 'right service', though there are improvements in the most recent year data for consumer experience, pre-admission contact and discharge follow up, which likely reflects recent increases in funded service hours. However, none of the measures are truly relevant to access, which considers the 'right time' part of the intended outcome. There are no measures of wait times for services, the numbers of consumers declined or delayed service due to capacity constraints, or consumer-reported experience of service accessibility. The measure of new registered clients could provide an indication of the system's capacity to support access; however, measured as a percentage of total clients, it gives no information on whether actual numbers of new clients are growing.
Further, DHHS has not articulated any targets for the measures that it has set. Without targets, it is unclear what level of improvement DHHS is aiming for.
As shown in Figure 2E, available service usage and capacity data for 2014–15 to 2017–18 shows recent improvements in the numbers of people accessing public mental health services; however, this reflects only a marginal increase in the proportion of people receiving care. The large gap against the target for timely access to a mental health inpatient bed from an ED persists. DHHS could use the information it already collects to set targets for improvements to access.
Figure 2E
Alternate indicators of mental health service accessibility
|
Indicator |
2014–15 |
2015–16 |
2016–17 |
2017–18 |
|
|---|---|---|---|---|---|
|
Community service contacts (number) |
2 058 909 |
1 935 262 |
1 675 772 |
2 407 730 |
|
|
Community service contacts (hours) |
1 011 396 |
971 965 |
881 950 |
1 288 028 |
|
|
Total numbers of people accessing clinical mental health services(a) |
67 030 |
67 559 |
66 487 |
72 859 |
|
|
Proportion of population receiving clinical care(b) |
1.13% |
1.12% |
1.08% |
1.16% |
|
|
Jul–Sep 2017 |
Oct–Dec 2017 |
Jan–Mar 2018 |
Apr–Jun 2018 |
Jul–Sep 2018 |
|
|
Audit mental health ED presentations transferred to a mental health bed within eight hours—target is 80% |
55% |
56% |
56% |
59% |
53% |
(a) 2015–16 and 2016–17 data collection was affected by industrial activity. The collection of non-clinical and administrative data was affected, with impacts on the recording of community mental health service activity and client outcome measures.
(b) Population estimate is based on Victorian in Future 2014 projections.
Source: VAGO, based on information from Victoria's Mental Health Services Annual Report 2016–17, the 2017–18 Annual Report, and the Victorian Health Services Performance website www.performance.health.vic.gov.au, DHHS.
Suicide rates, while determined by multiple environmental factors, in part reflect the quality and availability of clinical supports. The only stated outcome of the 10-year plan with a clear target relates to the aim to halve the Victorian suicide rate by 2025.
The 2017–18 Annual Report states there has been a reduction in the number of suicides from 654 in 2015 to 621 in 2017. However, 10-year data available from the Australia Bureau of Statistics shows that there is no significant reduction. As shown in Figure 2F, the suicide rate has been relatively stable, varying slightly around 10 per 100 000 with an increase between 2013 and 2014 due to a change to incorporate cause-of-death post coroners' enquiries2. To halve the 2015 rate of suicides these numbers will need to decline to around 418 in 2025 based on current Victorian population projections.
Figure 2F
Victorian suicide rate per 100 000 population, by year, 2008 to 2017
Source: VAGO, based on Australian Bureau of Statistics data.
DHHS has not completed an evaluation framework to support the 10-year plan; however, DHHS's Centre for Evaluation and Research is planning a formal evaluation of the 10-year plan by 2020, five years into the plan. To properly complete this task, performance indicators relevant to improving access to services and more importantly, targets are necessary, particularly to ensure DHHS and AMHSs collect the right data for the evaluation.
2.4 The draft Clinical mental health services plan 2018–2023
The draft Clinical mental health services action plan 2018–2023 is a blueprint for transforming clinical mental health services in Victoria to address demand for, and access to, mental health services. The action plan supports the 10-year plan implementation. The action plan's focus areas are:
- transforming adult community-based services by:
- increasing their capacity to treat more people and respond at earlier stages of illness
- supporting clinicians to deliver evidence-based and best practice interventions
- streamlining and improving service entry processes so that people can get timely assessment of their needs and referral to mental health or other services
- introducing new responses to help people experiencing a mental health crisis
- providing a balanced system of high-quality bed-based services, included enhanced sub-acute services to relieve pressure on acute inpatient units
- building links with and support for other services, with alcohol and other drug services prioritised for immediate action
- responding effectively to people with complex needs who present risks to community safety
- strengthening services for children and young people.
The key enablers are:
- a new funding model that incentivises health services to accept more patients and direct resources to the highest need patient groups
- a new Mental Health Performance and Accountability Framework that reflects the intended funding reform and creates greater transparency about service performance and consumer outcomes
- support for the mental health workforce, including in the delivery of evidence based and best practice treatment
- service and infrastructure planning to identify the optimum mix of community-based, sub-acute and acute inpatient services, taking account of the need for infrastructure to reflect demographic changes
- high-quality government policies, legislative frameworks and guidance for the sector
- strategic investment in research and evaluation to create a system that is continually learning.
Currently, this document is in draft form. It takes a step towards supporting AMHSs and their stakeholders by outlining more direct actions to reform the system and address capacity issues. While it took three years to develop, DHHS advises that it is unlikely to be finalised and released. DHHS is using elements of the draft action plan to inform new initiatives, many of which were funded as four-year initiatives from 2018–19; however, it is a missed opportunity for DHHS to not release the plan, particularly given the clear need of AMHSs for more communication about DHHS's intentions in this area.
2.5 Workforce strategy
Currently, there are over 5 000 people working in mental health, predominantly in roles such as psychiatry, mental health nursing, social work, psychology and occupational therapy, and increasingly, lived-experience workers (both consumers and carers) and other allied health professionals (such as speech pathologists). We found through our consultations with AMHSs that recruiting, retaining and managing their workforce is one of their most significant obstacles to providing access to services. They cited low morale and an ageing, stretched workforce as key challenges, in addition to stigma and negative community perceptions. The mental health workforce is impacted by:
- insufficient workers, particularly in rural and remote areas
- a change in service delivery needs from community mental health services to acute mental health services and the different skills needed
- risks to safety and wellbeing
- a lack of development opportunities
- inadequate undergraduate and other training opportunities.
DHHS is aware of these workforce challenges and has been actively trying to address them through a range of initiatives. The workforce strategy is a key focus area under wave 1 of the 10-year plan. DHHS published the new workforce strategy in June 2016, which builds on Victoria's specialist mental health workforce framework: strategic directions 2014–24 and the previous 10‑year plan Because mental health matters: Victorian Mental Health Reform Strategy 2009–2019. The workforce strategy outlines five key objectives, with the first being most relevant to access:
- workforce availability and skill—right person, right place, right skill
- worker safety and satisfaction—places people want to work
- workforce integration—learning together, working together
- co-design and co-delivery with consumers and carers—shaping the future together
- workforce innovation—exploring and sharing new ways of working.
|
The Centre for Mental Health Learning will act as an umbrella organisation, coordinating and leveraging current mental health investments by partnering with statewide trainers, Mental Health Workforce Learning and Development Clusters, health services, clinical academics and other stakeholders. |
Initiatives within the workforce strategy that aim to support workforce availability and skill include:
- the provision of learning and development in priority areas through DHHS's new Centre for Mental Health Learning (see sidebar)
- a targeted mental health recruitment campaign, Hello Open Minds, to attract and retain a skilled and sustainable workforce (launched in July 2017)
- workforce planning, informed by routine workforce data collection, to highlight where development and growth need to be focused
- a range of actions to attract and retain Aboriginal people to the mental health workforce
- expansion of the paid 'lived-experience' workforce to provide consumers with more choice in the types of services they receive, including peer support and advocacy
- a commitment for further work to address issues of occupational violence that affect attraction and retention.
A number of activities relate to addressing access by increasing the mental health workforce with initiatives such as Hello Open Minds—a strategy to support recruitment—and the Centre for Mental Health Learning—aimed at improving the retention of the workforce through professional development and enhancing their ability to care for clients with complex needs. DHHS also requested and received funding to support workforce initiatives aimed at increasing the number of mental health staff. In 2019, additional clinical nurse consultants and mental health engagement workers will be recruited.
Despite this range of workforce activities, it is not clear what DHHS aims to achieve through its workforce strategy and initiatives, as it has not set quantifiable performance indicators or targets, and there are no plans for a formal evaluation. DHHS advice to government through its 2018–19 business case to 'Reform clinical mental health services', does articulate the need for growth funding, additional and different services and additional staff, but does not explain their interdependencies. DHHS requires a clear understanding of the numbers and types of staff needed, and where and when they are needed, to enable its broader service reforms to occur. This in turn, would inform specific targets. Without such ways to measure progress, DHHS cannot track whether its investment in the workforce strategy and initiatives is growing and supporting the mental health workforce. The strategy also does not directly address the identified issue of higher workforce gaps in regional and rural areas.
2 Australian Bureau of Statistics technical note 2 CAUSES OF DEATH REVISIONS, 2013, http://www.abs.gov.au/ausstats/abs@.nsf/Previousproducts/3303.0Technical%20Note22015?opendocument&tabname=Notes&prodno=3303.0&issue=2015&num=&view=, 2018.
3 Understanding and meeting demand
Demand for mental health services in Victoria is increasing, not just in relation to the number of people who need services, but also in the severity of illness. The drivers of the increased demand include population growth, legal and illegal drug use, and heightened community awareness of mental health issues. The number of people experiencing mental illness in Australia has increased significantly in the last 10 years, as Figure 3A shows, and Victoria is consistent with this trend.
Figure 3A
Growth in number of Australians experiencing mental illness by area of residence
Source: Mental health services: In brief 2018, AIHW.
DHHS's intention for the mental health system is that, where possible, people are supported to remain in the community—which is often the best environment for the individual, and also reduces demand on bed-based services. However, achieving this aim relies on a system with the capacity to provide timely access to services.
This part examines the aspects of the mental health service system that underpin the provision of access to services; funding, demand, infrastructure and service distribution.
3.1 Conclusion
DHHS's 10-year plan includes 'enabling greater access to high quality, integrated services'—Outcome 13. Victorians have a right to expect this level of service from their public mental health services and to achieve this outcome, the system needs funding and infrastructure that matches demand and a service model that promotes, rather than impedes, access. Recent advice from DHHS to government, supported by multiple DHHS-commissioned reviews, clearly articulates the existing funding and infrastructure gaps. However, DHHS progress has been slow and the most important elements of change, such as funding reform, infrastructure planning, catchment area review, and improved data collection have only just, or not yet commenced. There is real risk that achievements intended within the 10-year plan's lifespan will not occur. Considerable acceleration of effort is required.
3.2 Funding
Victoria's public mental health services are subject to an input-based funding model. In this model, DHHS allocates a block of funding to AMHSs based on their number of inpatient beds or previous year's client numbers, which is indexed at 1.6 per cent per annum. The allocation is not sensitive to unmet demand, the needs and complexity of the mental health services' client cohort, contemporary population data, nor demographic changes.
AIHW data shows that between 2011–12 and 2015–16 national recurrent expenditure per capita on specialised mental health services grew an average of 0.7 per cent annually. Over that time in Victoria it declined by 0.3 per cent annually. In 2015–16, Victoria's per capita recurrent expenditure was $197.30, the lowest in Australia, against a national average of $226.52.
Funding for the mental health system since the 10-year plan was issued increased by $100.0 million in 2017–18 and $106.8 million in 2018–19. The Victorian State Budget 2018–19 provides $1 605.7 million in mental health funding, which will assist Victoria to address the funding disparity with other states and territories.
DHHS will spend $83.7 million during the 2018–19 financial year to begin clinical mental health services reform with a number of initiatives to help address access including:
- redesigning community-based mental health services
- strengthening the mental health workforce
- six new mental health and alcohol and drug service hubs
- growth in community mental health service hours
- increasing clinical capacity in sub-acute services.
Impact of funding shortfalls
Despite mental health system growth funding allocation over the last three state budgets, the lack of funding for more than 10 years has forced AMHSs to focus on acute and crisis treatment at the expense of earlier intervention services in the community. While community mental health received a share of growth funding, 2.3 per cent in 2016–17 and 7 per cent in 2017–18, AMHSs advise that this growth funding was largely directed to filling the existing gap between their service costs and the price DHHS pays, rather than providing additional services.
Because AMHSs often redirect resources from community to hospital settings to support consumers who need a higher level of care, AHMSs have limited capacity to intervene in the earlier stages of mental illness or deliver high quality interventions in the community to promote recovery. This limitation contributes to an increase in the number of people admitted to acute care without prior community contact. Between 2009 to 2016 acute admissions grew by 19 per cent, while community mental health contacts decreased by 17 per cent, which contributes to a cycle of increasing demand for costly emergency and inpatient services and further impacts AMHSs' ability to provide effective interventions during earlier stages of illness. Recent increases in funding for community services, however, have seen more people have preadmission contact, which begins to address this problem.
The audited AMHSs also advised that their bed day costs are higher than the price DHHS pays, and that they do not receive the necessary funding to meet demand. DHHS costings of acute mental health inpatient funding found that the price paid by DHHS meets only around 62 per cent of full costs to AMHSs, compared to 82 per cent of the price paid for general acute hospital beds. A DHHS commissioned review advised that the price paid should be 80 to 85 per cent of the full cost. All the audited AMHSs advised that, because of the current gap, AMHSs cross-subsidise their inpatient mental health services from other areas within the health service, which risks a negative impact on those services.
The case for funding reform
The introduction of activity-based funding in mental health services has been on the agenda in Victoria for over five years—DHHS's 2016–17 Acute Funding Review identified the need for mental health funding reform. DHHS's commissioned review 'Reform of Victoria's specialist clinical mental health services December 2017' (2017 review) also recommends that a future funding model should include output, input, block and outcome funding. Alongside this model is national health funding reform and the need for Victoria to align with the new Australian Mental Health Care Classification (AMHCC). The AMHCC is designed to provide consistency across health services, support integrated service delivery across services, and enable mental health services to be priced and funded on an activity basis.
|
Packages of Care—patients are classified into one of 13 levels by the complexity of their issues, phase of care and social connectedness, with funding matched to the needs of each classification level. DHHS intends to provide AMHSs with a single annual payment based on their patient mix. Over time, DHHS will bundle funding for community care and acute care to provide the strongest incentive to substitute community mental health services for acute care where clinically possible. In the interim, DHHS has started funding packages of care for high needs patients. |
DHHS is now implementing funding reform for clinical mental health services that will move away from an input-based model towards bundling bed and community hours funding through 'packages of care' that are informed by the complexity levels of the client mix at an AMHS. The aim is to improve the support for clients most in need of mental health services and to incentivise AMHSs to assist people to remain well within the community setting. This is consistent with the findings and recommendations in DHHS's 2017 review which emphasises the need to increase community-based mental health treatment to reduce the demand on acute services. The four-year funding reform began in 2018–19 with a 'shadow' year to allow AMHSs to adjust to the changes. If this funding distribution method is successful, it will enable greater early access for consumers in need of mental health services and eventually alleviate demand for acute mental health services.
While the new funding model is well aligned to the intent to incentivise more community-based treatment, without an adequate quantum of funding (and the staff and infrastructure to deliver the services) there is risk that the intended outcomes will not be achieved. DHHS advice to government states that the new funding reform model aims to provide each new community-based client with a maximum of six hours treatment per annum and that the nationally recommended level is 72 hours per annum. DHHS also notes that the four-year growth funding will enable DHHS to provide mental health services to 1.2 per cent of the population in 2018–19 and thereon, only a marginal improvement on the current 1.16 per cent coverage compared to the estimated 3.1 per cent of the Victorian population with a severe mental illness. This growth funding also only increases the price paid to 67 per cent of AMHSs' costs.
Another change is that DHHS has moved bed funding to a single price for all beds regardless of location or severity of illness. It is unclear how DHHS is addressing the risk of disadvantaging some service providers such as rural AMHSs that have inherently higher operating costs.
3.3 Understanding and planning to meet demand
Demand for mental health services in Victoria has increased over the last 10 years, and this trend is likely to continue, as indicated by Figure 3B. This demand is exceeding population growth, as shown in Figure 3C.
Figure 3B
Number of people receiving mental health services in Victoria
Note: Data was not available for 2011–12 and 2012–13.
Source: VAGO, based on Report on Government Services, Productivity Commission, 2017.
|
Mental health separations—when a patient formally admitted to hospital, receives at least one episode of care (and is in hospital for more than one day). Same-day services are counted separately. |
Figure 3C
Indexed growth in Victorian health service-related events versus population
Note: Between 2011–12 and 2012–13 the negative growth in public hospital separations was due to a change in admissions policies (patients accommodated in the ED only were no longer counted as admitted). Once hospitals reconfigured their ED/inpatient interface, growth in separations has consistently increased.
Source: VAGO, based on information from DHHS using internal and Australian Bureau of Statistics data.
DHHS's 2017 review estimates that close to one million Victorians have a mental illness, with around 184 000 having a severe mental illness, as Figure 3D shows.
Figure 3D
Estimated number of Victorians with a mental illness
|
Severity of illness |
Percentage of Victorians with a mental illness (%) |
Number (thousands) |
Percentage requiring treatment |
Number needing treatment (thousands) |
Primary government responsibility |
|---|---|---|---|---|---|
|
Mild |
9.0 |
537 |
50 |
268.5 |
Commonwealth |
|
Moderate |
4.6 |
272 |
80 |
217.6 |
State/Commonwealth |
|
Severe |
3.1 |
184 |
100 |
184 |
State |
|
Total with mental illness |
16.7 |
993 |
670.1 |
Source: 2017 review, DHHS.
The table highlights the unmet demand for services in Victoria. In 2017–18 there were 72 859 registered users of mental health services, compared to the estimated 184 000 with severe mental illness that DHHS's 2017 review states need treatment.
Victoria falls significantly behind other jurisdictions and the national average in the proportion of the population receiving clinical mental health services, as Figure 3E demonstrates.
Figure 3E
Percentage of the Victorian population receiving clinical mental health services compared to other jurisdictions and the national average
Source: VAGO, based on information from AIHW's Mental health services in Australia 2013–14 cited in Design, Service and Infrastructure Planning Framework for Victoria's Clinical Mental Health System, DHHS, 2017.
Increasing demand combined with current service shortfalls are placing the whole mental health service under considerable stress. The DHHS-commissioned Design, Service and Infrastructure Planning Framework for Victoria's Clinical Mental Health System report states that increased demand has placed pressure across the mental health system over the last 10 years, which includes:
- ED presentations increasing 9 per cent from 2015–16
- acute hospital admissions growing at an annual rate of 2.4 per cent
- LOS in hospital trending down from 14.7 days to 11.2 days from 2009 to 2017—potentially not providing enough time for patients to become well
- unplanned readmission rates for adult mental health patients at 14.4 per cent in 2017–18
- community mental health contacts per 1 000 people declining at a rate of 2.5 per cent per annum over the last 10 years.
Figure 3F shows the increase in adult mental health admissions from 2009 to 2017. The increased number of presentations coupled with a shortage of mental health beds affects patients' LOS, meaning some patients likely do not receive the length of treatment they need. The 2017–18 Annual Report states LOS for adult acute mental health patients is just 9.6 days, a further decrease from that reported in the 2017 DHHS-commissioned review.
Figure 3F
Acute adult mental health admissions and average length of stay, 2009 to 2017
Source: Reform of Victoria's specialist clinical mental health services: Advice to the Secretary, Department of Health and Human Services, by A.Cockram, S.Solomon, H.Whiteford, 2017.
DHHS's 2017 review found demand pressures have also increased the threshold for access to community-based services so that AMHSs only see the most unwell, which creates a flow on effect with AIHW reporting the number of mental health patients accessing acute services through police, ambulance and self-presentations to hospital EDs increasing from 28 757 in 2004–05 to 54 114 in 2016–17.
Mental health patients are also staying in EDs longer. Between 2015 to 2017 their average wait time in EDs has gone from 7.6 hours to 9.5 hours, well over the national target of 4 hours. Mental health patients are the most represented when wait times for movement from the ED to a bed exceed 24 hours—79 per cent of patients compared to 30 per cent five years ago. For patients experiencing acute mental illness, the ED environment is often clinically inappropriate, and at times the presence of acutely unwell patients in the ED presents risks to the patient and others around them.
Collecting data to understand the system
To understand and respond to demand and access issues, DHHS needs systems that capture necessary data to reflect current service capacity and use statistical techniques to calculate unmet demand.
DHHS's key data tool is its Client Management Interface/Operational Data Store (CMI/ODS). AMHSs use it to record the core data elements of their service provision as mandated under the Act.
|
Mental health triage is the first point of system entry for potential consumers, or people seeking assistance on behalf of another. A triage clinician assesses whether a person is likely to have a mental illness and the nature and urgency of the response required. Where an AMHS is not the most appropriate option for the person, they are referred to another organisation or given other advice. When specialist mental health services are likely to be suitable, the triage clinician comprehensive intake assessment is done. The intake assessment may result in referral to another organisation and/or in the person being treated within the specialist mental health service. Only clients that receive treatment are recorded in CMI/ODS. |
All the audited AMHSs use CMI/ODS as part of their data collection. They input data up to three times a day and this data links to quarterly reporting against KPIs that measure, for example, the rate a patient is readmitted, use of seclusion, and rates of post-discharge follow-ups.
However, while DHHS and AMHSs consider the data recorded to be accurate, five of the six audited AMHSs reported shortcomings in the CMI/ODS system including lack of functionality and low useability. Due to this shortcoming, the audited AMHSs use their own bespoke systems in addition to CMI/ODS for collecting and analysing data, duplicating effort in what is an already stretched workforce.
DHHS's 2017 review highlights the lack of comprehensive mental health triage data at a statewide level. The review notes the limitations the lack of data places on understanding the people who AMHSs do not accept into the mental health system and the reasons. The report states there has been a 63 per cent increase over the last four years in the number of people seeking access to, but not accepted by, AMHSs. This is also supported by DHHS's data analytics work undertaken in 2017, which used some triage information to demonstrate service demand increased by 43 per cent between 2010–11 and 2016–17.
DHHS is aware of the gaps in its triage data collection and the need to review triage services. While DHHS has decided to delay triage reform until after funding reforms, there is still an opportunity to improve data collection and analysis now to better inform future change.
In 2017, data analytics work by the Victorian Data Linkage Centre within DHHS in conjunction with external consultants noted limitations in the current data set and made several recommendations, including:
- incorporating data on unregistered clients into CMI/ODS to give a more complete picture of service activity and demand
- integrating mental health triage (see sidebar) data into CMI/ODS to give a better picture of service demand and analysis of how quickly services are provided as is done in other jurisdictions
- including information about mental health clients that present to EDs for treatment to allow for analysis of preventable ED presentations
- including information about people that contact mental health triage and do not go on to receive services but later present at an ED.
Forecasting demand
Having an estimate of future mental health system demand is crucial to ensuring adequate future service access and to advise government of funding needs. DHHS lacks a comprehensive view of current mental health service demand, and until recently DHHS utilised only basic forecasting.
|
Capture-recapture is a statistical method to estimate the population of a subset of a population. Typical applications include estimating the number of people needing particular services, or with particular conditions. |
DHHS's current forecasting tool is available on its intranet and DHHS has committed to using this tool for its mental health work. It provides forecasting for system indicators including registered client numbers, acute admissions, community contacts and case length by taking historical data and aligning this with forecast population growth.
DHHS applies a statistical method of approximating demand known as 'capture‑recapture', which informs its forecasting model that helps to estimate unmet demand by utilising DHHS data sources including ED presentations and information from its drug and alcohol, disability and child protection datasets. However, without the inclusion of data from the triage system and unregistered clients there remains a significant risk that using this statistical method, DHHS does not adequately capture the extent of mental health illness in the population and the true unmet demand for services.
Figure 3G is an example of forecasts using this tool, it projects the number of registered mental health clients will increase from 62 000 in 2017 to 80 000 in 2031—a 29 per cent increase—with the proportion of clients with moderate illness increasing from 38 per cent in 2017 to 42 per cent in 2032 and clients with severe illness being relatively stable at 33 per cent. Given the model limitations, the projection should be considered conservative, particularly as the number of registered clients for 2017–18, 72 859, already exceeds the projection for that year.
Figure 3G
Past and forecast registered active clients by illness severity
Source: DHHS, 2017.
3.4 Capital infrastructure
The other foundational factor needed to meet demand for mental health services is capital infrastructure: namely inpatient beds, including separate facilities for female inpatients. Responding to this need requires significant forward planning as new facilities take around five years to plan and build and, without accurate demand forecasting, can be already at or over capacity when they open.
Victoria's acute mental health beds are under significant pressure. There is sufficient evidence from the recent reviews that there are not enough mental health beds in Victoria to meet current, or future, demand. A DHHS review found that all major acute psychiatric units are continually operating at or above 95 per cent capacity, well above desirable levels of 80 to 85 per cent that allow AMHSs to admit acutely ill patients as needed.
The audited AMHS confirmed the capacity issue during our site visits. The impact on patients of high bed capacity is that AMHSs must make difficult decisions to manage bed availability. Audited AMHSs informed us that strategies used to manage bed availability include increasing the LOS in EDs, discharging the least unwell, and utilising other wards such as aged care, potentially placing a patient's care at risk.
In most facilities, males with acute mental health issues mix with female inpatients, which places women at significant risk of sexual abuse. Victoria's Mental Health Complaints Commissioner's The Right to be Safe: Ensuring sexual safety in acute mental health inpatient units: sexual safety project report (The Right to be Safe: Sexual Safety Project Report) found that 74.4 per cent of sexual safety complaints from 2014 to 2017 related to mixing males with acute mental health issues with female inpatients as shown in Figure 3H. AMHSs cite challenges to separating males and females because of ageing infrastructure.
Figure 3H
The Right to be Safe: Sexual Safety Project Report
|
Victoria's Mental Health Complaints Commissioner's The Right to be Safe: Sexual Safety Project Report assessed 90 complaints from 1 July 2014 to 30 June 2017 that related to the sexual safety of acute mental health inpatients. The Commissioner found that most complaints related to breaches that occurred in the high dependency units or intensive care areas of the ward (40.4 per cent) or in bedrooms (34 per cent). The commissioner found that while most health services have some type of separate gender area, six cases occurred in women's only areas and for a further 22 cases, the health services reported that the service infrastructure (including gender separate areas) was not being adhered to. During our audit, all audited health services reported that they struggled to separate males and females due to a lack of appropriate infrastructure. |
Source: VAGO, based on The Right to be Safe: Sexual Safety Project Report, Victoria's Mental Health Complaints Commissioner, 2018.
The availability of acute mental health beds is different across geographic areas, with outer suburban areas not keeping pace with population increases in growth corridors. Demographic changes in regional areas also impact bed requirements, for example at least two of the four regional AMHSs audited cited the ageing population in their catchment area and the need for more aged mental health beds.
To service current unmet need as well as future demand and to adequately support community-based treatment and care, the mental health bed base across Victoria must be increased. Victoria currently has the lowest bed base nationally as well as a comparatively low bed base globally. A review commissioned by DHHS advised that Victoria's bed base should increase in line with the bed base provided by other comparable states. The review estimates that the bed base would need to grow by 80 per cent over the next decade, which highlights the existing low bed base per head of population in Victoria shown in Figure 3I.
Figure 3I
Comparison of states and territories on per capita utilisation of mental health beds and community contacts
Note: Excludes forensic mental health beds.
Source: AIHW's Mental health services in Australia 2013–14, cited in DHHS-commissioned consultant report, Design, Service and Infrastructure Planning Framework for Victoria's Clinical Mental Health System, 2017.
There are 53 new acute adult beds funded in 2018–19; with 21 now open and 34 in planning. There are also 24 sub-acute beds in the planning phase, and 10 mother and baby unit beds will now operate seven rather than five days a week. No further new beds are in the capital pipeline and given population growth, current and planned beds will not meet the unmet demand nor move Victoria towards the recommended bed base. Delivering mental health facilities requires significant planning and construction time—around five years—in part due to the need for reinforced walls, egress and seclusion areas, outside space, and anti-ligature features.
DHHS intends to complete a 'Detailed services and infrastructure plan for Victoria's clinical mental health system over the next 20 years' and update it every five years to support the 'Statewide design, service and infrastructure plan for Victoria's health system 2017–2037'. However, given it will likely take DHHS some time to complete this plan, secure and allocate funding, and then plan and build infrastructure, DHHS should anticipate and plan for Victorians with mental health issues to continue to experience problems accessing mental health beds at least across the remaining life of the 10-year plan, and that this will impact the effectiveness of any changes to funding or the service delivery model.
3.5 Catchment areas
Clinical mental health services are provided in geographic catchment areas that were established in the 1990s. The consumer's place of residence determines which service or services they can access. DHHS's internally commissioned reviews highlight practical problems with the current area-based clinical mental health system that impact Victorians' ability to access services, which include:
- the catchment areas are not aligned with other health and human service areas, or local government area boundaries, which makes service coordination difficult for consumers and carers, many of whom need support from multiple services
- lack of alignment between geographic catchments and age-based service groupings
- lack of coordination between catchment areas when patients need to access services across catchment borders
- misalignment between service levels and types within a catchment and population growth and demographic changes in that area.
In August 2013, DHHS reviewed the mental health catchments. The review states that 'reconfiguring the catchment areas under which clinical mental health services are organised is a key step in delivering the kind of seamless, easy-to-navigate system that consumers and carers expect. It is also important for achieving optimal efficiency and effectiveness across the state'. Commitment to changing the catchment areas was included in the then Department of Health's strategy document, Victoria's priorities for mental health reform 2013–15. Despite this, DHHS has not implemented the changes to catchment areas.
In 2017, DHHS commissioned external consultants to develop the Design, Service and Infrastructure Planning Framework for Victoria's clinical mental health system. The framework recommended the following principles in reconfiguring service regions:
- Design service regions for populations between 500 000 to 1 000 000 people forecast by 2036, where appropriate and practical taking into consideration geographic placement of services and other factors.
- Improve access, outcome and demand management in growth corridors, including that sensible access to services overrides artificial geographical boundaries where appropriate.
- Align catchment areas with contemporary local government areas.
DHHS has not yet implemented these recommendations. While issues relating to catchments are complex and challenging, it is a critical piece of work that will contribute to improved access for consumers and we recommend that DHHS direct resources to this issue.
Appendix A. Audit Act 1994 section 16—submissions and comments
We have consulted with DHHS, Bendigo Health, Melbourne Health, Monash Health, Latrobe Regional Hospital, Peninsula Health and South West Healthcare and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report to those agencies and asked for their submissions or comments. We also provided a copy of the report to the Department of Premier and Cabinet.
Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
- DHHS
- Melbourne Health
RESPONSE provided by the Secretary, DHHS
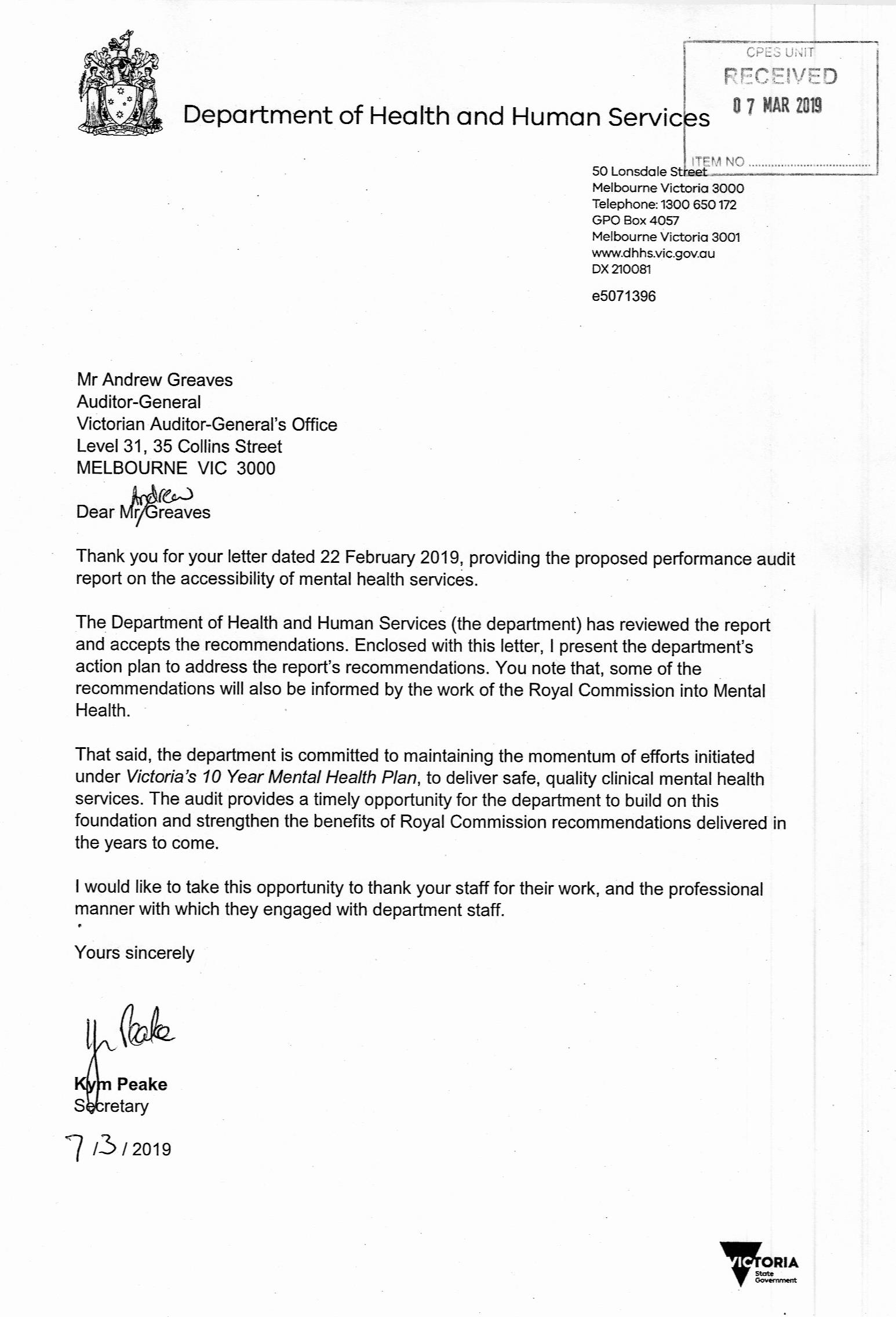
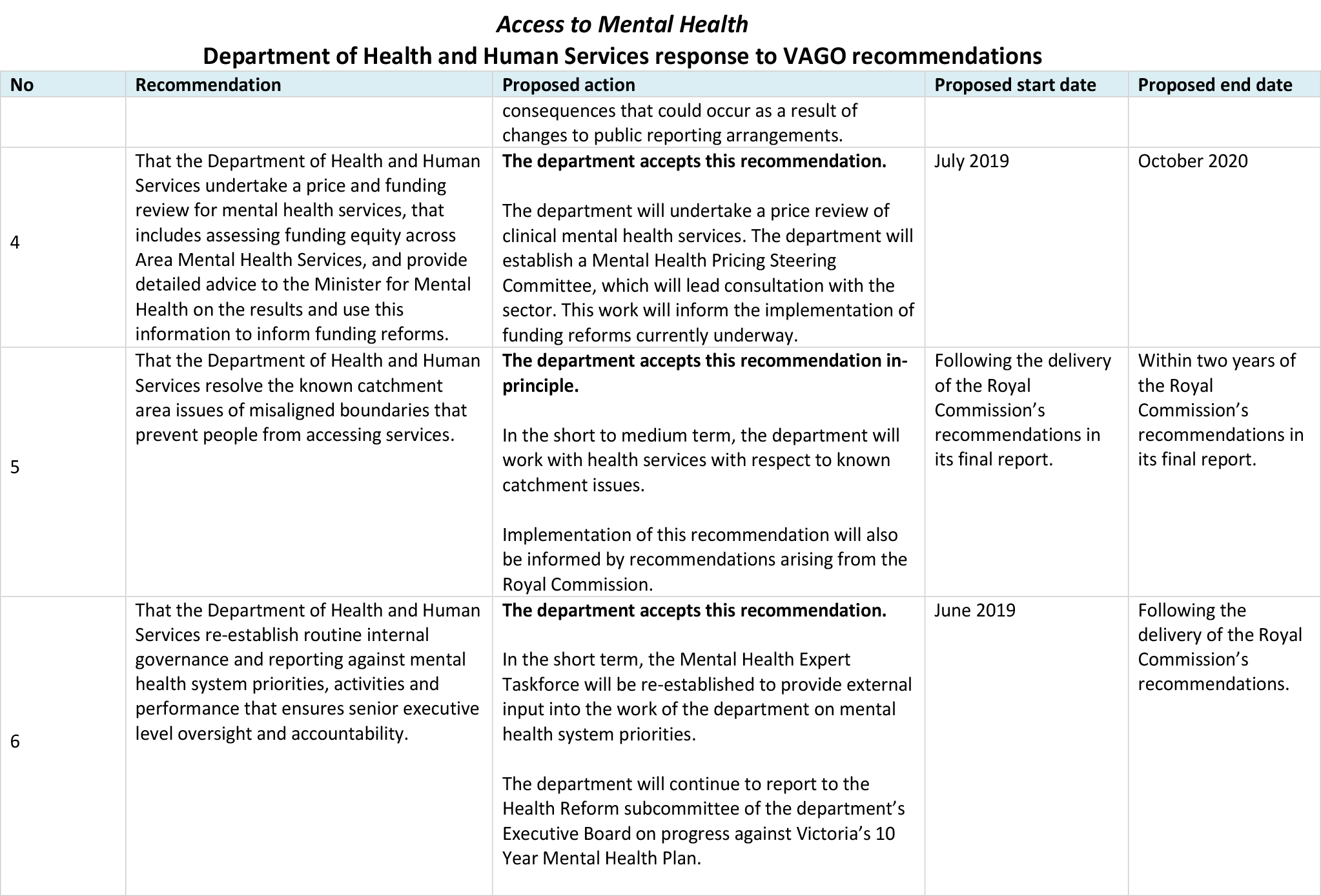
RESPONSE provided by the Chief Executive, Melbourne Health