Child and Youth Mental Health
Overview
Mental health problems are the most common health issues facing young people worldwide, according to the Global Burden of Disease Study 2017. One in four Australians aged 16–24 will experience mental illness in any given year.
For children and young people, intervention early in life and early in mental illness can reduce its duration and impact. Without access to mental health services, young people are at risk of ongoing problems that may affect their engagement with education and employment, and lead to greater contact with human services and the justice system.
This audit assessed whether child and youth mental health services are effectively preventing, supporting and treating child and youth mental illness. We examined how the Department of Health and Human Services (DHHS) designs and administers child and youth mental services, and facilitates access and service coordination for the most vulnerable and complex clients.
We made 20 recommendations for DHHS.
Transmittal letter
Independent assurance report to Parliament
Ordered to be published
VICTORIAN GOVERNMENT PRINTER June 2019
PP No 36, Session 2018–19
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report Child and Youth Mental Health.
Yours faithfully
Andrew Greaves
Auditor-General
5 June 2019
Acronyms
| AWH | Albury Wodonga Health |
| CAMHS | child and adolescent mental health services |
| CAP | child and adolescent psychiatrists |
| CEO | chief executive officer |
| CMI | Client Management Interface |
| CYMHS | Child and youth mental health services |
| DHHS | Department of Health and Human Services |
| DJCS | Department of Justice and Community Safety |
| DTF | Department of Treasury and Finance |
| ECT | electroconvulsive treatment |
| KPI | key performance indicator |
| MACNI | Multiple and Complex Needs Initiative |
| MHIDI | Mental Health and Intellectual Disability |
| NDIS | National Disability Insurance Scheme |
| NOCC | National Outcomes and Casemix Collection |
| OCP | Office of the Chief Psychiatrist |
| ODS | operational data score |
| PCP | Primary Care Partnership |
| PHN | Primary Health Networks |
| PRISM | Program Report for Integrated Service Monitoring |
| RANZCP | Royal Australian and New Zealand College of Psychiatrists |
| RCH | Royal Children's Hospital |
| SCV | Safer Care Victoria |
| SDQ | Strengths and Difficulties Questionnaire |
| SoP | Statement of Priorities |
| VAGO | Victorian Auditor-General's Office |
| VAHI | Victorian Agency for Health Information |
| Y-PARC | Youth Prevention and Recovery Centres |
Audit overview
|
There are many different terms used for children and young people in different contexts. In this report:
'Children and young people' is used in this report as a generic term that has no specific age grouping or may refer to several different groupings that are later specified. |
Mental health problems are the most common health issues facing young people worldwide, according to the Global Burden of Disease Study 2017. Mental health problems encompass mild and short-term problems to severe, lifelong and debilitating, or life-threatening problems.
Three-quarters of all mental health problems manifest in people under the age of 25. One in 50 Australian children and adolescents has a severe mental health problem. Severe mental health problems include acute psychiatric disorders, such as schizophrenia, that are persistent and make daily tasks difficult. Some severe mental health problems can be triggered by trauma such as abuse or neglect, or by developmental disorders or physical trauma that leads to disability.
The likelihood of mental health problems increases exponentially where there are other indicators of vulnerability such as unstable housing and poverty, neglect and abuse, intergenerational trauma or developmental disabilities.
Intervention early in life, and early in mental illness, can reduce the duration and impact. Early intervention is especially important for children and young people because many mental health problems can affect psychosocial growth and development, which can lead to difficulties later in life.
Victoria's public mental health services focus on the treatment of more severe mental health problems and support infants, children, and young people through a mix of community, outreach, and inpatient hospital services. They also provide education, upskilling and leadership on managing mental health problems to the services and agencies that involve children and young people, which include schools, child protection, and disability services.
There has never been an independent review of clinical mental health services for children and young people in Victoria, despite significant changes in the service system with the introduction of the National Disability Insurance Scheme (NDIS) and headspace centres (youth-specific community mental health services).
This audit assessed the effectiveness of public child and youth mental health services (CYMHS) in one regional and four metropolitan health services. After our planning process identified the most significant risks for CYMHS, we focused on whether the services have been designed appropriately, and whether the Department of Health and Human Services (DHHS) is administering them effectively. The audit did not investigate the clinical effectiveness of individual patient care.
Conclusion
Not all Victorian children and young people with dangerous and debilitating mental health problems receive the services that they and their families need. This can lead to ongoing health problems, increasing the risk that children and young people will disengage from education and employment and be more likely to be involved with human services and the justice system.
Specialist child, adolescent and youth mental health services do improve many of their clients' outcomes, but they do not meet service demand or operate as a coordinated system. This can lead to significant deterioration in the health and wellbeing of some of Victoria's most vulnerable citizens.
DHHS has neither established strategic directions for CYMHS nor set expected outcomes for most of its CYMHS funding. This key issue inhibits service and program managers from realising efficiencies and improvements to service delivery such as working to a common purpose, sharing lessons or benchmarking progress.
Problems with the CYMHS performance monitoring system create oversight gaps for DHHS, which leaves it unable to address significant issues that require a system-level response. These issues include clinically unnecessary stays in inpatient mental health wards, and the admission of children and young people to adult mental health beds.
Health services express that due to DHHS's limited engagement with them, and monitoring systems that do not accurately reflect services' performance, DHHS does not sufficiently understand the CYMHS system and the challenges it faces. DHHS's lack of understanding contributes to a climate of uncertainty and distrust, which inhibits systemic improvement and creates significant variability and inequity in the care that children and young people receive.
DHHS has predominantly taken a one-size-fits-all approach to the mental health system's design and monitoring, which does not adequately identify and respond to the unique needs of children and young people.
Findings
Design of child and youth mental health services
There is no strategic framework to guide and coordinate DHHS or health services that are responsible for CYMHS, which is evident in a range of issues with the CYMHS design:
- DHHS lacks a rationale for the programs and services it funds and there has been a lack of transparency in how some programs and services have been funded.
- Some health services receive funding for programs that technically have ceased, and health services that provide similar activities receive different funding.
- DHHS does not set expectations for service delivery for most funded programs and does not monitor what programs and activities health services deliver.
- DHHS has not adequately considered the geographic distribution of services relative to the population, which creates inequities in service provision.
- There is a confusing mix of age eligibility arrangements across services—some treat young people up to the age of 25 and some up to 18. This is because in 2006, DHHS began increasing service eligibility to 25, but stopped the rollout midway through when the government changed.
- DHHS has not considered CYMHS's particular workforce challenges and needs that can vary from the adult sector, and the recent DHHS mental health workforce strategy does not specifically address CYMHS workforce issues. DHHS advises that the new Centre for Mental Health Learning is now mapping workforce needs, including for CYMHS.
While the cause of this lack of a strategic approach to CYMHS is unclear, high staff turnover in leadership roles and lack of specific performance oversight of CYMHS are likely contributing factors.
DHHS's commitment to reform the mental health funding model into activity‑based funding has not progressed for CYMHS. DHHS has taken no action to address the known problems with transparency and equity in the current funding model.
Monitoring performance, quality and outcomes
DHHS's performance monitoring of CYMHS comprises seven separate systems that are conducted in silos. The different areas that hold responsibility for monitoring within DHHS do not coordinate to identify common or systemic issues, nor do they share the information they collect. The current arrangement offers significantly limited oversight of CYMHS:
- The Mental Health Branch's program meetings discussed CYMHS only once in four years for four health services.
- Key performance indicators (KPI) to measure CYMHS differ from the national mental health performance framework limiting performance benchmarking.
- The two CYMHS KPIs that inform DHHS's quarterly performance discussions with chief executive officers (CEO) only concern services provided to patients who have had an inpatient admission.
- There are no KPIs or monitoring of some significant issues in CYMHS, such as long inpatient stays, accessibility, service coordination or family engagement in care.
The lack of service performance expectations and the limitations of DHHS's performance monitoring systems for CYMHS also hinder its ability to accurately advise government on how this important system performs, or what improvements are needed.
Monitoring the quality and safety of service delivery
The Chief Psychiatrist has legislated responsibilities to monitor service quality and safety in CYMHS. The Office of the Chief Psychiatrist (OCP) has delivered a large program of activities to review and improve service quality across mental health services; however, there has been no attention to the unique issues in CYMHS. Rather, the monitoring is reactive and crisis-driven, with limited focus on systemic issues.
DHHS does not routinely monitor the quality of CYMHS service delivery. Further, DHHS has commissioned two significant evaluations and reviews of new CYMHS services that have not been publicly released, and their findings have not been communicated to the CYMHS that were reviewed. A further nine reviews and analyses that DHHS conducted internally include information about CYMHS that could contribute to broader service quality improvement; however, these have not been provided to health services.
Access for vulnerable populations
DHHS has not identified priority populations or enabled health services to provide priority access to those most in need. Only one of the five audited health services has implemented the Chief Psychiatrist's 2011 guideline to prioritise children in out-of-home care. DHHS has not reviewed the guideline or its implementation since its release. Furthermore, DHHS's data does not record a client's legal status, which means there is no mechanism to reliably identify children in out-of-home care in the CYMHS system.
DHHS has not reviewed its triage scale since its introduction in 2010. DHHS is aware that the triage scale is not optimal for children and young people because it does not consider developmental risks and does not enable prioritisation of access for high-risk population groups.
Service coordination around multiple and complex needs
Young people are routinely getting 'stuck' in CYMHS inpatient beds when they should be discharged, because they cannot access family or carer support and/or services such as disability accommodation or child protection and out-of-home care. DHHS does not monitor this issue of inpatient stays that are clinically unnecessary despite health services having raised it repeatedly.
Current data systems prevent definitive monitoring of clinically unnecessary stays in CYMHS inpatient beds. However, the five audited health services provided to this audit 29 case studies from the prior 12 months that show at least 1 054 bed days used by patients without clinical need to be mental health inpatients. While some of the drivers of this problem are complex social and family issues, DHHS has not taken strategic action to address systemic issues with service coordination that they have the authority to resolve.
Monitoring long inpatient stays would provide a partial indicator of clinically unnecessary stays. DHHS could not explain why it monitors long stays over 35 days for the adult mental health system, but not for CYMHS, despite our data analysis showing that there have been 228 long stays in four health services over three years, of which 107 were children under 18 years.
In one region, there has been a long‐running dispute between two service providers over referral and discharge processes. DHHS has acted to resolve this issue, which caused longer inpatient stays for approximately 300 adolescents per year, by advising the health services to meet monthly and to escalate matters that cannot be resolved to the Chief Psychiatrist.
Clients with intellectual or developmental disabilities complicated by mental health problems account for many long and/or clinically unnecessary inpatient stays. DHHS has not responded adequately to CYMHS's reports about the service gap for young people with dual disability and the significant negative impacts on CYMHS's resources, workforce and the young people and their families.
DHHS and the Department of Justice and Community Safety's (DJCS) shared Multiple and Complex Needs Initiative (MACNI) provides case management for people aged 16 and over with mental illness, complex needs, and dangerous behaviours. Eligibility criteria are too narrow and processes too slow for this service to assist CYMHS with complex clients who are 'stuck' in inpatient units.
A $5.5 million pilot project that DHHS funded three years ago, and another CYMHS's independent service development, have lessons and resources that DHHS has not shared with other CYMHS. DHHS has not responded to either of these services' recommendations to address gaps in accommodation and service coordination for these young people, nor taken any action to support other CYMHS with providing services to clients with dual disability who have complex needs.
Recommendations
We recommend that the Department of Health and Human Services:
- in conjunction with child, adolescent and youth mental health services and consumers, develop strategic directions for child, adolescent and youth mental health services that include objectives, outcome measures with targets, and an implementation plan that is supported by evidence‑based strategies at both the system and health service levels (see Section 2.2)
- when implementing the six recommendations from the VAGO audit Access to Mental Health Services, ensure that the needs of children, adolescents and young people as well as child, adolescent and youth mental health services are considered and applied, wherever appropriate (see Section 1.4)
- establish and implement a consistent service response for 0–25 year-olds in regional Victoria that need crisis or specialised support beyond what their local child, adolescent and youth mental health services' community programs can provide, including reviewing the extent to which the six funded regional beds are able to provide an evidence-based child and adolescent service (see Sections 2.4 and 3.2)
- establish and implement a transition plan towards achieving a consistent service response for 19–25 year-olds with moderate and severe mental health problems (see Section 2.5)
- develop and implement a child, adolescent and youth mental health workforce plan that includes understanding the specific capability needs of the sector and specifically increasing capabilities in the area of dual disability, that is, intellectual or developmental disabilities complicated by mental health problems (see Section 2.7)
- refine, document and disseminate the performance monitoring approach for child and youth mental health services so it consolidates current disparate reporting requirements and includes:
- measures that allow monitoring of long inpatient stays, priority client groups, clinical outcomes and accessibility of child and youth mental health services
- introducing quality and safety measures of child and youth mental health services community programs in the Victorian Health Services Performance Monitoring Framework
- the role of the Chief Psychiatrist in performance monitoring, and how the information it receives from mandatory reporting informs the Department of Health and Human Services' performance monitoring
- documenting in one place all reporting requirements for child and youth mental health services from all areas of the Department of Health and Human Services, including administrative offices Safer Care Victoria and the Victorian Agency for Health Information
- how the Department of Health and Human Services will respond to performance issues (see Sections 3.2 and 3.6)
- ensure that six-monthly mental health program meetings occur and information received is consolidated to identify systemic and persistent issues (see Section 3.4)
- initiate negotiations with the Department of Treasury and Finance during the state budget process to ensure that Budget Paper 3 performance measures include monitoring of child, adolescent and youth mental health services (see Section 3.6)
- disseminate evaluations and reviews of child, adolescent and youth mental health service projects and services to all child, adolescent and youth mental health service leaders (see Section 3.7)
- formally respond to all recommendations made in the 2016 review of the role of the Chief Psychiatrist and advise the Minister for Mental Health on intended actions (see Section 3.7)
- in consultation with health services, ensure that the Chief Psychiatrist's guidelines and directions are effectively communicated to those responsible for their implementation in child, adolescent and youth mental health services and that their implementation is supported and monitored (see Section 3.7)
- benchmark the performance of child, adolescent and youth mental health services in Victoria at the system level against other jurisdictions, and national and international targets, and report the findings and opportunities for improvement subsequently identified in the Mental Health Annual Report (see Section 3.8)
- ensure that the data that the Department of Health and Human Services and/or health services need to collect about child and youth mental health services for their reporting and monitoring obligations, including the outcome measures and targets developed through Recommendation 1, is consistent with what is collected and recorded in the Client Management Interface database and develop a single and comprehensive source of guidance and business rules about data reporting requirements (see Section 3.9)
- update the triage scale and process so it is developmentally appropriate for children, adolescents and young people, and considers how triage can be provided at peak periods of demand such as evenings and weekends (see Section 4.2)
- ensure the registration forms that the Department of Health and Human Services issues to health services can record a child, adolescent or young person's legal status with regards to guardianship, out-of-home care, and restrictive interventions or compulsory treatment under the Disability Act 2006, that the information can be entered into central databases, that business rules exist for doing so and data entry is monitored to ensure it is occurring (see Section 4.2)
- provide written guidance to child and youth mental health services' leaders about both the Department of Health and Human Services' Complex Care Panels and the Multiple and Complex Needs Initiative, which includes how to refer clients to each, how to contact the necessary staff in each Department of Health and Human Services geographic area for information and advice, which clients are eligible for each, and is updated at least annually (see Section 4.3)
- consider establishing a High-Risk Complex Care Child and Youth Panel, with executive representation from out-of-home care, disability services, and mental health areas of the Department of Health and Human Services, with remit to:
- allow health services to rapidly escalate cases to the panel when a local service response is not meeting a young person's needs, to prevent a clinically unnecessary inpatient stay that may cause deterioration of the young person's health and wellbeing
- identify and address service gaps and service coordination challenges that are contributing to clinically unnecessary inpatient stays
- liaise with the National Disability Insurance Agency, as required (see Section 4.4)
- create a channel for the Chief Psychiatrist to independently brief the Minister for Mental Health or the Secretary, if they deem it necessary (see Section 4.4)
- establish and implement a consistent service response for 0–25 year-olds who have intellectual or developmental disabilities and moderate to severe mental health problems (see Section 4.5)
- establish a mechanism for operational and clinical leaders of all child, adolescent and youth mental health services to collaborate with each other and with the Department of Health and Human Services to improve service response consistency, and strengthen pathways between services for clients and families, including reviewing catchment boundaries and access to specialised statewide programs (see Section 4.5).
Responses to recommendations
We have consulted with DHHS, Albury Wodonga Health (AWH), Austin Health, Eastern Health, Monash Health and the Royal Children's Hospital (RCH) and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report to those agencies and asked for their submissions or comments. We also provided a copy of this report to the Department of Premier and Cabinet.
DHHS provided a response. The following is a summary of its response. The full response is included in Appendix A.
DHHS accepted each of the 20 recommendations, noting that implementation of the recommendations will be informed by the outcomes of the Royal Commission into Mental Health, particularly recommendations relating to system design. DHHS will develop strategic directions and refine the performance monitoring approach for services, share reviews and evaluations, update triage and registration processes, provide guidance around complex care panels, consider establishing a High-Risk Complex Care Child and Youth Panel, establish a mechanism for health services to collaborate and create a means for the Chief Psychiatrist to independently brief the Secretary or Minister for Mental Health.
1 Audit context
Mental health problems are the most common health issues facing young people worldwide, according to the Global Burden of Disease Study 2017. Three-quarters of all mental health problems manifest in people under the age of 25. One in four Australians aged 16–24 years will experience mental health problems in any given year, while 2.1 per cent of Australian children and adolescents have a severe mental health problem and a further 3.5 per cent have moderate mental health problem. One in 10 Australian adolescents (10.9 per cent) have deliberately injured themselves, and each year one in 40 (2.4 per cent) attempt suicide.
The Australian Government's national survey of child and adolescent mental health defines the most common and disabling mental health problems that children and young people in Australia experience as:
- major depressive disorder
- attention-deficit/hyperactivity disorder
- conduct disorder
- social phobia
- separation anxiety
- generalised anxiety
- obsessive-compulsive disorder.
Figure 1A summarises the most recent data on children and young people's mental health problems. This data references various years and sources, and highlights that some children and young people are at higher risk of having a mental health problem. For example, children and young people from socio‑economically disadvantaged families have higher rates of mental health problems. Children living in out-of-home care experience two to five times higher rates of mental health problems and more than double the rate of serious suicide attempts.
Figure 1A
Prevalence of mental health problems in Australian children and young people
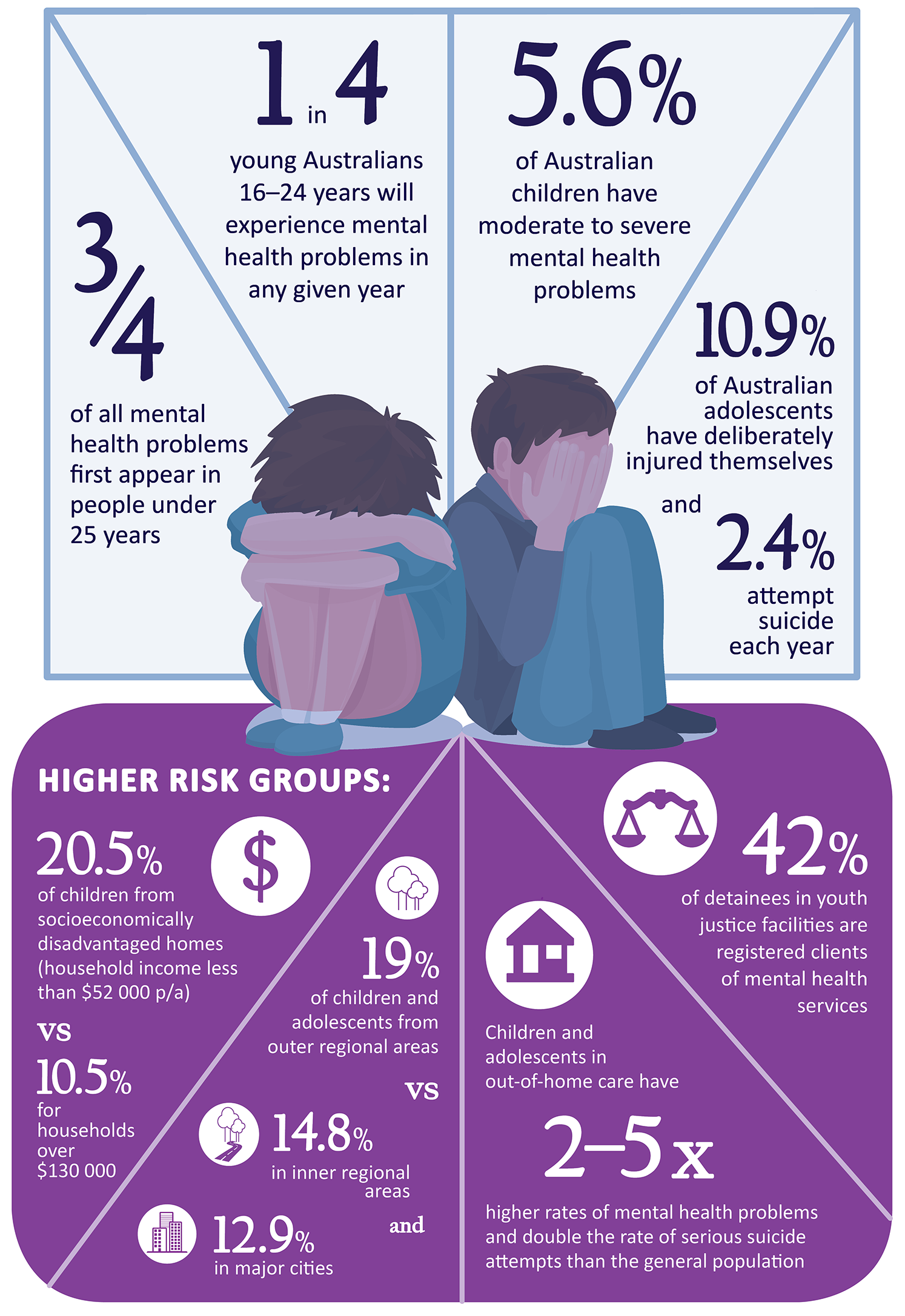
Note: A serious suicide attempt is a suicide attempt that required medical treatment.
Source: VAGO with information from Lawrence D, et al, (2015), The Mental Health of Children and Adolescents: Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing; Department of Health, Canberra; Sawyer, M. et al (2007), 'The mental health and wellbeing of children and adolescents in home-based foster care', Medical Journal of Australia, 186:4; Kessler RC, et al, (2005), Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication; Australian Institute of Health and Welfare, (2007), Young Australians: their health and wellbeing; DHHS (2018), Mental Health 2018–2023 Services Strategy analysis – Draft, Linkage, Modelling and Forecasting Section.
Services used by children and young people with mental health problems
|
In 2017–18, there were 11 945 registered clients of CYMHS, 331 058 contacts and 2 014 inpatient stays. |
For children and young people, intervention early in life and at an early stage of mental health problems can reduce the duration and impact of the problems. Services that recognise the significance of family and social support are particularly important for children and young people. These principles informed the Australian Government's National Mental Health Plan, published in 2003.
A national survey by the University of Western Australia and Roy Morgan Research for the Australian Government in 2013–14 (published in 2015) on mental health of children and adolescents estimated that 3.3 per cent of Australian children and young people with mental health problems access clinical mental health services. However, 12 per cent with severe mental health problems do not access any services, including those provided through schools, general practitioners, telephone helplines or online. For children and young people with moderate or severe mental health problems, this figure rises to 27.5 per cent. Service use varies by age as well as the severity of problems, as shown in Figure 1B.
Figure 1B
2015 Australian Government report of service use by 4–17 year-old Australians with mental health problems by age group and severity of problem
Note: Services include any service provided by a qualified health professional regardless of where that service was provided including in the community, hospital inpatient, outpatient and emergency, and private rooms; school or other educational institution; telephone counselling; online services that provided personalised assessment, support or counselling.
Source: VAGO based on information from the Australian Government's 2015 report, The mental health of Australian children and young people: Report on the second Australian child and adolescent survey of mental health and wellbeing.
1.1 Agency roles and responsibilities
Department of Health and Human Services
DHHS is responsible for ensuring the delivery of good-quality health services to the community on behalf of the Minister for Health and the Minister for Mental Health. DHHS plans services, develops policy, and funds and regulates health service providers and activities that promote and protect the health of Victorians.
The Secretary of DHHS is responsible for working with, and providing guidance to, health services to assist them on matters relating to public administration and governance.
The Mental Health Branch of DHHS has 84 staff who carry out the duties prescribed to the Secretary.
The Chief Psychiatrist
The Secretary of DHHS appoints a Chief Psychiatrist, who has legislated responsibilities under the Victorian Mental Health Act 2014 (the Act) for:
- providing clinical leadership and advice to public mental health services
- promoting continuous improvement in quality and safety
- promoting the rights of persons receiving treatment
- providing advice to the minister and the Secretary about the provision of mental health services.
The Chief Psychiatrist is subject to the general direction and control of the Secretary of DHHS in the exercise of their duties, functions and powers under the Act. The Secretary has specific powers to request the Chief Psychiatrist take action, for example, to conduct a clinical audit. The Chief Psychiatrist also has statutory obligations to the Secretary to provide a report of any investigation undertaken. Operationally, the Chief Psychiatrist reports to DHHS's Director of Mental Health.
|
Clinical mental health services targeting people up to 18 years only are known as child and adolescent mental health services (CAMHS) and those who have expanded their models to 0–25 years refer to themselves as child and youth mental health services (CYMHS). The subtle difference in terminology creates frequent confusion in discussions around these services. In this report, 'child and youth mental health services (CYMHS)' is used to refer to all clinical services that the Victorian Government funds to support children, adolescents and youth aged 0–25 years who have moderate to severe mental health problems, and includes services named CAMHS. |
Child and Youth Mental Health Services
CYMHS support children and adolescents through a mix of community-based or outpatient programs and inpatient treatment in hospitals, as well as a small number of community residential programs. They also provide education, upskilling and leadership on managing mental health problems to the services and agencies that care for children and young people, which includes schools, child protection and disability services. Health services manage CYMHS and are responsible for ensuring compliance with relevant legislation, regulations and policies.
DHHS provides $11.4 million per year for an early psychosis program to target young people aged 16–25 who are experiencing their first episode of psychosis. The program provides case management, medication, psychological therapies, social, educational and employment support, and family work.
In addition to accessing CYMHS, some young people in Victoria use adult mental health services because eligibility for the adult stream commences at 16 years. DHHS funds specialist perinatal mental health services, mother and baby units, and a statewide program that aims to reduce the impact of parental mental illness on family members through the adult mental health system. While these programs directly impact children and young people, this audit does not examine them.
Mental health problems have many causes, including abuse and neglect in childhood, developmental disorders, and physical disability. Children and young people who access clinical mental health services commonly also need services such as child protection or disability support. Coordinating these different services is an important and complex part of best-practice care for many children and young people with mental health problems.
Figure 1C shows one CYMHS's description of the service system for its clients and their role within it.
Figure 1C
Other services that clients of CYMHS routinely require
Source: RCH response to DHHS's 10-Year Mental Health Plan, 2016.
Commonwealth-funded services
|
There are 27 headspace centres around Victoria that offer enhanced primary care services, which include mental health, physical and sexual health, and life skill support around work and study in an accessible, youth-friendly environment. |
Children and young people can access Commonwealth-funded services to support their mental health needs. The Australian Government funds Primary Health Networks (PHN), which provide early-intervention services for young people with, or at risk of, severe mental illness, alongside its funding of primary care through general practitioners and headspace centres. Victoria has six PHNs that provide 28 different services. CYMHS are involved with supporting some Commonwealth-funded initiatives. Many CYMHS have active roles in managing and supporting their local headspace centres.
Workforce challenges
Attracting, training and retaining a sufficient and appropriately skilled mental health workforce, and making mental health services safe places to work, is a major challenge for health services and DHHS.
The Royal Australian and New Zealand College of Psychiatrists' (RANZCP) review of workforce issues, which it publicly reported in 2018, noted a shortage of Victorian child and adolescent psychiatrists (CAP). Victoria has 31 CAP training positions, of which two are in regional areas. RANZCP says that Victoria urgently needs 12 additional CAP training positions.
A 2016 study by the University of Melbourne and the Health and Community Services Union, published in the International Journal of Mental Health Nursing, found that 83 per cent of 411 surveyed staff in Victoria's mental health workforce had experienced violence in the prior 12 months, mostly comprising verbal abuse (80 per cent) followed by physical violence (34 per cent) and bullying (30 per cent). One in three victims of violence rated themselves as being in psychological distress, 54 per cent of whom reported being in severe psychological distress. The survey did not report on these matters specific to CYMHS.
1.2 Relevant legislation
In 2014, the Act came into effect. The Act prescribed many changes to the mental health system including ensuring that treatment is provided in the least restrictive way possible.
Under the Act, mental illness is defined as 'a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory'.
The Act mandates that health services report to the Chief Psychiatrist on the use of electroconvulsive treatment (ECT), results of neurosurgery, the use of restrictive interventions, and any deaths that meet the Coroners Act 2008's definition for a reportable death.
The Act sets out roles and responsibilities for the Chief Psychiatrist and the Secretary of DHHS.
The 'Mental Health Principles' in the Act state that:
Children and young persons receiving mental health services should have their best interests recognised and promoted as a primary consideration, including receiving services separately from adults, whenever this is possible.
The Act does not specify an age grouping for children and young persons to which this principle would apply.
1.3 Why this audit is important
There have been considerable changes to the environment in which CYMHS operate in recent years. The types and complexity of mental health problems that children and young people seek support for is increasingly challenging for health services. Demand for services is growing rapidly due to interconnected factors including reduced stigma around mental health problems, and more youth-friendly access points for young people to seek help, such as headspace centres.
This is the first Victorian Auditor-General's Office (VAGO) audit of Victoria's child and youth mental health system, and there has been no other substantial public, external review of this topic. VAGO's 2019 audit Access to Mental Health Services found that DHHS has not done enough to address the imbalance between demand for, and supply of, mental health services in Victoria. VAGO made six recommendations to DHHS about investment planning, monitoring access, funding reforms, catchment boundaries, and internal governance.
During VAGO's audit, the Victorian Government established a Royal Commission to inquire into mental health, which is due to provide an interim report to the Governor of Victoria in November 2019 and a final report in October 2020. The terms of reference released in February 2019 give the Royal Commission an extensive brief to report on how to improve many matters in the mental health system, including access, governance, funding, accountability, commissioning, infrastructure planning, workforce, and information sharing.
The Productivity Commission is currently conducting an inquiry into The Social and Economic Benefits of Improving Mental Health, which will focus on the largest potential improvements, including for young people and disadvantaged groups. This audit adds a detailed review of this particular part of the mental health system to these larger and broader inquiries.
1.4 What this audit examined and how
The objective of this audit was to determine whether child and adolescent mental health services effectively prevent, support and treat child and youth mental health problems. We considered whether the services are appropriately designed and whether DHHS administers them effectively. The audit focused on clinical mental health services for young people with moderate to severe mental health problems.
We selected five health services for the audit, alongside DHHS, in order to sample the varied services in Victoria's devolved health system:
- AWH
- Austin Health
- Eastern Health
- Monash Health
- RCH.
The audit focused on current service delivery, with some reference to significant changes over the past three to five years.
We conducted our audit in accordance with section 15 of the Audit Act 1994 and ASAE 3500 Performance Engagements. We complied with the independence and other relevant ethical requirements related to assurance engagements. The cost of this audit was $530 000.
In accordance with section 20(3) of the Audit Act 1994, unless otherwise indicated, any persons named in this report are not the subject of adverse comment or opinion.
1.5 Report structure
The remainder of this report is structured as follows:
- Part 2 examines the design of CYMHS.
- Part 3 examines how DHHS monitors performance, quality and outcomes of child and youth mental health services.
- Part 4 examines access and coordination of care for the most vulnerable and complex clients.
2 Design of child and youth mental health services
The Victorian Government funds 17 health services to provide clinical services to children or young people with moderate to severe mental health problems.
In 2017–18, clinical mental health services in Victoria treated 11 945 children and young people up to the age of 18 years—an 11.5 per cent increase on the previous year—and admitted 2 014 to hospital, a 9.8 per cent increase. DHHS was not able to provide any information about young people aged 19–25 years in either the adolescent or adult mental health system.
There are six CYMHS in metropolitan Melbourne and eight in regional Victoria, as shown in Figure 2A. Clients must attend the CYMHS located in the catchment where they live, unless they require a specialised service that is not provided or available in their own catchment. Regional CYMHS are attached to one of four metropolitan services as their primary referral option for specialist or inpatient support that is not available locally, as illustrated by Figure 2A.
Three provide limited, specialised services to children and adolescents such as forensic services and treatment of eating disorders. The remaining 14 provide a general service, often alongside a suite of specialised programs. Eight of these provide inpatient services, of which two include inpatient services specifically for children under 12 years of age. One of these services is specifically 'youth‑focused', providing both inpatient and community services to 15–24 year-olds in its catchment area.
Figure 2A
Location of CYMHS and their partner agencies for inpatient and specialised service referrals
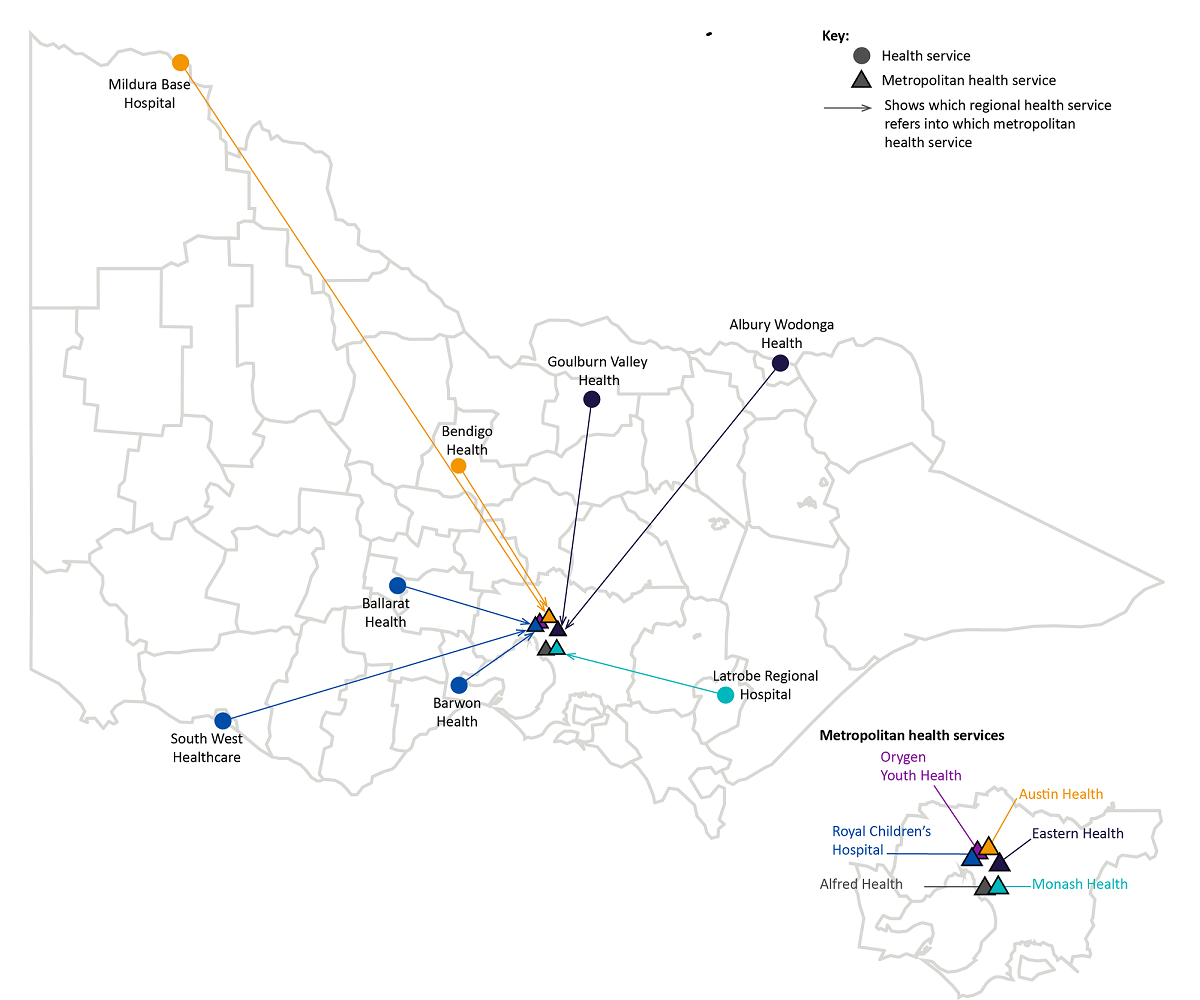
Source: VAGO mapping of DHHS information.
2.1 Conclusion
DHHS has not provided the strategic leadership necessary to effectively plan, fund and manage CYMHS. Consequently, the system consists of a collection of fragmented and overstretched health services. DHHS has created a system that cannot effectively work together even when client need requires it.
DHHS has not met the obligations of its role as a system manager—to set clear strategic directions and service expectations for CYMHS, to establish a transparent and equitable funding model, and to ensure service design supports the infrastructure and service accessibility that children and young people need. Where health services have made innovative attempts to improve services, there are no mechanisms for sharing or collaborating.
This lack of leadership and strong communication and collaboration with the CYMHS sector has created a culture of distrust, and has impeded knowledge sharing among health services and between health services and DHHS. All of this results in a service system that is not meeting the needs of some vulnerable children and young people.
2.2 Strategic direction
In 2015, DHHS published Victoria's 10-year Mental Health Plan (the 10-year plan), which is a high-level framework for mental health service reform. There is one action in the plan that is relevant to child and youth clinical mental health services:
strengthening collaboration between public specialist mental health services for children and young people and paediatricians, other social and community services and schools
The 10-year plan does not provide a strategic framework for child and youth mental health. DHHS formed the Mental Health Expert Taskforce (the taskforce) to advise on the 10-year plan and its implementation. The taskforce identified child and youth mental health as one of the highest priority areas for action; however, no plan was developed on what that action should be.
DHHS's Clinical Mental Health Services Improvement Implementation Plan—endorsed internally in December 2018—commits to developing a 'child and youth service framework' with immediate priorities identified by June 2019 and the framework complete by June 2020. DHHS has not progressed this work and has not determined the framework's scope, purpose or how it will be developed. In early 2019, DHHS took a decision to not progress this work until the Victorian Government's Royal Commission into Mental Health concludes.
During the audit, DHHS became aware of a proposal by RCH for a strategic direction for CYMHS, which calls for bringing all Victorian CYMHS together into a network that undertakes shared work on quality improvement, workforce development and practice innovation. The proposal identified nine priority areas for this work, which are:
- development with consumers and carers of a central dataset that monitors clinical needs, accessibility, collaboration with child and family service providers, and outcome evaluation to allow benchmarking and collaboration across mental health services
- workforce development
- establishing a research forum
- clinical pathways between services
- policy directions to specify the role of public mental health services
- expanding targeted interventions for dual disability, gender dysphoria, eating disorders, Aboriginal and Torres Strait Islander children, trauma, children in out-of-home care, and refugees
- clinical guidelines commencing with psychopharmacology, dual disability, and children involved with child protection
- implementation research
- engaging with schools.
Given our observations of a fragmented system and the lack of strategic direction, RCH's proposal has merit. DHHS should consider this proposal and provide a response to RCH at the earliest opportunity.
The only evidence that DHHS provided strategic guidance to CYMHS about how they should operate is the following statement in the Clinical Specialist Child Initiative program guidelines issued in 2016:
It is expected that the new, expanded and existing services will work together to form a comprehensive response to the mental health needs of children aged 0–12. It is expected that the local operation of these services will interlink and not be delivered in isolation.
Despite giving these directions, DHHS has not taken action to enable services to achieve them and it has not monitored progress.
There has been significant change in the position of Director of Mental Health at DHHS. In the three years from 2016 to 2018, eight people have held the role, as illustrated in Figure 2B. Three permanent appointments covered 15 months out of the three years. Five other individuals held the role in acting positions, and two of the permanent appointees began their tenure with temporary secondments. For 537 days, or 49 per cent, of the three years, there was a temporary appointee in the role.
DHHS advises that there has not been instability in the leadership of the Mental Health Branch because the same people rotated through the temporary appointments, which enabled continuity. However, the temporary, albeit rotational, leadership of the branch likely impacts its ability to maintain a clear long-term vision, and make and follow through on decisive actions.
Figure 2B
Individuals who have held the Director of Mental Health role at DHHS in 2016–18, by month
Note: Each colour represents a different individual, with an 'A' or a 'P' indicating whether that individual was in an acting or a permanent role at that time.
Source: VAGO analysis of information supplied by DHHS from 'SAP Organisational Management' database, December 2018.
It is also unclear what resources are dedicated to DHHS's oversight and monitoring of CYMHS, as this is predominantly embedded within positions responsible for broader performance monitoring of individual health services and/or the mental health system more generally. There is one position within the Mental Health Branch whose responsibilities include the 'child and adolescent portfolio' alongside being the lead contact for monitoring performance for several health services. Portfolio responsibilities include program development, service planning and system oversight. These portfolio responsibilities form approximately 20 per cent of the workload in the position, dependent on other responsibilities.
2.3 Funding model
DHHS has not acted to address the transparency and equity problems with the current funding model, and there has been no progress towards introducing activity-based funding for CYMHS.
Mental health is funded through a block funding model, where a sum of funding is provided by DHHS for the health service to deliver an agreed number of services—a number of 'beds' for inpatient services and 'service hours' for community-based services.
DHHS determines each year's funding allocation by considering the previous year's funding, some analysis of services provided in the previous year, and any new government commitments in the State Budget.
As noted in a 2018 report to DHHS's Audit and Risk Committee, Hospital Budget Governance Framework – Internal Audit Report, there is a 'medium-level' risk that models of funding that are not activity-based have 'a lack of governance and documentation of decisions taken'. Figure 2C shows the funded units that are relevant to CYMHS.
Figure 2C
Mental health—funded units applicable to clinical bed-based services 2018–19
|
Service element |
Funded unit |
All health services ($) |
|---|---|---|
|
Admitted care |
||
|
Acute Care—child/adolescent, adult, aged(a) |
Available bed day |
712.00 |
|
Youth Prevention and Recovery Centre |
Available bed day |
600.13 |
|
Clinical community care |
||
|
Ambulatory |
Community service hour |
402.58 |
Note: (a) Supplement grant provided to support the acute care unit price.
Source: VAGO based on DHHS Policy and Funding Guidelines 2018–19.
DHHS's internal analysis shows that its funding covers 65 per cent of the costs of inpatient mental health beds while other health services are funded at more than 80 per cent of the actual cost. Audited health services confirmed that they 'cross-subsidise' from their community CYMHS funding to cover the costs of meeting demand for their inpatient beds.
In addition to the 'available bed day' funding unit, Monash Health receives $1 092 774 per year labelled 'child bed supplement' in DHHS's funding system. DHHS advises that the extra funding is to support Monash Health to provide inpatient services for children. However, we found that Austin Health does not receive this supplement despite also providing inpatient beds for children. DHHS's explanation for the funding discrepancy is that each health service provides a different model of care and that if Austin Health transitioned to the same model as Monash Health, it would also receive the supplement. DHHS has not communicated this to Austin Health, which demonstrates an example of the risk raised in the internal audit report of a lack of transparency and clarity around block funding arrangements.
DHHS provides a total of $9.3 million for eating disorder services to seven health services. As we were unable to determine what proportion of this funding is spent in CYMHS, we have only included eating disorder funding for RCH in our funding analysis as this health service only treats children and young people.
Activity-based funding is used for most other services provided through Victorian hospitals—the amount paid reflects a service's complexity and cost with some additional loadings for especially complex and high-risk patient groups. In its Policy and Funding Guidelines 2018–19, DHHS states its commitment to introducing an activity-based funding model, also noting its benefits:
There will be a focus on developing a new mental health funding model for specialist community-based adult mental health services in 2018–19. The new model will link funding to the delivery of services and will provide different levels of funding depending on the complexity of the consumer needs. The reforms, and related and revised performance and outcomes monitoring, will improve the transparency and drive improvements in services' performance and consumer outcomes.
During the audit, DHHS was in the early stages of planning a trial of activity-based funding for one adult mental health program. DHHS advises that in future, it will consider using activity-based funding for CYMHS.
2.4 Services funded
DHHS does not have a transparent and clear rationale for the suite of programs and services that it funds, or how it determines the distribution of funding across programs, regions and health services.
DHHS specifies the number of inpatient beds for children and adolescents, but for community or outpatient programs it provides guidance only on how health services should use the funding for two of the 14 funded programs. Health services must deduce what DHHS expects them to deliver and develop their own rationale for what they will deliver with the funding.
In 2018–19, DHHS is providing $127.7 million to Victorian health services for a range of clinical mental health services targeted at children and young people with mental health problems, which is a significant increase in funding. In 2016–17, the Victorian Government committed $73.8 million over four years, primarily to increase accessibility to CYMHS for children under 13 years. In the same year, the government also provided $59 million to support the construction of a new facility to house Orygen, the National Centre of Excellence in Youth Mental Health, which opened during this audit, in Parkville.
The programs delivered by each of the 17 funded health services vary significantly. Four receive more than $15 million per year each for a large array of different programs and services. A fifth receives $7.7 million for services specifically targeted at young people aged 15–24 years. Nine are in regional areas with either no inpatients or two inpatient beds and funding between $2 and $5 million per year each. Funding by service type and health service is shown in Appendix B.
Each service has different client eligibility arrangements—some accept children and young people up to the age of 25 years, while others only accept those up to 18 years. Eligibility also varies by age for specific programs provided within CYMHS. In one region, the client's age determines whether the same service that provides inpatient care will provide ongoing care or whether they need to be referred to another service in the catchment.
DHHS currently distributes funding across seven different types of services, as shown in Figure 2D.
Figure 2D
Distribution of CYMHS funding by type of service
|
Type of services |
Proportion of total funding (%) |
|---|---|
|
Community-based assessment and treatment services |
43.9 |
|
Inpatient services |
25.6 |
|
Other specialised community programs |
14.6 |
|
Early psychosis services |
8.9 |
|
Eating disorders specialised services |
1.1 |
|
School outreach program |
5.0 |
|
Autism coordinators |
0.8 |
Source: VAGO, with information provided by DHHS.
Inpatient beds
DHHS determines how many inpatient mental health beds each health service provides and whether these beds are for children (0–12 years), adolescents (13–18 years) or young people (15–25 years). DHHS could not provide a clear rationale for how it determines the location and number of these beds, and there is no evidence that DHHS consults with CYMHS when making these decisions.
Figure 2E shows DHHS distribution of inpatient mental health beds for children, adolescents and young people.
Figure 2E
Number of inpatient mental health beds for children, adolescents and young people funded by DHHS
|
Health service |
Children aged |
Adolescents aged |
Young people aged |
Funding |
|---|---|---|---|---|
|
Monash Health |
8 |
15 |
* |
7.07 |
|
Austin Health |
12 |
11 |
5.98 |
|
|
Melbourne Health (as auspice of Orygen Youth Health) |
16 |
4.16 |
||
|
RCH |
16 |
4.16 |
||
|
Eastern Health |
12 |
3.12 |
||
|
Ballarat Health |
2 |
0.52 |
||
|
Latrobe Regional Hospital |
2 |
0.52 |
||
|
Ramsay Healthcare (as managers of Mildura Base Hospital) |
2 |
0.52 |
||
|
Total |
20 |
60 |
16 |
26.06 |
Note: * Monash Health operates a youth inpatient service for 18–25 year-olds that is not included in this table because DHHS does not fund it as part of its child and youth mental health funding. Monash Health created the dedicated youth service as part of its adult mental health service.
Source: VAGO from DHHS Policy and Funding Guidelines 2018–19 and DHHS website.
There are complex catchment arrangements across the system. DHHS has acknowledged the catchment arrangements are problematic because they are not aligned with the catchments that other government services use. Clients must attend the CYMHS located in the catchment area they live in, unless they require a specialised service that is not provided or available in their own catchment. Figure 2A shows how regional CYMHS are attached to one of four metropolitan services as their primary referral option for specialist or inpatient support. DHHS has not yet taken action to improve or resolve the catchment issues.
If a child or young person urgently requires inpatient care, health services may admit them 'out-of-area' for care at a CYMHS in another catchment, when one or more of the following occurs:
- Their local CYMHS does not have an available bed.
- Their local CYMHS does not provide inpatient services.
- The health service that their local CYMHS refers to for inpatient services does not have an available bed.
These scenarios can require a child or young person to be transferred to a health service located several hours from their home. Once treatment has ended, the child or young person is 'repatriated' to the CYMHS within their catchment for follow-up care. Health services do not have a consistent process for repatriation. Each repatriation varies depending on the clinical needs of the child or young person, and the availability of their catchment CYMHS service to engage in the repatriation process. Given services are stretched across all CYMHS, it can be difficult for health services to effect repatriations effectively and efficiently.
Children and young people in adult inpatient beds
There are systemic conflicts around inpatient services for young people, which DHHS acknowledges, but has not acted to address:
- The Act says 'children and young people' should receive separate services from adults wherever possible. The Act does not define the age of 'young people' though this terminology is commonly understood to include people aged approximately 18–25 years of age.
- DHHS does not define eligibility for CYMHS adolescent inpatient beds beyond a description on its website stating that 'CAMHS inpatient units Ö mostly admit young people aged 13–18 years' and that RCH admits young people 13–15 years and Orygen Youth Health 15–24 years.
- Audited health services received guidance from DHHS that eligibility for CYMHS adolescent beds ceases on a young person's 18th birthday, but they can use the beds for 18-year-olds if clinically appropriate—there is no written evidence of this guidance.
- DHHS only funds dedicated inpatient beds for young people aged 18–24 in one metropolitan catchment.
- DHHS defines eligibility for adult inpatient beds as 16 years and over.
DHHS has never analysed the use of adult inpatient beds for children and adolescents and does not monitor the issue despite it being clinically inappropriate, inconsistent with legislation, and a potential indicator of significant demand pressures on CYMHS.
When we analysed inpatient admissions data over three years (2016–18) for our audited health services, we found young people admitted to adult mental health services as young as 13 years, as shown in Figure 2F.
RCH is excluded from this table because it is a paediatric hospital. Monash Health was also excluded as the data could not distinguish between inpatient wards and Youth Prevention and Recovery Centres (Y-PARC) that are designed for 16–25 year-olds.
Figure 2F
Adolescents and young people in adult mental health services at audited health services during 2016–18, by age at admission
Note: This assumes that all 18–25 year-olds at Austin Health and Eastern Health are in their adult service, but a small but undetermined number are known to be admitted to adolescent beds based on clinical assessments of individual need and availability of beds.
Source: VAGO analysis of Client Management Interface data provided by five audited health services. See Appendix D for data analysis scope and methodology.
Austin Health and Eastern Health had 2 154 admissions of young people aged 18–25 years in the three years between 2016 and 2018. These health services routinely place these patients in adult mental health beds because their age limit for adolescent beds is a child's 18th birthday.
Monash Health recorded 3 131 admissions of young people aged 18–25 years; however, they have established a separate youth ward of 25 beds within their adult service and they also have a Y-PARC community residential facility. It was not possible through our data analysis to confirm that all of the 18–25 year-olds were treated in the separate youth ward or the breakdown between the Y-PARC and the hospital inpatient services.
Monash Health's service development work to create a youth ward within an adult service without dedicated resources is an important initiative. DHHS should review and monitor this youth ward to identify opportunities to share the learnings with other CYMHS and inform service development that could increase compliance with the Act's principle to provide services for young people separate to adults wherever possible.
AWH admitted 403 mental health inpatients aged 0–25 years to its adult mental health ward. This included 86 admissions for adolescents aged 13–18 years. Some were admitted more than once. Sixty-nine individual adolescents had inpatient admissions to an adult facility.
Our analysis considered four health services. It is likely that admission of children and young people to adult mental health beds has occurred in other health services, particularly in regional and rural areas. This warrants broader review by DHHS.
During this audit, AWH undertook a snapshot audit of 13 adolescents admitted to its adult inpatient facility and found that the reasons for admission across the different cases included:
- a family who refused a referral to the metropolitan adolescent inpatient unit due to the costs and time of travel involved, including a prior experience of having to arrange return transport without assistance
- a patient who was scheduled for transfer to the metropolitan adolescent unit the following day, and spent one night 'contained' in the adult mental health bed while transport was arranged
- a patient's residence being out-of-area for AWH CYMHS, but who was admitted after a crisis assessment
- the crisis assessment team admitting a patient with no explanation in the notes of why a referral to the metropolitan adolescent service was not considered.
AWH has committed to investigate these adolescent admissions to the adult inpatient unit to understand and address the underlying issues.
DHHS has not reviewed, and does not monitor, the effectiveness and appropriateness of transfers between regional areas and metropolitan CYMHS and has not taken action to understand or alleviate the challenges this poses for both families and health services.
Access to inpatient beds for regional areas
At three regional health services, DHHS provides funding for two CYMHS inpatient beds. DHHS has not reviewed the use of these beds and does not monitor the extent to which CYMHS allocate them to children and young people. It would be challenging for the three regional health services to run a separate, dedicated child and adolescent inpatient service given the small number of CYMHS-funded beds. Not only do the beds need to be physically separate from their adult mental health service to meet the principle of care in the Act, but the clinical staff also need to be trained in the child and youth mental health specialty.
Given the significant demand pressures that we reported in our March 2019 audit Access to Mental Health Services together with the workforce challenges of attracting sufficient child and adolescent psychiatrists to regional areas, as described in Sections 1.2 and 2.7, it is unrealistic to expect these services to deliver appropriate CYMHS inpatient services. There is a high risk that the beds are used for adult mental health patients instead, which could mean that CYMHS funding is diverted from children and young people. In 2018–19, these beds represented $1.56 million of the ongoing CYMHS funding.
All regional CYMHS, including those with their own inpatient bed funding, are designated one of four metropolitan services to refer their clients to if they require inpatient or other specialised care that is not available locally, as shown in Figure 2A. For example, AWH CYMHS refers to Eastern Health's CYMHS.
Over the three years between 2016 and 2018, our analysis of health services' data shows that Eastern Health and AWH shared 59 clients.
AWH believes it may have enough demand for its own CYMHS inpatient service. As shown in Figure 2G, AWH had 86 admissions for adolescents aged 13–18 years and a further 317 admissions for young people aged 19–25 years during the three years between 2016 and 2018. In addition, AWH keeps a manual record of transfers to other health service inpatient units, which shows 44 transfers for admission elsewhere, mostly to Eastern Health, between 2016 and 2018. DHHS has advised that services can submit a business case to DHHS requesting additional resources, but this process is not documented anywhere and AWH was not aware of this process.
Figure 2G
Number of mental health inpatient admissions at AWH for 0–25 year-olds, 2016–18, by age at admission
Source: VAGO analysis of DHHS information, February 2019.
Youth Prevention and Recovery Centres
In addition to the inpatient beds located in hospitals, Y-PARCs offer short-term, subacute, intervention and recovery-focused clinical treatment services in residential settings. They are a voluntary program sometimes described as a 'step up, step down' service for young people aged 16–25 years who are unwell, but not so unwell that they need to be in hospital, or who have been released from hospital, but would benefit from further recovery before going home.
There are currently three Y-PARCs—in Bendigo, Frankston and Dandenong—with 10 beds in each. Each received $2.19 million funding from DHHS in 2018‑19. In 2018–19, DHHS allocated $11.9 million over three years to Melbourne Health to establish a fourth Y-PARC in Parkville. DHHS cannot demonstrate how it determined where the Y‑PARCs should be located.
The University of Melbourne evaluated the Frankston Y-PARC and found that it had positive impacts on reducing client crisis episodes and reducing emergency department presentations.
In addition to Y-PARCs, young people use adult Prevention and Recovery Centres (PARC) of which there are 23 in Victoria. All the audited health services except RCH manage at least one PARC. Our data analysis found that for the audited agencies, 212 young people up to 25 years had spent time in an adult PARC in the past three years, of which five were aged 16–18 years.
Community programs
The majority of CYMHS services are delivered to people living in the community through outpatient clinics at hospitals, or outreach programs at other community locations (community programs). These programs represent 74.4 per cent of CYMHS annual funding—$95 million in 2018–19.
DHHS does not advise health services on the intent or deliverables for eight of the 14 CYMHS community programs it funds—totalling over $19 million.
DHHS's lack of guidance on what community programs health services should deliver makes it impossible to understand funding distribution across programs and to monitor performance of health services against program objectives, where they exist. We discuss this further in Section 3.2.
DHHS asserts that health services are best placed to determine local need; however, it should still articulate what it expects health services to deliver based on statewide analysis of need and demographics. Without such guidance, DHHS cannot hold health services to account for the funding they receive and assure itself that the right services are provided in the right places.
Under the current devolved system, children and young people receive different services and care based on the catchment they live in, which leads to inequity across the system and can also mean that clients who move between catchments may lose services that were previously available to them.
With a lack of any other guidance on what they are expected to deliver with their community funding, some health services have developed their own internal systems based on how DHHS provides their CYMHS funding through up to 14 'funding lines' in their financial system. Figure 2H shows how DHHS's financial system identifies 14 'funding lines' and the availability of guidance for each.
Figure 2H
DHHS funding in 2018–19 and guidance to health services for clinical mental health services for children and young people, by funding line
|
Program |
Total program funding 2018–19 ($) |
Number of health services receiving this program funding |
Guidelines available |
Program description in policy and funding guidelines |
|---|---|---|---|---|
|
Child and adolescent treatment services |
56 042 170 |
13 |
No |
Yes |
|
Early psychosis |
11 425 522 |
15 |
No |
Yes |
|
CAMHS and Schools Early Action (CASEA) |
6 440 097 |
13 |
Yes |
No |
|
Youth integrated community service |
5 650 860 |
7 |
No |
No |
|
Intensive youth support |
4 807 444 |
9 |
No |
Yes |
|
Child clinical specialist initiatives |
2 115 152 |
13 |
Yes |
No |
|
Gender dysphoria |
2 047 896 |
1 |
No |
No |
|
Mental health output eating disorders funding |
1 432 591 |
1 |
No |
Yes(a) |
|
Mental health and intellectual disability initiative (MHIDI) |
1 321 000 |
1 |
No |
No |
|
Autism coordinator |
1 071 258 |
14 |
No |
No |
|
Homeless youth dual diagnosis initiative (one-off funding) |
1 004 272 |
8 |
No |
No |
|
Community forensic youth mental health |
752 019 |
2 |
No |
No |
|
Youth justice mental health |
724 711 |
5 |
No |
No |
|
Refugee |
200 000 |
1 |
No |
No |
(a) There is a program description for 'Community Specialist Statewide Services – Eating Disorders', which we have assumed to be the same program as 'Mental health output eating disorders' funding.
Source: VAGO analysis of DHHS information, February 2019.
Lack of program guidelines or expectations
|
DHHS commissioned the Reform of Victoria's specialist clinical mental health services: Advice to the Secretary, DHHS in 2017. It provided advice on future directions for Victoria's specialist clinical mental health services. The report has not been released to health services or the public. |
The 2017 Reform of Victoria's specialist clinical mental health services review recommended that DHHS 'develop clinical guidelines that specify expectations of the level and mix of services', but DHHS disputes that it should develop program guidelines for mental health programs, and does not plan to develop guidelines for the remaining programs.
The DHHS Policy and Funding Guidelines 2018–19 provides a one or two-sentence 'program description' for six mental health community programs that mention children and young people, but only four align with the CYMHS funded programs. The brief program descriptions, where they exist, do not provide sufficient guidance to health services about the intent or expected deliverables for their funded programs.
Some funding lines are historical and reflect programs that have ceased while the funding has continued. For example, the youth integrated community service funding line provides $5.7 million per year to seven CYMHS. DHHS advises that this was originally funding to trial new Youth Early Intervention Teams in 2010 and that DHHS did not continue that program after a change in policy directions in 2013. DHHS does not know why it has continued to provide CYMHS with this funding given the program does not exist, nor could it provide guidance on how health services should use this funding.
2.5 Inconsistency in treatment age
When requiring inpatient care, all 18–25 year-olds must use the adult mental health system with the exception of the 16 beds at Orygen Youth Health in the Western region and the youth inpatient service at Monash Health. Only four of 13 CYMHS provide youth-targeted community programs for young Victorians aged 18–25 years, as shown in Figure 2I.
Historically, all health services treated children only to age 18 years. However, it is now commonly understood that it is not in the best interests of young people to transfer to the adult system at 18 years, as this is a vulnerable time in their life. This is especially true for adolescents in out-of-home care, who must manage the significant transition to independent living at this age.
Figure 2I
Age eligibility for programs, by CYMHS
|
Health service |
Child inpatient |
Adolescent inpatient |
Youth inpatient/ residential |
Community programs |
|---|---|---|---|---|
|
AWH |
No |
No—refers to Eastern Health |
No |
0–18 |
|
Alfred Health |
No |
No—refers to Monash health |
No |
0–18 for residents of Bayside and Kingston 0–25 for residents of Port Phillip, Stonnington and Glen Eira |
|
Austin Health |
Yes— up to age 13 |
Yes—ages 13–18 |
No |
5–18 for community teams Three specialist/outreach teams extend to 24 or 25 years |
|
Ballarat Health |
No |
Two local beds and also refers to RCH |
No |
0–14 Child and infant 15–25 Youth |
|
Barwon Health |
No |
No—refers to RCH |
No |
0–15 |
|
Bendigo Health |
No |
No—refers to Austin Health |
Y-PARC—ages |
0–18 |
|
Eastern Health |
No |
Yes—ages 13–18 |
No |
0–25 |
|
Goulburn Valley Health |
No |
No—refers to Eastern Health |
No |
0–18 |
|
Latrobe Regional Hospital |
No |
Two local beds and also refers to Monash Health |
No |
0–18 |
|
Melbourne Health (Orygen) |
No |
Yes—ages 15–24 |
Yes—ages 15–24 |
15–24 |
|
Monash Health |
Yes—ages 0–12 |
Yes—ages 12–18 |
Yes—Youth mental health service for 19–25 years Y‑PARC—ages |
0–18 Early in Life Mental Health Service 19–25 Youth mental health service |
|
Ramsay Healthcare (Mildura) |
No |
Two local beds and also refers to Austin Health |
No |
0–18 |
|
RCH |
No |
Yes—ages 13–18 |
No |
0–14 (15+ referred to Melbourne Health) 0–18 (some statewide services) |
|
Southwest Healthcare |
No |
No—refers to RCH |
No |
0–18 |
Source: VAGO interviews and document review with audited health services; public websites service descriptions for other services.
The inconsistencies exist because DHHS introduced, then ceased midway, a suite of pilot projects to increase the age eligibility to 25 at some health services. DHHS has taken no action to address the subsequent differences in age eligibility across the system.
The Victorian Government introduced a reform strategy for mental health services in 2009, Because Mental Health Matters, which included a specific commitment to 'redeveloping services within a 0–25 years framework'. The government provided $34 million for the following projects to progress this commitment:
- child and youth mental health service redesign—two demonstration projects
- youth early intervention teams—six sites
- youth justice mental health initiative—six sites
- youth crisis response team—two sites
- Y-PARCs—two sites.
This reform strategy ceased in 2013, during its fourth year of implementation, following the change of government. No alternative strategic direction or policy replaced it. Despite this, DHHS continues to provide funding for defunct programs, but does not tell health services what to do with it.
The reform strategy introduced fundamental changes to the whole service system; however, DHHS did not advise health services whether they should continue with the changes or revert to the previous system. This has resulted in inconsistency as some CYMHS chose to continue with the reforms independently while others did not.
DHHS commissioned external consultants to undertake two formal evaluations of the reform projects in 2012 and 2013. These reports contain valuable lessons about effective strategies for undertaking the reforms and delivering services to 0–25 year-olds. The reports would be particularly beneficial for the CYMHS that were part of the projects, as well as those that have chosen to, or are considering, reforming their services to a 0–25 year-old framework. DHHS has not shared this information with those CYMHS and has no plans to do so.
2.6 Geographic distribution of services
Our analysis of CYMHS funding by geographic area compared to the population of 0–24 year-olds shows substantial variation in funding distribution per head, with the South Western area of the state receiving $57.94 per child and young person compared to the North Eastern's $79.87. This analysis does not include forecasts of population growth and includes several statewide services that should not be directly mapped to regions. DHHS should investigate these funding discrepancies.
Figure 2J
Geographic distribution of 2018–19 CYMHS funding compared to population of 0–24 year-olds
Note: Funding was assigned to a geographic area based on the CYMHS referring relationships as shown in Figure 2A. The three health services delivering a limited program were assigned to an area based on which CYMHS catchment they are located in. Our analysis does not account for exact residence of clients receiving services in each region, such as where one CYMHS delivers a specialised, statewide program and the clients receiving that service may reside in other regions—we have assumed in this analysis that the funding provided into each region is serving that same region's population.
Source: VAGO analysis of Australian Bureau of Statistics (ABS) 2016 Census data, DHHS 2018–19 funding to health services information and DHHS catchment areas.
DHHS has advised that it carries out demand forecasting and considers population size and socio-economic issues when distributing new funding. However, it could provide only one example—the $4.1 million ongoing funding to expand clinical services to children under 12 in 2016–17.
Our examination of DHHS's analysis shows that it distributed most of that funding according to a model that considered the number of children living in each CYMHS catchment, the current funding, and the catchment's socio-economic disadvantage. DHHS applied this model to $3.7 million of the funding and then made some adjustments to the model, which are only partly explained in their working papers.
Monash Health received $100 000 more than the modelling allocated it, which appears to be related to its new inpatient service for children. DHHS allocated the remaining $232 410 to RCH because its funding (per head of catchment population) was significantly lower than all other CYMHS.
DHHS's modelling in 2016 showed that RCH received $38.28 community funding per head of population in its catchment, compared to an average across all CYMHS of $72.42. The second-lowest funded CYMHS was significantly higher than RCH, at $58.88 per head of population. RCH confirmed that it had been operating for many years under very challenging resource constraints and while DHHS had never explained to them the rationale for the substantial increase in funding for 2016–17, it did relieve some of its resource pressures in meeting its population's demand.
Despite carrying out modelling in 2016, DHHS still does not monitor geographical equity of CYMHS funding and has not acted to address the ongoing inequities in geographic distribution that our analysis indicates.
2.7 Workforce development
DHHS's Mental Health Workforce Strategy (the workforce strategy), which it published in 2016, notes age-appropriate and developmentally focused care as a principle, but does not address how the CYMHS workforce's needs might be met.
Although the workforce strategy provides a clear future direction around general mental health workforce issues, it lacks timelines, milestones and mechanisms to keep DHHS accountable for its implementation—such as targets and performance measures. The Workforce Strategy was informed through consultations with members of the workforce, service providers, education and training providers, professional bodies, unions, and peak bodies including consumers and carers. However, DHHS did not specifically consult with CYMHS on the strategy. It advised that this was not possible in its available budget.
The 2018–19 Victorian Budget invested $32.5 million towards implementing the workforce strategy, with a focus on reducing occupational violence against the mental health workforce in inpatient units. This investment included the six Clinical Nurse Consultants appointed to implement quality improvement initiatives in CYMHS inpatient wards—these are described further in Section 3.2. However, it did not include other initiatives to consider or address the specific workforce challenges that CYMHS experiences.
A major workforce challenge for CYMHS is filling clinical positions that require specialised skill sets such as working with children and young people who have a disability and mental health problems. After advertising repeatedly, the MHIDI pilot project at Alfred Health changed its recruitment approach. Alfred Health advertised for mental health clinicians, and committed to train them in working with disability on commencement. The process took two years, which naturally created a delay in initiating the project and the service it created. As DHHS never circulated lessons from the MHIDI project, other CYMHS have not had the opportunity to replicate Alfred Health's solution, risking repetition of the challenges and delays they experienced, as discussed further in Section 4.5.
In 2017, DHHS commissioned RANZCP to conduct a review of workforce issues for psychiatrists in Victoria, which included child and adolescent psychiatry. DHHS has not responded to the review's findings that relate to child and adolescent psychiatry or CYMHS, which included:
- a shortage of child and adolescent psychiatrists in Victoria
- a shortage of training positions for child and adolescent psychiatrists in Victoria, especially in regional areas
- workload issues for child and adolescent psychiatrists in regional areas.
The number and location of psychiatry training positions is determined by federal funding to RANZCP to provide the training, and health services' local decisions to create the training positions within their medical workforce. DHHS has taken no action to encourage health services that it funds to increase their child and adolescent psychiatry training places.
3 Monitoring performance, quality and outcomes
Government departments have a core responsibility to monitor the performance of their funded agencies and to understand what services or other public value is being delivered with the funding that it provides, and ideally to also understand what outcomes are achieved.
The processes and information that departments use to make decisions about funding and the performance of funded agencies—often described as performance and accountability frameworks—should be clear and transparent to all relevant stakeholders. In most cases they should also be transparent to the public and the recipients of services.
3.1 Conclusion
DHHS does not have a clear method for monitoring the performance of the CYMHS system within broader health service and mental health system performance monitoring and oversight. Without this, DHHS cannot fulfil its role to advise government on the system's performance, its resourcing needs, or the challenges patients and health services face in engaging other necessary social services. An example of this is that the current performance monitoring system has not highlighted the significant number of young people regularly 'stuck' in inpatient mental health services. Legislated mechanisms to protect the most vulnerable Victorians are also impeded by bureaucratic hierarchies and silos within DHHS.
3.2 Monitoring performance
DHHS has no effective governance arrangements to provide oversight of CYMHS, as CYMHS monitoring is embedded within broader performance monitoring and system oversight, as seen in Figure 3A. Legislation mandates some of the Chief Psychiatrist's and Secretary's monitoring but other components of the monitoring would benefit from a more systemic approach.
Figure 3A
DHHS performance monitoring agreements for CYMHS, their oversight bodies and mechanisms, the KPIs and other items
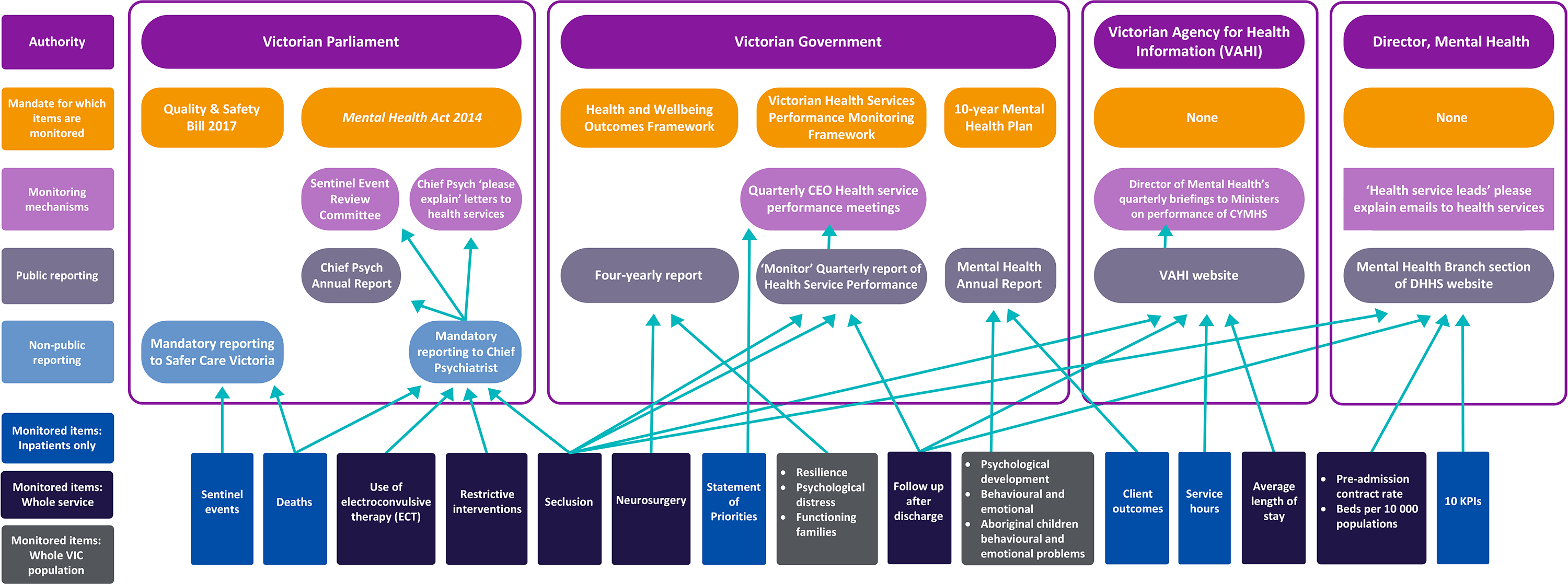
Key to ‘Monitored items’ section: Dark grey = population-level health outcomes. Blue = consider only inpatient services. Dark purple = monitor either community programs or CYMHS as a whole.
Note: Regarding reporting of deaths, Safer Care Victoria and the Chief Psychiatrist each require reporting of certain types of deaths only. Different criteria are legislated/mandated for each reporting requirement.
Source: VAGO, with information provided by DHHS.
DHHS does not have mechanisms to identify and address consistent issues in CYMHS in order to proactively prevent safety breaches or improve the quality of CYMHS.
When the performance monitoring that occurs around CYMHS is presented together, as in Figure 3A, it is evident that a lack of overarching governance and coordinated monitoring of CYMHS creates an unnecessary reporting burden on health services.
There are 29 components of CYMHS service delivery or outcomes that are monitored, by mandate or request, through seven different systems that are managed by DHHS and overseen by four different authorities with different roles and responsibilities in monitoring the performance of CYMHS. There are also six public reports produced by six different agencies or groups about different aspects of CYMHS performance.
This section examines the effectiveness and appropriateness of each of the seven different systems for performance monitoring of CYMHS, which are:
- the Victorian Health Services Performance Monitoring Framework, published by DHHS's Health Services Performance and Regulation Branch, which also convenes the primary performance monitoring discussions between DHHS and health service CEOs each quarter
- 15 KPIs on CYMHS service delivery and outcomes, collected and publicly reported by the Mental Health Branch
- legislated responsibilities of the Chief Psychiatrist to monitor five components of service delivery and the quality of services more broadly
- the Quality and Safety Bill 2017 by which Safer Care Victoria (SCV) was established as an administrative office of DHHS with a range of functions, including monitoring sentinel events
- public reporting on five components of CYMHS service delivery by the Victorian Agency for Health Information (VAHI), another administrative office of DHHS
- the Mental Health Services Annual Report, which the Secretary of DHHS has a legislated responsibility to produce
- the Victorian Government's Health and Wellbeing Outcomes Framework, which monitors three components of Victorian children and young people's mental health.
|
Sentinel events are defined by SCV as 'unexpected events that result in death or serious harm to a patient while in the care of a health service'. |
Three items are reported and monitored by multiple mechanisms and agencies, as follows:
- Some deaths must be reported as a sentinel event to SCV and the Chief Psychiatrist also requires notification of 'reportable deaths'. The two mechanisms use different definitions of what needs to be reported and have different processes for how they are reported and analysed.
- The rate of seclusion events is monitored by the Chief Psychiatrist;the Monitor report, which makes it a topic of the quarterly CEO health service performance meetings;and public reporting on both the VAHI website and the Mental Health Branch's section of the DHHS website.
- The rate of follow-up after discharge is similarly reported in Monitor and therefore CEO health service performance meetings as well as public reporting on VAHI and DHHS websites.
The latter two items relate only to inpatients and DHHS could not provide any rationale for why the most actively monitored items neglect the largest component of CYMHS clients, those receiving community programs.
In addition to the performance monitoring arrangements described above, both the Public Advocate and the Mental Health Complaints Commissioner, which was established under the new Act in 2014 as an independent authority, undertake investigations around mental health services. These entities require health services to provide information about incidents, which can duplicate what they provide to DHHS.
DHHS could not provide evidence that it had taken any action to understand the complexity and duplication that exists within the performance monitoring arrangements. It has taken no action to streamline or resolve conflicts and confusion caused by the overlapping reporting requirements for health services or its own duplicated monitoring arrangements, except for discussions around sentinel event reporting, which resulted in a joint OCP and SCV sentinel event review process.
During the audit, DHHS commenced a project to develop a new performance and accountability framework for mental health, with an initial focus on adult services. DHHS should ensure the inclusion of CYMHS in this work and also consider health services' reporting burden under current and future accountability arrangements.
DHHS has advised that 'quality and safety reporting and monitoring requirements will continue to be managed by the Office of the Chief Psychiatrist'. DHHS needs to ensure that there is clarity and transparency about the role of the Chief Psychiatrist in performance monitoring, and the accountability framework should articulate the Chief Psychiatrist's role.
There is no single source of information for CYMHS about either reporting requirements or DHHS's performance monitoring activities. The DHHS Policy and Funding Guidelines 2018–19 contain only an incomplete description of reporting and monitoring for CYMHS.
During the audit, the Director of Mental Health proposed some additions to the 2019–20 version of the DHHS Policy and Funding Guidelines to detail all of health services' mandatory reporting requirements to the Chief Psychiatrist.
Even if the proposed changes to the DHHS Policy and Funding Guidelines 2019–20 proceed, there remains no single source of information on the reporting requirements and performance monitoring arrangements for CYMHS. This reflects a siloed approach within DHHS and within the Mental Health Branch itself (between its performance monitoring area and the OCP), which inhibits DHHS from effective and efficient performance monitoring. It also inhibits DHHS's capability to provide accurate advice to government on CYMHS and the needs of Victorian children and young people with serious mental health problems. Although during the audit, DHHS finalised an Operational Model, which outlines a more integrated approach to performance monitoring that details the roles of the performance monitoring area and the OCP.
The Victorian Health Services Performance Monitoring Framework
The Victorian Health Services Performance Monitoring Framework describes DHHS's roles, responsibilities and processes for monitoring the performance of health services across all areas of quality of care, governance, access to care, and financial management. It specifies two KPIs for CYMHS that health services' CEOs are held accountable for by DHHS, through its quarterly performance meetings.
Figure 3B
Victorian Health Services Performance Monitoring Framework KPIs for child and youth mental health
|
KPI |
Target |
|---|---|
|
Rate of seclusion events relating to a child and adolescent acute mental health admission |
15 seclusions per 1 000 bed days |
|
Percentage of child and adolescent mental health inpatients with post-discharge follow-up within seven days |
80 per cent 75 per cent prior to 1 July 2018 |
Source: VAGO, from the Victorian Health Services Performance Monitoring Framework 2018–19.
DHHS could not provide a rationale for why it chose these two KPIs as the measures of CYMHS performance at a high level. Each KPI addresses areas that are important to monitor, but we found critical weaknesses in how the follow-up rate is calculated and how the seclusion rate is reported. It is a significant concern that these KPIs apply to inpatients only. The Victorian Health Services Performance Monitoring Framework therefore does not monitor the largest cohort of CYMHS clients, those in community or outpatient programs, which represent 74.4 per cent of CYMHS funding and a greater, though undetermined, proportion of people receiving CYMHS services.
Monitoring seclusion
If a health service exceeds DHHS's target for seclusions in CYMHS, DHHS brings this to the attention of the health service CEO and Board through the Monitor report and the quarterly health service performance meetings. CYMHS leaders are subsequently asked to explain the breach of the target to their hospital executive and Board. The explanation requires significant time and resources because of the required detail, which includes the background of the young people involved, and the complex and rapid clinical decisions that led to seclusions.
Quality improvement activities must accompany monitoring activities, otherwise a punitive culture can develop, which can worsen the practice the KPI is seeking to improve.
International literature shows that effectively reducing seclusion requires a comprehensive set of actions including training, debriefing and leadership on organisational change, alongside monitoring data. DHHS should consider reporting a health service's engagement in evidence-based activities to improve seclusion practices alongside the KPI in the Monitor report.
Figure 3C
Definition of seclusion in mental health care
|
Seclusion is the confinement of a patient at any time of the day or night alone in a room or area from which free exit is prevented. The purpose, duration, structure of the area and awareness of the patient are not relevant in determining what constitutes seclusion. Seclusion also applies if the patient agrees to or requests confinement and cannot leave of their own accord. While seclusion can be used to provide safety and containment at times when this is considered necessary to protect patients, staff and others, it can also be a source of distress; not only for the patient but also for support persons, representatives, other patients, staff and visitors. Wherever possible, alternative, less-restrictive ways of managing a patient's behaviour should be used, and hence the use of seclusion minimised. |
Source: Australian Institute of Health and Welfare, Mental Health Services in Australia, 2019.
Since 2013, the Office of the Chief Mental Health Nurse within DHHS has led important work to introduce systems-oriented quality-improvement practices focused on seclusion and other restrictive practices across Victorian mental health services, including CYMHS.
Safewards is a UK-developed model with a set of 10 interventions designed to reduce conflict and containment in inpatient services. The trial of Safewards in Victoria in 2013 included two youth and one adolescent ward, as well as an adult ward that receives funding for two adolescent beds. A comprehensive evaluation by The University of Melbourne, published in 2015, showed that the rate of seclusion in the three adolescent/youth wards reduced significantly from 19 seclusions per 1 000 occupied bed days before the 12-week trial to 9.5 seclusions at the 12-month follow-up. The trial also showed promising, though less significant, improvements in adult services.
A 2016 expansion of Safewards engaged all but one of the adolescent and youth CYMHS wards. One of the child wards did not yet exist and the other was deemed out of scope for the project.
In 2018–19, another initiative to expand the Safewards program saw eight of the 11 CYMHS inpatient wards funded to employ a Clinical Nurse Consultant whose responsibilities include implementing Safewards and other activities to reduce restrictive interventions. A ninth CYMHS, Orygen Youth Health, had recently established a similar position at the time that the Victorian Budget provided this new funding, so it did not receive the funding but is doing the same work. Figure 3D shows the CYMHS wards that have been engaged in each of these three components of the Safewards program. DHHS needs to ensure that all CYMHS inpatient wards are engaged with Safewards.
Figure 3D
Participation in the three components of the Safewards program, by CYMHS wards
|
Ward |
Trial, 2013 |
Expansion, 2016 |
Clinical Nurse Consultant funded, 2018–19 |
Any of the three components |
|---|---|---|---|---|
|
Metropolitan services |
||||
|
Austin—adolescent |
✘ |
✔ |
✔ |
✔ |
|
Austin—child |
✘ |
✘ |
✔ |
✔ |
|
Eastern—adolescent |
✘ |
✔ |
✔ |
✔ |
|
Monash—youth |
✔ |
✔ |
✔ |
✔ |
|
Monash—adolescent |
✔ |
✔ |
✔ |
✔ |
|
Monash—child |
n/a |
n/a |
✔ |
✔ |
|
Orygen Youth Health |
✔ |
✔ |
self-funded |
✔ |
|
RCH |
✘ |
✔ |
✔ |
✔ |
|
Regional services |
||||
|
Ballarat Health |
✘ |
✔ |
✔ |
✔ |
|
Latrobe Regional Hospital |
✔ |
✔ |
✘ |
✔ |
|
Mildura Base Hospital |
✘ |
✘ |
✘ |
✘ |
|
Total |
4 |
8 |
8–9 |
10 |
Note: Monash Child ward opened in 2018.
Note: The sites in Figure 3D were nominated for the expansion of the project but their actual participation varied due to staged implementation based on service capability.
Note: Monash Health and Austin Health both have one Clinical Nurse Consultant position split across their child and adolescent wards, making the total number of Clinical Nurse Consultants across CYMHS six.
Source: VAGO, based on information from DHHS.
Despite the significant work with Safewards, the rates of seclusion in CYMHS continue to exceed DHHS's target of 15 seclusions per 1 000 bed days and the national rate in 2017–18 of 8.1 seclusions per 1 000 bed days. DHHS advises that the national rate is lower than the Victorian rate due to a stricter definition of seclusion in Victoria, and therefore higher rates of reporting in Victoria. However, DHHS has not conducted an audit or review to confirm this theory.
DHHS's rationale for setting the target at 15 seclusions per 1 000 bed days includes data from a report it published in 2018 that shows trends in seclusion rates in adult mental health services only. DHHS advises that its Restrictive Interventions Governance Group has considered the target on several occasions. This group decided against reducing the target, but DHHS could not provide evidence of these deliberations.
DHHS monitors and publicly reports the seclusion rate at individual health services and calculates the total rate for all metropolitan CYMHS, which has only exceeded the target in one quarter since 2015–16, as shown in Figure 3E.
Figure 3E
Seclusion rate for audited CYMHS per 1 000 bed days, 2015–16 to 2017–18
Note: In the graph Q refers to 'Quarter'.
Note: The target in the Victorian Health Performance Framework is 15 seclusions per 1 000 bed days.
Source: VAGO analysis of information available on DHHS website. National rate 2017–2018 as reported by Australian Institute of Health and Welfare in Mental Health Services in Australia, published 22 March 2019.
|
The Act defines seclusion as 'the sole confinement of a person to a room or any other enclosed space, from which it is not within the control of the person confined to leave'. |
A variety of scenarios can occur when a young person in a mental health facility becomes agitated or aggressive. These can include a clinician leaving the room so that the young person is left alone. The door to the room where the young person is can be left open, closed or locked. There are different understandings among CYMHS clinicians about whether an open door, or a closed but unlocked door, must be reported and recorded as a seclusion.
In 2018, the Chief Psychiatrist wrote to authorised psychiatrists about a concern that seclusion was under-reported. There was debate about reporting practices at a forum of mental health nurses in November 2018, which was chaired by DHHS's Chief Mental Health Nurse, that included different interpretations of the 2018 correspondence from the Chief Psychiatrist.
|
An authorised psychiatrist is appointed by the board of a health service and has specific legislated responsibilities under the Act around compulsory assessment and treatment and other situations where a consumer's rights may be at risk. |
Inconsistent reporting of seclusion reduces the validity of the KPI. DHHS needs to better understand whether there are variable reporting practices around seclusion in CYMHS and take strategic action to improve them.
Chief Psychiatrist monitoring of individual seclusions
Health services must report every case of seclusion to the Chief Psychiatrist through monthly reporting processes. Reports include the patient's date of birth, which allows the Chief Psychiatrist to identify seclusions of children and young people. Reports include the duration of seclusion, the reason for it, who secluded the patient, and who approved and authorised the seclusion. The Chief Psychiatrist's Data Review Working Group reviews all reports of seclusion monthly. Services are required to clarify the circumstances of episodes of seclusion and restraints that exceed thresholds. In circumstances where the clarification raises concerns regarding quality and safety, the matter is brought to the Chief Psychiatrist's Portfolio Governance meeting for assessment and review. This process is highly resource-intensive, with approximately 10 senior staff involved at least half a day every month.
DHHS could not provide evidence of how it decides that there is a 'concern' that requires action or analysis to identify trends or persistent issues to inform strategic action.
The current process is reactive and focuses on singular cases. DHHS advises that actions arising from the meetings include phone calls made by senior staff to the authorised psychiatrists in the health services concerned. They may also instigate visits to health services by the Chief Psychiatrist and/or the Chief Mental Health Nurse. DHHS should develop a more transparent, timely, and efficient mechanism for reviewing individual cases of seclusion.
To enable this, DHHS should consider analysis of individual seclusion reports that includes:
- identifying trends at health services over time
- identifying trends or clusters within vulnerable population groups
- collecting and analysing additional information about the secluded client such as indicators of vulnerability, which for children and young people would include legal status with regards to child protection, disability diagnoses and family and housing characteristics.
This form of analysis would be consistent with the 2016 external review of the OCP, to be discussed in Section 3.7, which recommended increasing data analysis capacity.
There is no evidence that this monitoring of individual seclusion cases by the OCP is coordinated with the monitoring of the seclusion rate by the performance monitoring areas of DHHS. When DHHS communicates a breach of the seclusion rate target to hospital CEOs through its performance monitoring, it should draw on the information it holds through the OCP's extensive monitoring processes to form consolidated and consistent advice to health services.
Monitoring seclusion in regional health services
DHHS does not report the seclusion rate—or any other KPI—for the six CYMHS inpatient beds it funds for regional health services in Ballarat, Mildura, and Gippsland as it does for metropolitan services. DHHS advises that it 'monitors all seclusions for all health services Ö against age-determined benchmarks', but it could not provide evidence of seclusion rates for these regional CYMHS beds nor for children and adolescents in these regional services. One example of a seclusion report received by the OCP for a young person in a regional service was provided, but there is no evidence that seclusion of children and young people in regional health services is monitored strategically.
DHHS has not taken action to investigate the rate of seclusion for children and adolescents in these or any other regional mental health services. In Section 2.4, we detailed the significant problems with the system design around these beds and the risk that health services are not able to use them as a child and adolescent inpatient service.
In Section 2.4, we also showed how there are significant numbers of both adolescents and young adults using adult inpatient services in the regional health service that we audited. DHHS has taken no action to monitor the seclusion rate for children and young people who are being admitted as inpatients to adult services.
Post-discharge follow-up
Continuity of care, especially after an inpatient admission, is a critical component of good-quality mental health care. It requires the discharging inpatient service to make appropriate referrals, and communicate with the 'receiving' community program as well as the client and family. It also requires the 'receiving' community program to participate in the discharge process and communicate effectively with the inpatient service, client and family.
The post-discharge follow-up KPI holds only the 'receiving' CYMHS accountable for follow-up, when the process is also highly dependent on the inpatient service communicating well during the discharge process.
This issue is significantly exacerbated in the Western metropolitan region, where CYMHS funding and service delivery is shared between two organisations. RCH provides an inpatient service for adolescents aged 13–18 years, but their community programs that offer follow-up care for younger clients cease at 15 years. For RCH inpatients aged 15 years or over who live in the Western metropolitan catchment—approximately 300 young people each year—follow-up care is provided by Orygen Youth Health.
DHHS's performance monitoring system does not account for this complexity through its KPI reporting. RCH is reporting against post-discharge follow-up within seven days for inpatients over 15 years, although this service is provided by Orygen Youth Health. Orygen Youth Health, which is funded to provide the follow up care, is only held accountable for following up its own inpatients, excluding those transferred from RCH. During the audit, DHHS committed to 'improve the transparency' around this matter, but did not advise how they plan to do this and whether it will rectify this error in its performance monitoring system.
DHHS advises that the follow-up target is set at only 80 per cent to allow for clients who may use services outside of the Victorian public mental health system for their follow-up care. It had not done any research or analysis to confirm what proportion of CYMHS clients receive their follow-up care in the private or other parts of the health system. The target is also consistently lower than the current data on follow-up, which shows an average of 90 per cent for metropolitan services and 87 per cent for rural services. DHHS increased the target from 75 per cent to the current 80 per cent on 1 July 2018, but could not provide a rationale for why the target was increased or why 80 per cent was chosen.
3.3 Mandatory reporting to the Chief Psychiatrist
The Act stipulates that health services must report to the Chief Psychiatrist on:
- use of ECT
- results of neurosurgery performed
- use of restrictive interventions
- reportable deaths under the Coroners Act 2008.
The Chief Psychiatrist has powers under the Act to request additional reporting to what is legislated. This is communicated to health services as a part of guidelines that address individual topics, such as the guideline on ECT, for which the Chief Psychiatrist requires reporting 'in advance' for children and adolescents. As another example, in 2018, the Chief Psychiatrist issued a new reporting instruction to health services to mandate reporting of sexual safety violations.
During the audit, the OCP provided us with some proposed changes to the DHHS Policy and Funding Guidelines 2017–18 to include all mandatory reporting requirements to the Chief Psychiatrist. This is an important development if it proceeds, because while some of the mandatory reporting to the Chief Psychiatrist is contained in legislation, other requirements are issued through topic-specific guidelines or directives. There are currently 32 documents on the Chief Psychiatrist's website that health services need to review to identify whether they contain a reporting mandate.
|
A person with dual disability has a developmental disability, such as intellectual disability or autism spectrum disorders and also severe mental health problems. |
During the audit, the OCP proposed a new requirement for health services to report long periods of seclusion and long stays in high-dependency units, which our audit has shown are important matters to monitor in CYMHS given the challenges with complex clients with dual disability. However, this is only proposed as a revision to the DHHS Policy and Funding Guidelines 2019–20. The OCP advises that they will consider whether a guideline or reporting directive is required after reporting has commenced. This creates another level of inconsistency in reporting guidance for health services where some reporting requirements have directives or guidelines from the Chief Psychiatrist to explain the context, rationale and reporting processes, but others do not.
Health services are confused about their reporting obligations and associated actions with regards to SCV and the Chief Psychiatrist having some overlapping responsibilities. DHHS has not taken any action to clarify or explain this.
Some of the information health services report to the Chief Psychiatrist is made public through their annual reports. The reports use age groupings or service type of child and youth, adult or aged which allows monitoring of these measures for CYMHS, but only at a statewide level. There are privacy issues that reasonably explain why the data should not be publicly reported at a health service level.
The last published annual report for 2016–17 reported:
- seclusion episodes per 1 000 occupied bed days, by clinical program
- bodily restraint episodes per 1 000 occupied bed days
- number of ECTs for people under 18 years, and for 18–29 year-olds, by gender.
Deaths reported to the Chief Psychiatrist are not stated in the annual report by age for privacy reasons, although they are carefully monitored by the OCP.
The Chief Psychiatrist annual report for the period ending June 2018 was not published until March 2019, nine months after the end of the reporting period. This data is less useful when it is reported with extensive delays.
The OCP analyses the data it receives and identifies trends that it acts on either by issuing statewide guidance or instigating investigations of specific services. However, we found that this guidance is not communicated to CYMHS leaders nor is it understood consistently by senior staff in CYMHS responsible for implementing it.
The Chief Psychiatrist also chairs a Sentinel Event Review Committee, which makes recommendations about themes and system issues.
3.4 Mental Health Branch's monitoring activities
DHHS's Mental Health Branch monitors the performance of CYMHS through a suite of 15 KPIs, allocation of 'health service leads' and convening program meetings with each health service.
Key performance indicators
DHHS has a broader suite of 15 KPIs for CYMHS, shown below in Figure 3F, which it publicly reports on four times per year on its website. These KPIs have significant problems with their appropriateness as a representation of performance.
There is no governance structure or performance monitoring framework that oversees the development or use of these KPIs. DHHS has never evaluated, reviewed or consulted health services nor other experts on these or other KPIs' appropriateness for monitoring the performance of CYMHS. DHHS advises that its plans to develop a performance and accountability framework for mental health include reviewing its KPIs. DHHS should ensure that this review extends to the CYMHS KPIs, and addresses the problems with validity and appropriateness that are described in this report.
DHHS's rationale for the selection of these KPIs is that they are 'based on the national KPIs', but it could not explain the rationale for many of the significant differences between the national KPIs and those that it uses.
The national KPIs are formally known as the Key Performance Indicators for Australian Public Mental Health Services, Third Edition ('the national KPIs'), which are developed and overseen by a subcommittee established to advise the Australian Health Minister's Advisory Council. The national KPIs contain 15 KPIs that DHHS reports against to the Australian Government annually. DHHS could not provide any evidence of their decision-making process to develop their own suite of KPIs and the changes made from the national KPIs, which had been developed by high-level committees of experts in the field.
DHHS does not have a corresponding KPI for six of the national KPIs, which are marked as red in Figure 3F, and its rationale for excluding each is either absent or incomplete for three of these KPIs as follows:
- 'Costs of services'—data is available because it is reported to the Australian Institute of Health and Welfare, but DHHS could not provide any rationale for excluding this KPI
- 'Accessibility—New client index'—no rationale
- 'Accessibility—Proportion of population receiving care'—excluded because 'the CAMHS population is very small', without further explanation.
A further eight of the DHHS KPIs can be aligned to their counterpart in the national KPIs, but DHHS has changed them substantially, which are those marked orange in Figure 3F. For example, 'change in consumers' clinical outcomes' is measured by DHHS only for community clients, whereas the national KPI does not prescribe this limitation. 'Comparative area resources' is measured only in metropolitan areas, when geographic proximity is a known issue for regional areas and the rates of mental health problems for young people in regional areas are greater. DHHS excludes regional areas from this KPI without a rationale.
DHHS has an additional KPI outside the scope of the national KPIs, which is for monitoring services provided to children under the age of 12 years.
Figure 3F
DHHS's KPIs compared to national KPIs
|
Domain |
National KPIs |
DHHS Mental Health Branch's CAMHS KPIs |
VAHI Victorian Health Services Performance public report |
Victorian Health Services Performance Framework |
|---|---|---|---|---|
|
Effective |
Change in consumers' clinical outcomes |
Percentage of clients with significant improvement case end (community only) |
✘ |
✘ |
|
Change in mean number of clinically significant HoNOS items (community only) |
✘ |
✘ |
||
|
Mean HoNOS at episode start |
✘ |
✘ |
||
|
28-day readmission rate |
✘ |
✘ |
||
|
Appropriate |
National service standards compliance |
✘ |
✘ |
|
|
Efficient—inpatient |
Average length of acute inpatient stay |
Trimmed average length of stay, excluding same day stays and stays over 35 days |
✔ |
✘ |
|
Average cost per acute admitted patient day |
✘ |
✘ |
||
|
Efficient—community |
Average treatment days per three-month community care period |
Average treatment days |
✘ |
✘ |
|
Average cost per community treatment day |
✘ |
✘ |
||
|
Average length of case (days) |
✘ |
✘ |
||
|
Case re-referral rate |
✘ |
✘ |
||
|
Accessible |
Proportion of population receiving clinical mental health care |
✘ |
✘ |
|
|
New client index |
✘ |
✘ |
||
|
Comparative area resources |
Beds per 10 000 of population (metro only) |
✘ |
✘ |
|
|
Continuous |
Rate of preadmission community care |
Preadmission contact rate—CAMHS |
✘ |
✘ |
|
Rate of post-discharge community care |
Post-discharge contact rate—CAMHS |
✔ |
✔ |
|
|
Responsive |
Consumer outcomes participation |
Percentage self-rating measures offered |
✘ |
✘ |
|
Percentage self-rating measures completed |
✘ |
✘ |
||
|
Capable |
Outcomes readiness |
Percentage HoNOS compliant |
✘ |
✘ |
|
Safe |
Rate of seclusion |
Seclusion per 1 000 occupied bed days |
✔ |
✔ |
|
No domain in national KPIs |
n/a |
Percentage clients aged under 12 |
✘ |
✘ |
|
Service hours |
✔ |
✘ |
Key: Red = very significant variation or omission; orange = substantial variation; green = consistent.
Note: HoNOS = Health of the National Outcomes Scale.
Note: 28 day readmissions: CAMHS services advised that the 28-day readmission rate is not a reliable indicator of service as clinicians need flexibility to readmit patients if needed, without being concerned about KPIs.
Note: National service standard compliance: this KPI is measured at a health service/organisational level.
Source: VAGO analysis of Key Performance Indicators for Australian Public Mental Health Services (Third Edition), DHHS Mental Health Branch quarterly reports to Ministers and public, VAHI's Victorian Health Services Performance public report and the Victorian Health Services Performance Framework.
Health services could use these KPIs to benchmark their performance against other services, but they advise that this is rarely useful given the measures do not appropriately represent their performance. They report that the KPIs do not sufficiently monitor client outcomes and monitor seclusion in a manner that is not useful to understand the problems and respond to any performance issues at the health service level.
DHHS has not reviewed the effectiveness or appropriateness of its KPIs in monitoring CYMHS performance, nor has it strategically consulted with CYMHS or acted on their advice that the KPIs are not a useful measure of performance.
Section 4.3 of this report details how long patient bed occupancy is a significant issue in CYMHS, but DHHS could not provide any rationale or evidence to explain why it does not monitor it for CYMHS.
Six-monthly program meetings
Six-monthly program meetings are attended by senior staff from the health service (at least the Director of Mental Health, and sometimes the CEO as well) and the DHHS Mental Health Branch, often including the Chief Psychiatrist.
DHHS report that these meetings are not for performance monitoring. However, audited health services consider them to be an important forum to seek and receive guidance from DHHS and to communicate challenges and opportunities they face. Some of the audited health services noted that these meetings are their sole opportunity to formally communicate with DHHS, and in some cases their only opportunity to communicate at all, as they did not know who to contact at DHHS if they need guidance.
The meetings are held inconsistently for all but one health service, and do not regularly cover any matters related to CYMHS, focusing instead on adult mental health services. The meetings occur significantly less frequently with regional health services.
Our analysis of DHHS's minutes of these meetings over the past four years for 13 health services that have CYMHS and/or a Y-PARC found that, on average across all health services, CYMHS had only been discussed on two occasions in four years and only half of the meetings held mentioned child and youth mental health—for regional services it was less often. For four health services, only one meeting in four years had addressed child and youth matters, as seen in Figure 3G. DHHS could not provide evidence of any program meetings at AWH or Ballarat Health.
It is unclear whether agreed actions are followed through by either party, as the structure of the meetings does not frequently include reference to progress against agreed actions.
During the audit, the Mental Health Branch finalised an Operational Model, which outlines a range of processes and protocols including for:
- engaging with health services
- monitoring programs
- escalating performance issues
- working across DHHS to address systems issues
- program meetings
- ensuring the follow up of agreed actions.
Figure 3G
Six-monthly program meetings held in 2015–18
|
Meetings held |
Meetings that included matters related to children and youth |
|
|---|---|---|
|
Metropolitan services |
||
|
Alfred Health |
6 |
6 |
|
Austin Health |
8 |
7 |
|
Eastern Health |
7 |
4 |
|
Melbourne Health (auspice of Orygen Youth Health) |
5 |
1 |
|
Monash Health |
7 |
3 |
|
RCH |
5 |
5 |
|
Regional services |
||
|
AWH |
0 |
0 |
|
Ballarat Health |
0 |
0 |
|
Barwon Health |
4 |
2 |
|
Bendigo Health |
3 |
2 |
|
Goulburn Valley Health |
3 |
1 |
|
Latrobe Regional Hospital |
3 |
1 |
|
Mildura Base Hospital |
3 |
1 |
|
Peninsula Health |
7 |
2 |
|
South West Healthcare |
4 |
2 |
Source: VAGO analysis of DHHS minutes of six-monthly program meetings held between 1 January 2015 and 31 December 2018.
The role of health service leads
DHHS's Mental Health Branch allocates a health service lead to each mental health service. They are primarily responsible for liaison between DHHS and the health service around mental health matters. One staff member may be the health service lead for one or two health services.
One of the tasks of the health service lead is to ask services to explain their KPI results to DHHS when they are released quarterly. There is no protocol for what does or does not trigger the health service lead to ask for these explanations, and there is no evidence that DHHS has taken any follow-up action on the responses.
DHHS has acknowledged weaknesses in its engagement model with health services and had commenced a review at the time of the audit, but this was in a very early stage so we cannot report on its appropriateness for addressing the issues identified in this audit.
3.5 Failing to monitor accessibility
The only KPI for accessibility of services is limited to inpatient beds in metropolitan services, as shown in Figure 3F. Our March 2019 performance audit Access to Mental Health Services found that accessibility is a significant problem that DHHS needs to monitor more closely.
|
The Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA) is a clinician-rated instrument comprising 15 questions measuring behaviour, impairment, symptoms, social problems and information problems for those under 18 years. |
DHHS's KPI of a mean (average) HoNOSCA score does not allow it to monitor whether the most severe clients are accessing CYMHS. To do this, DHHS should monitor the distribution of outcome measures at admission and look at the proportion that are of a high severity. DHHS's KPI shows that CYMHS are collecting outcomes measures at a high rate, so it could commence more meaningful analysis and monitoring of accessibility immediately.
In 2012, the National Mental Health Performance Subcommittee considered adopting a new accessibility measure that would monitor whether the most seriously unwell clients were getting access to CYMHS. The measure was to look at what proportion of clients accessing CYMHS community programs had very high (95th percentile) scores on a self-rating measure that is routinely collected—the Strengths and Difficulties Questionnaire (SDQ)—Parent versions. While this measure did not become a national KPI, it is an example of a measure that DHHS could use to monitor access for CYMHS. DHHS has been collecting this data for many years, so changes over time could also be determined and monitored going forward.
|
The Strengths and Difficulties Questionnaire (SDQ) is a brief emotional and behavioural screening tool. The tool can capture the perspective of children and young people, their parents and teachers. The SDQ can be used for various purposes, including clinical assessment, evaluation of outcomes, research and screening. |
The most recent data from the Australian Mental Health Outcomes and Classification Network shown in Figure 3H demonstrates that clients admitted to CYMHS in Victoria in 2016–17 had an average SDQ impact score of between 6 and 6.1 out of 10 over the past four years. The most unwell 5 per cent of the population will have a score over 3. In 2016–17, 89 per cent of CYMHS clients in Victoria had an SDQ impact score over 3, putting them in the highest range of the most unwell 5 per cent of the population. This demonstrates that CYMHS are seeing the most unwell young people in the population.
Figure 3H shows that in 2015–16 the severity of CYMHS 'youth' clients was the highest of the four years of available data, while the severity of 'child' clients was lower than the other years. It also shows that in 2014≠–15, the minimum level for children accessing CYMHS was more severe than other years. These differences cannot be seen by the corresponding average figure, which is also shown on the chart in Figure 3H, and does not vary enough to identify changes.
Further analysis and monitoring of this data, which DHHS receives daily through its Client Management Interface (CMI) database, could show DHHS any changes over time and any variations between health services. There is no evidence that DHHS has ever reviewed the severity of clients accessing CYMHS nor taken any action where variation has occurred over time or between services.
Figure 3H
Severity of mental health problems as shown by the SDQ's impact scores for Victorian CYMHS clients at access to community programs, by year
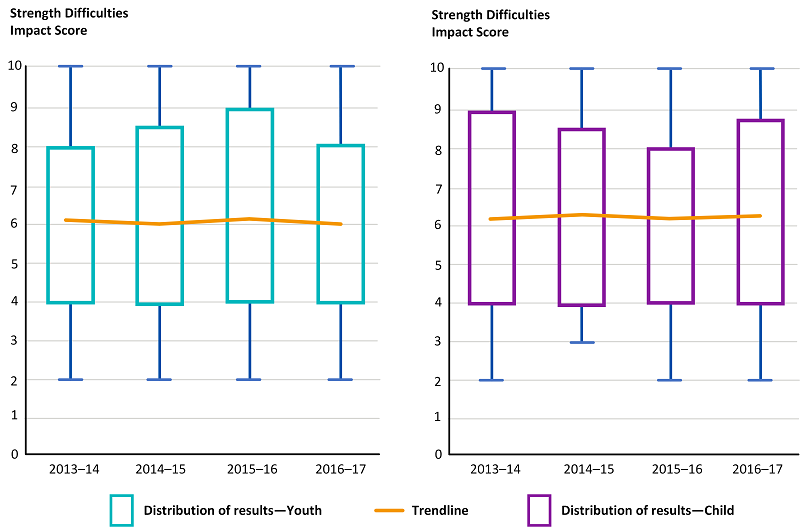
Note: The box in each chart shows the upper and lower limits of the middle 50 per cent of all scores recorded, and the lines or 'whiskers' show the upper limits, the highest and lowest scores recorded.
Source: VAGO analysis of Australian Mental Health Outcomes and Classification Network information.
The measure DHHS uses as a KPI to monitor the severity of CYMHS clients is less precise and less useful as it does not identify the wide range of levels of severity of mental health problems seen in CYMHS. It therefore does not allow any determination around whether the intended client group—those with more severe problems—are accessing CYMHS.
3.6 Other DHHS areas and agencies' performance monitoring of CYMHS
There are four performance monitoring activities for CYMHS that are managed by areas of DHHS outside of the Mental Health Branch:
- quarterly health service performance meetings
- VAHI reporting of CMI data
- sentinel event reporting to SCV
- reporting to Department of Treasury and Finance (DTF).
Quarterly health service performance meetings
The primary mechanism for managing the performance of health services is a quarterly meeting between health service CEOs and DHHS. The inputs to this meeting are the KPIs in the Victorian Health Services Performance Monitoring Framework and the agreement made through the Statement of Priorities (SoP), which are described below.
The meetings cover performance of the entire health service, and DHHS was not able to provide advice about the extent to which they address mental health performance matters. A representative of the Mental Health Branch is invited to attend if a mental health program matter is on the agenda. This can be contributed by a health service or the Mental Health Branch can recommend agenda items relating to the health service's performance against KPIs.
Statements of Priorities
Each year, a SoP is developed as an agreement between each health service and the Minister for Health on what that year's priorities will be. We analysed the SoPs for all 17 Victorian health services that receive funding directed at children and youth with mental health problems (see Appendix B for funded agencies).
No SoPs in 2018–19 mention child and youth mental health, though two did in the previous year. In 2016–17, when there was a substantial investment of new funds and new programs, only five health services mentioned child and youth mental health in their SoP.
Victorian Agency for Health Information
VAHI was established as an administrative office within DHHS in 2017 after Targeting zero: Report of the Review of Hospital Safety and Quality Assurance in Victoria made 66 recommendations about improving quality and safety in Victorian hospitals.
VAHI produces a quarterly report on the performance of Victorian health services, which includes four items that allow performance monitoring of CYMHS. All are reported at the individual health service level. These are:
- service hours provided by community mental health services
- child and adolescent mental health average length of stay
- child and adolescent mental health post discharge follow-up rate
- child and adolescent mental health seclusion events per 1 000 bed days.
DHHS advises that 27 items that VAHI reports on relate to CYMHS. However, the four above are the only items where CYMHS data is separated from other parts of the mental health system and therefore used to monitor CYMHS performance. It is not possible to monitor the performance of CYMHS using data that does not distinguish between the different sectors of the mental health system.
VAHI's quarterly report is the primary source of evidence for advising the ministers for Health, Ambulance Services and Mental Health on the performance of CYMHS.
DHHS could not provide a rationale or evidence of the decision‑making for how or why these four indicators were selected. These indicators do not adequately monitor the performance of community programs and critical issues for inpatients such as long stays, continuity of care for vulnerable groups and aspects of accessibility, as discussed in Section 3.5. The quality of DHHS's advice to its ministers is therefore impacted.
VAHI produces a range of reports with this information, which are distributed to different groups, as follows:
- VAHI Board Quality and Safety Report is sent quarterly to health service boards and CEOs.
- Inspire is sent directly to clinicians quarterly with special issues also produced for in-depth reporting on specific clinical areas. There have been two Inspire reports into mental health, which included data reported for children and youth.
- Monitor is sent to public health service boards, CEOs and DHHS quarterly, and reports performance information across measures contained in each health service's SoP.
- Program Report for Integrated Service Monitoring (PRISM) is sent to public health service boards, CEOs and DHHS quarterly, with a broader range of performance information to complement Monitor.
Sentinel event reporting to Safer Care Victoria
The Health Legislation Amendment (Quality and Safety) Bill 2017 established SCV as an administrative office of DHHS to monitor and improve the quality and safety of care delivered across Victoria's health system. It also gave the Secretary of DHHS powers to request information from health services, which has been one of the enablers of SCV's mandatory reporting of sentinel events.
Health services must report sentinel events within three days and must complete and provide to SCV a 'root cause analysis' within 30 working days.
DHHS advises that it had received a report of one sentinel event in CYMHS since SCV was established three years ago, but it could not provide evidence to the audit about this event or its treatment. There is no evidence that this sentinel event report was shared with other areas of DHHS with responsibility for monitoring quality, safety or performance such as the Chief Psychiatrist or the Mental Health Branch, nor how these different areas coordinate their various monitoring activities.
Reporting to the Department of Treasury and Finance
DHHS must report to the DTF every year on the performance of the mental health system through Budget Paper 3.
The 14 performance measures and targets relate to the whole mental health system, and are not broken down by age, so none of measures that are used for this purpose allow DTF to monitor CYMHS or children and young people's mental health.
Budget Paper 3 performance measures can be changed through negotiations with DTF during the annual state budget process, but there is no evidence that DHHS considered giving DTF visibility of the performance of CYMHS.
Given the significant economic impact of addressing mental health problems early in life, DTF should be able to monitor the performance of CYMHS as a priority area.
3.7 Monitoring the quality of service delivery
The Act prescribes three functions to the Secretary of DHHS that relate to service quality and a further six service quality functions to the Chief Psychiatrist, as shown in Figure 3I. The activities we identified around monitoring or improving service quality for CYMHS were those undertaken by the OCP.
Figure 3I
Functions in the Act for the Secretary and the Chief Psychiatrist that relate to program quality
|
The Secretary's functions include: (a) to develop and implement mental health strategies, policies, guidelines and Codes of Practice (b) to plan, develop and promote a range of mental health services that are comprehensive, integrated, accessible, safe, inclusive, equitable, and free from stigma (c) to promote continuous improvement in the quality and safety of mental health services. The Chief Psychiatrist's functions include: (a) to develop standards, guidelines and practice directions for the provision of mental health services and publish or otherwise make available those standards, guidelines and practice directions (b) to assist mental health service providers to comply with the standards, guidelines and practice directions developed by the chief psychiatrist (c) to develop and provide information, training and education to promote improved quality and safety in the provision of mental health services (e) to assist mental health service providers to comply with this Act, regulations made under this Act and any Codes of Practice (i) to conduct investigations in relation to the provision of mental health services by mental health service providers (j) to give directions to mental health service providers in respect of the provision of mental health services. |
Source: Excerpts from the Mental Health Act 2014.
Seven of the 15 KPIs that DHHS's Mental Health Branch monitors every quarter measure different aspects of service quality, which are clinical outcomes, seclusions, continuity of care and consumer participation in monitoring outcomes. However, all the KPIs have significant limitations, which we have detailed in Section 3.4.
The role of the Chief Psychiatrist
DHHS has assigned all responsibility for matters of service quality in mental health services to the OCP. The Chief Psychiatrist undertakes a wide range of activities that endeavour to improve service quality across mental health services for all children and young people, adults and aged people, such as issuing guidelines, forums, service reviews and correspondence.
Figure 3J shows the functions of the Chief Psychiatrist legislated in the Act that relate to service quality and evidence of action against each of these areas with relevance to CYMHS.
Figure 3J
OCP's actions against the Chief Psychiatrist's legislated functions that relate to service quality
|
Legislated function |
Evidence of action in 2017–19 |
|---|---|
|
(a) to develop standards, guidelines and practice directions for the provision of mental health services and publish or otherwise make available those standards, guidelines and practice directions |
|
|
(b) to assist mental health service providers to comply with the standards, guidelines and practice directions developed by the chief psychiatrist |
|
|
(c) to develop and provide information, training and education to promote improved quality and safety in the provision of mental health services |
|
|
(d) to monitor the provision of mental health services in order to improve the quality and safety of mental health services |
|
|
(e) to assist mental health service providers to comply with this Act, regulations made under this Act and any Codes of Practice |
|
|
(i) to conduct investigations in relation to the provision of mental health services by mental health service providers |
|
|
(j) to give directions to mental health service providers in respect of the provision of mental health services |
|
Key: Green = actions have fully met the legislated functions; orange = actions have not completely met legislative functions.
Source: Mental Health Act 2014; VAGO analysis of Chief Psychiatrist Annual Report 2017–18 (draft) and other documentation provided to the audit.
The audited health services confirmed that the two areas noted as 'minimal' in Figure 3J are both lacking actions by the OCP and that the lack of guidance in these areas is a cause of significant challenges for CYMHS.
External review of the OCP
In 2016, DHHS commissioned an external review of the Chief Psychiatrist's role by two senior health service managers from New South Wales, one of whom was a psychiatrist. The review made 22 recommendations about organisational structure and resourcing, engagement with health services and stakeholders, internal business processes and several matters of scope and role definition.
The OCP's internal acquittal of the review in February 2019 shows that five of the recommendations were not supported. The OCP replaced one of them with an alternate response, but the remaining four, which relate to resourcing the OCP and its scope extending to oversight of the private sector, have no explanation as to the rationale or decision-making process for their dismissal, nor any alternative response proposed to deal with the underlying issues identified by the review.
Eight recommendations have been partially implemented three years after the review and one has not been implemented at all, which was about the Chief Psychiatrist providing regular independent briefings to the DHHS Secretary, the implications of which are discussed in Section 4.4.
For three of the eight recommendations that the OCP's internal acquittal notes as fully implemented, our audit has found evidence which contradicts these assertions, which relate to:
- clarifying respective roles around sentinel event reporting with SCV
- clarifying and communicating to mental health services the respective roles of the OCP and other parts of the Mental Health Branch
- contributing to health service performance discussions.
It is unclear why the OCP would acquit these recommendations as complete when they have not been. DHHS should more thoroughly respond to this review and increase its transparency by reporting against its progress to the Minister.
Chief Psychiatrist's Guidelines
The OCP develops and issues guidelines on a range of topics. The guidelines do not differentiate between different parts of the mental health system with different models of care. As such, their implementation in CYMHS can be complex and conflict with their own health service policies. There is insufficient interpretation or implementation support provided by the OCP or DHHS.
Audited health services report that it can be difficult to determine whether communication from the Chief Psychiatrist is a mandate or directive that must be implemented under legislation, or whether it is merely advice of recommended practice that can be adapted and implemented to suit local needs. This is an important distinction that should be made clear in all communications if the impact of the mandated directives is to be upheld. The OCP does not monitor the implementation of guidelines.
The guidelines are issued to only one person in each health service, the authorised psychiatrist, which can cause delays or, on occasion, failures in delivery to those who are responsible for implementing them in CYMHS. It is a simple administrative matter to ensure distribution of guidelines to senior staff. There is no evidence that these staff change frequently in CYMHS, so maintaining a database of the the relevant names and their email addresses would not be a significant resource burden for DHHS.
Governance and 'umpire' functions
Health services described the occasional need for an 'umpire' where there are disputes or differing policies and procedures between services. For example, where there are disputes about responsibility for patients and processes for transferring patients between catchments.
The Chief Psychiatrist convenes four external committees and six internal groups that provide governance around the functions in the Act, as shown in Figure 3K. There is no evidence that these committees have considered CYMHS specifically in the past year, as their meetings are fully occupied by matters in the adult mental health system.
Figure 3K
Governance of quality and safety issues in mental health services managed by the OCP
Source: OCP.
Unreleased evaluations and reviews
The Victorian Government invested $34 million over four years in child and youth reform initiatives in 2008. $200 000 was allocated towards evaluation, which internal correspondence noted as insufficient. $100 000 was spent to undertake an internal evaluation; however, competing priorities prevented the evaluation from being finalised. The remaining $100 000 was subsequently combined with some program delivery underspend, so that $453 963 was allocated towards evaluation of the 2008 reforms.
DHHS commissioned two external evaluations, but did not release either 'due to a change in government'. The reports were titled:
- Evaluation of selected Victorian child and youth mental health reform initiatives. Stage 1 Preliminary Investigation Final Report, 31 October 2012
- Evaluation of selected child and youth mental health reform initiatives, 29 May 2013.
Audited health services advise that the findings of these two evaluations are highly sought-after and would remain relevant and useful today.
There are another 10 reviews and reports that also provide data and lessons about program quality and improvement opportunities for CYMHS that have not been released for reasons that DHHS could not explain. These documents represent a considerable expenditure of government funds and resources. Where CYMHS have directly contributed to the evaluations and reviews, withholding these reports has eroded their trust in DHHS. It is also inconsistent with DHHS's organisational value to 'generously share our knowledge'.
The University of Melbourne evaluated the Frankston Y-PARC in 2017, but only an executive summary was published. DHHS did not commission this evaluation, and ownership sits with the university and the agency that manages the Y-PARC, Mind Australia. However, as the funding body for the service, DHHS could direct and enable this evaluation to be shared with the wider sector. Further, DHHS has not sought or reviewed either the unreleased full evaluation report or the publicly available executive summary.
DHHS has also not released a comprehensive report by Alfred Health on the establishment of a dual disability service there, which Alfred Health provided to DHHS in 2018. DHHS has taken no action to communicate the project's outcomes with other CYMHS. The report contains valuable lessons for improving service quality in CYMHS. The importance of this project is discussed further in Section 4.5. Alfred Health has presented at one conference about the project, but has not discussed it more widely.
The following eight reviews and analyses of clinical mental health services, conducted or commissioned by DHHS, include specific consideration of CYMHS, but have never been released or communicated to the sector:
- Mental Health Services Strategy Data Analysis Report—Draft Report, April2018
- Reform of Victoria's specialist clinical mental health services: Advice to the Secretary, December 2017
- DHHS Linkage, Modelling and Forecasting Section, Mental Health 2018–23 Services Strategy analysis—Draft, 2018
- Design, Service and Infrastructure Planning Framework for Victoria's Clinical Mental Health System, April 2017
- Consultation paper Clinical mental health service catchments, August 2013
- Review of acute mental health assessment and treatment for Victorian children aged 0–12 Summary Report, April 2010
- Next steps 0–25 Next Steps in Mental Healthcare Reform for Children, Young People and their families: Guidance for state-funded specialist mental health services, August 2012
- Victorian Department of Health and Human Services' Expert Taskforce on Mental Health, 10-year mental health plan wave 2 priorities—discussion paper, 28 June 2016.
All relevant lessons learned from these 12 evaluations and reviews, and where possible complete reports, should be released to CYMHS leaders, and more widely to consumers and the general public, so they can be used to inform service development and quality improvement.
3.8 Monitoring outcomes
Monitoring outcomes is a significant priority for all mental health services and for the Victorian Government, but there are some significant failings in DHHS's approach to monitoring outcomes in CYMHS.
In a March 2019 publication about the Victorian Government's commitment to 'outcomes-thinking', the Secretary of the Department of Premier and Cabinet stated that:
The best way to deliver public value to the people of Victoria is to clearly define the outcomes we are trying to achieve, and measure progress along the way.
There is no evidence that DHHS has asked a CYMHS to explain its performance with regards to outcome measures—neither their collection nor the results.
DHHS's Health and Wellbeing Outcomes Framework
DHHS's Health and Wellbeing Outcomes Framework, published in 2016, includes as an outcome that 'Victorians have good mental health', but none of the targets monitor the wellbeing of children and young people who have mental health problems nor the effectiveness of government programs to assist them. The selected outcomes measures take a prevention and population health approach to mental health, which is important, but does not allow for any outcome monitoring for people with more severe mental health problems that are using CYMHS.
The outcomes framework is not an effective mechanism for monitoring outcomes of CYMHS or the children and young people with mental health problems who CYMHS supports.
The one target against the outcomes is a 20 per cent increase in resilience of adolescents by 2025, which comes from the government's education policy, 'Education State'. Three of the measures defined against this outcome relate to children and young people, which are:
- the proportion of adolescents who experience psychological distress
- the proportion of adolescents with a high level of resilience
- the proportion of children living in families with unhealthy family functioning.
The suicide rate is also a measure, but it is not broken down by age to measure the rate for children and young people specifically.
10-year Mental Health Plan outcomes framework
DHHS's 10-year plan defines 16 outcomes and DHHS has developed indicators and measures for 10 of these. It reports progress against the indicators in its annual report to the Minister for Mental Health and publishes the report on its website.
Four of the 34 indicators relate to children and young people with severe mental health problems, as shown in Figure 3L. A further 18 of the indicators would provide useful information about CYMHS and its clients; however, they are only reported for adults or for the whole system, so children and young people cannot be separately monitored.
Figure 3L
Indicators in the 10-year mental health plan that relate to children and young people with severe mental health problems
|
Indicator |
Reference year |
Two years prior |
One year prior |
Most current data |
|---|---|---|---|---|
|
Proportion of Victorian young people with positive psychological development |
2016 |
70.1% |
n/a |
68.8% |
|
Proportion of children at school entry at high risk of clinically significant problems related to behaviour and emotional wellbeing |
2017 |
4.6% |
4.8% |
4.9% |
|
Proportion of Victorian Aboriginal children at school entry at high risk of clinically significant problems related to behaviour and emotional wellbeing |
2017 |
14.2% |
15.6% |
14.4% |
|
Proportion of registered clients experiencing stable or improved clinical outcomes (children and adolescents) |
2017–18 |
90.6% |
91.3% |
90.6% |
Source: DHHS Mental Health Services Annual Report 2017–18.
- DHHS has not developed indicators or measures to monitor four other outcomes in its framework that relate to the wellbeing of children and young people with severe mental health problems. These outcomes are that Victorians with mental illness:
- participate in learning and education
- participate in and contribute to the economy
- have financial security
- are socially engaged and live in inclusive communities.
DHHS advises that it has developed an indicator for CYMHS clients' participation in learning and education, but this was not being used at the time of the audit and DHHS could not provide any evidence of this work. Our analysis of data from the five audited CYMHS shows that education and economic indicators are a significant issue for CYMHS clients, as seen in Figure 3M. We found 65 CYMHS clients of school age who had never attended school, while 19 per cent of clients over the age of 15 years were not employed or in any education program.
Figure 3M
Number of clients with 'education status' recorded as 'not at school' or 'unemployed/pensioner'
Note: Analysis is limited to the 12 848 CYMHS clients over three years to 31 December 2018 who had their education status recorded in the clinical database.
Source: VAGO analysis of information from five audited health services.
Our 2019 audit Access to Mental Health Services also found significant failings in the outcomes selected for the 10-year plan, with the following finding:
There are few measures in the outcomes framework for the 10-year plan that directly capture performance against providing access to services or increasing service reach—this despite the acknowledged performance problems in this area—which shows a lack of focus on the most pressing issue the system faces.
Nationally agreed outcomes collection
|
A self-rating measure is a survey that asks clients, or their parents, or both, to rate various aspects of their health and wellbeing. The surveys are used as a part of therapeutic care and the results can also be used to inform research and service development. The most commonly used self-rating measure in Australian clinical mental health services is the SDQ, which has three different versions: one for parents of children, one for parents of youth and a youth self-report version. |
Under the Second National Mental Health Plan, endorsed in 1998, all Australian states and territories committed to routine collection of outcomes data in public mental health services. The National Outcomes and Casemix Collection (NOCC) was first specified in August 2002. It outlines the agreed national minimum requirements and includes a set of protocols about the times and points in service delivery when each outcome should be collected. The outcomes include a mix of self-rated and clinician-rated assessment tools.
The NOCC protocols require CYMHS to collect seven different outcomes for all clients and they specify whether they need to be collected at admission, review, discharge, or all three points, which varies between inpatient, community residential or ambulatory settings.
DHHS monitors compliance with three elements of the NOCC protocols, by having KPIs for health services:
- completing the HoNOSCA outcome tool
- offering a self-rating outcome measure to inpatients only
- completing a self-rating measure.
CYMHS's performance against these KPIs shows that their completion of outcome measures varies between different settings and between services, as shown in Figure 3N.
Figure 3N
Completion of the HoNOSCA outcome measures in April to June 2018 by health service
Source: VAGO from DHHS website quarterly CAMHS KPIs.
DHHS's guidance to health services, Outcome measurement in clinical mental health services, published on its website, has not been reviewed since 2009 and contains errors. It states that the NOCC outcomes for 'community residential' are not applicable in Victoria for children and adolescents, despite such facilities now existing. Elsewhere on the DHHS website there is guidance on implementing the NOCC protocols that differs from this publication in stating whether measures should be collected at intake or admission.
International Declaration on Youth Mental Health
The United Kingdom's Association for Child and Adolescent Mental Health together with the International Association for Youth Mental Health published a declaration on youth mental health in 2011 and updated it in 2013. The declaration sets eleven 10-year targets for service provision for young people aged 12–25 years.
Benchmarking performance against other organisations or consensus targets like the international declaration is an important and effective strategy to identify opportunities for improvements in systems and processes. DHHS has never benchmarked Victorian CYMHS against these international targets and it does not collect the relevant data or other information to allow it to monitor them. For some of the targets, DHHS does not collect data in the right format, such as breaking down suicide rate by age. For other targets, DHHS has data that would allow some monitoring, but it has never done so, such as using CMI data to monitor accessibility, as discussed in Section 3.5, or the user-experience survey data, which it collects but has never analysed or used.
If DHHS proceeds with its commitment to develop strategic directions under its Clinical Mental Health Services Improvement Implementation Plan, which this audit recommends, it should consider benchmarking against the international targets. It should share the results of the benchmarking with CYMHS leaders and involve them in developing strategies to address any discrepancies identified between Victorian CYMHS's performance and the international targets. DHHS should also rectify the issues described in Figure 3O in regards to its capacity to monitor the important issues covered by the international targets.
Figure 3O
Relevant(a) targets in the International Declaration on Youth Mental Health and DHHS's ability to monitor each
|
Target |
Available data or system to monitor? |
|---|---|
|
1. Suicide rates for young people aged 12–25 years will have reduced by a minimum of 50 per cent over the next 10 years. |
The Victorian population's suicide rate is not measured or reported by age. |
|
5. All young people and their families or carers will be able to access specialist mental health assessment and intervention in youth-friendly locations. |
Location of services is not monitored. |
|
6. Specialist assessment and intervention will be immediately accessible to every young person who urgently needs them. |
Accessibility or time lines of access is not monitored, as discussed in Section 3.5. |
|
7. All young people aged 12–25 years who require specialist intervention will experience continuity of care as they move through the phases of adolescence and emerging adulthood. Transitions from one service to another will always involve a formal face-to-face transfer of care meeting involving the young person, his or her family/carers and each service involved in his or her care. |
The KPI for follow-up applies only to inpatients and does not monitor the type of transition service provided. |
|
8. Two years after accessing specialist mental health support, 90 per cent of young people will report being engaged in meaningful educational, vocational or social activity. |
Not monitored, though the CMI database does collect information which shows poor outcomes, with 19 per cent not engaged. |
|
9. Every newly developed specialist youth mental health service will demonstrate evidence of youth participation in the process of planning and developing those services. |
Youth participation in CYMHS is not monitored. |
|
10. A minimum of 80 per cent of young people will report satisfaction with their experience of mental health service provision. |
DHHS's Your Experience of Service (YES) survey is completed by people aged over 16 years using mental health services. In the three months March to May 2018, 1 051 people aged 16–25 years completed the survey. The survey is not mandatory and health services administer it at widely differing rates. There is no evidence that DHHS analyses the results for under 25-year-olds CYMHS clients nor uses them to monitor performance. |
|
11. A minimum of 80% of families will report satisfaction that they felt respected and included as partners in care. |
The YES survey asks the young person's perception of their family's experience. Families themselves are not surveyed. |
(a) Three of the targets relate to prevention and workforce issues that were out of scope for this audit.
Source: VAGO analysis of information provided by DHHS and the '10-year targets' in the International Declaration on Youth Mental Health published by the International Association for Youth Mental Health, October 2013.
Audited health services' outcomes monitoring
In addition to the outcome measures mandated by DHHS and NOCC, RCH has begun to use 10 tools to measure and monitor clinical outcomes. The selected tools are freely available and are commonly used in research, allowing RCH to benchmark outcomes for their clients nationally and internationally. The tools are rating scales and questionnaires developed for specific disorders, such as anxiety, obsessive compulsive disorder and suicidality, and are all tailored to children and young people.
DHHS was not aware of this work, possibly because it had not convened its six-monthly program meeting with RCH for nine months at the time of the audit and the work had occurred during that period. This represents a missed opportunity for DHHS to share RCH's work with other health services.
3.9 Data collection and reporting to DHHS
The Mental Health Branch requires CYMHS to report all client contacts and information through a computer application called CMI, which delivers data into a central database managed by DHHS called the operational data score (ODS).
DHHS has a manual that provides guidance on how to report activity into CMI. The manual is not publicly available, and DHHS advises that the manual is out of date and being updated, but could not provide evidence of the process or the expected completion date.
DHHS also communicates some reporting requirements to health services in a series of bulletins published on its website. Each relates to a specific matter, such as 'recording admissions' or 'deceased clients'—there is no single source of information on CMI and its reporting requirements except for seeking advice from the DHHS staff who are responsible for maintaining the database. CYMHS independently convene a network of their health information managers to provide support and upskilling to these specialised staff.
Our analysis of some CMI/ODS data (see the scope and methodology in Appendix D) identified some significant gaps in the information that can be entered into the database and the usefulness of other information that is entered, due to there not being any current guidance on terminology and definitions of fields.
We found the following specific issues with the CMI database:
- The 'legal status' information that can be recorded on DHHS's printed client registration forms does not have a corresponding field and cannot be entered into the CMI/ODS database.
- The 'sex' field on the client registration form and in the CMI database only include the options 'male' and 'female', which is not consistent with the Victorian Government's guidance on inclusive language. DHHS advises that it is working to improve mental health services' collection of sex/gender information in line with the 'Rainbow Tick' national accreditation program for organisations that are committed to safe and inclusive service delivery for lesbian, gay, bisexual, transgender and intersex people. There is no evidence yet of implementation in CYMHS.
- 'Living arrangements' has 20 response options that are not mutually exclusive or defined with business rules.
- 'Living status' response options include 'acute hospital' and 'psychiatric hospital', but there are no business rules to explain the distinction or why these would be an individual's place of residence.
- The 'carer relationship' field has 24 response options that are not defined or clearly described.
- The 'carer' field is used by health services to record the client's medical professional's details, which should be a separate and different field.
- Health services recorded 15 CYMHS clients born in Adelie Land, a French‑claimed territory in Antarctica. This is likely to be a data entry mistake, as Adelie Land is the first option for country of birth in the alphabetic list on CMI and no respondent in the 2016 census was born there. During the audit, DHHS advised that it had introduced validations to identify this and ensure corrections are made.
- Health services can create their own response options for many fields in the database, which creates inconsistent data that is difficult to analyse at the sector or statewide level.
DHHS owns the CMI database and is responsible for managing and maintaining it. The Mental Health Branch uses this data to generate the KPI reports it uses to monitor CYMHS performance. It advised us that making changes to the database is difficult because it is managed by a different area within DHHS whose resources are stretched. DHHS's Digitising health strategy, published in 2016, notes 'Mental health modernisation' as a priority. DHHS advises that significant work is underway, including the appointment of a provider to transition the CMI/ODS database to a new platform. However, DHHS could not provide evidence of progress, methodology or timelines for this activity.
DHHS does not review whether CMI is collecting the appropriate and necessary information and was not aware of the failures of the CMI system that we identified through our analysis.
As a result of these database issues, DHHS cannot understand many important components of CYMHS, such as whether they are providing services to vulnerable populations, or the complexity and vulnerability of the clients who do access CYMHS. Without an accurate way to collect this information, DHHS cannot appropriately monitor the performance of CYMHS. The problems with collecting this information will also impede DHHS's ability to describe performance issues to government and advocate for additional resources where they might be needed.
4 Access and service responses for vulnerable populations
Mental health problems increase exponentially when there are other indicators of vulnerability, such as unstable housing and poverty, neglect and abuse, intergenerational trauma or developmental disabilities.
Both individuals and the society they live in substantially benefit from timely wrap-around care that coordinates the many services that can be involved for these most vulnerable children and young people.
4.1 Conclusion
Under-resourcing combined with a lack of DHHS service coordination and oversight mean that many vulnerable Victorians cannot access CYMHS for the support they need. Those who do get access often need multiple providers that are unable to coordinate around their shared clients' needs. This lack of coordination places pressures on CYMHS, which have become the last resort for 'housing' young people who disability and child protection services have not been able to support. DHHS's patchy and often reactive approach to system oversight has impacted its ability to identify systemic failures that are causing harm to vulnerable children and young people.
4.2 Prioritising access to vulnerable groups
DHHS has not identified priority populations for CYMHS nor enabled health services to prioritise access at the local level. DHHS advises that it is not its role to identify priority populations for CYMHS, but that individual health services in Victoria's devolved health system are responsible for managing access and any priority populations at the local level.
DHHS advises that its Policy and Funding Guidelines 2019–20 will include a new statement about prioritising access for vulnerable populations, though there is no evidence that DHHS has taken any action to enable this nor has any plans to monitor it. The statement to be included is:
Vulnerable children and young people, particularly those involved with statutory services such as child protection, are prioritised.
Our analysis of three years of clients at the five audited health services shows that the rates of vulnerable client groups accessing CYMHS is low compared to less vulnerable groups.
People from culturally and linguistically diverse backgrounds are less likely to seek help for mental health problems, but no less likely to experience problems. Figure 4A shows that the majority of CYMHS clients are born in Australia and access CYMHS at a rate proportionate to their share of the total Victorian population aged under 25 years. People who were born in Southern Europe, Asia and on the Indian Subcontinent are underrepresented as CYMHS clients. The percentage of CYMHS clients from these three regions is less than half of what we would expect if they were accessing CYMHS at a rate proportional to their share of the Victorian population. Young people from these regions are at risk of not accessing the mental health services they need.
Refugees are more likely to have experienced trauma than the general population and are at greater risk of mental health problems as a result. Our data analysis shows that young people born in Sub‑Saharan Africa, who are frequently refugees who have experienced trauma, are accessing CYMHS at a higher rate than their population share, but there is no evidence to show whether this rate is commensurate with the mental health needs of the population given its experience of trauma.
DHHS funds a torture and trauma counselling service, which is accessible to children and young people, but it has not evaluated it and so was not able to provide any information on the reach or impact of this program in supporting young people. Other CYMHS therefore miss out on any learnings from this initiative.
Figure 4A
Country of birth for CYMHS clients compared to country of birth for the total Victorian population aged 0–25 years
|
Region of birth |
Percentage of Victorian population aged 0–25 |
Percentage of CYMHS clients |
Percentage of expected numbers in CYMHS |
|---|---|---|---|
|
Australia |
79.87 |
79.21 |
99 |
|
Other Asia |
6.07 |
2.18 |
36 |
|
Indian Subcontinent |
3.02 |
1.47 |
49 |
|
English speaking countries in Northern Europe and North America |
1.47 |
1.12 |
76 |
|
New Zealand and South Pacific |
1.41 |
1.28 |
91 |
|
Middle East and North Africa |
1.06 |
0.72 |
68 |
|
Sub-Saharan Africa |
0.88 |
1.08 |
123 |
|
Western Europe |
0.28 |
0.19 |
68 |
|
Eastern Europe |
0.24 |
0.22 |
92 |
|
Southern Europe |
0.21 |
0.09 |
43 |
|
Latin America |
0.17 |
0.18 |
106 |
|
At sea |
0.00 |
0.01 |
0 |
|
Not stated/inadequately described/no data |
5.30 |
12.18 |
230 |
Note: Countries of birth were assigned to a region based on the categories used in either the DHHS report Racism in Victoria and what it means for the Health of Victorians or the ABS's geographical categorisations.
Source: VAGO, based on ABS Census 2016 population figures.
Use of an adult triage process
|
Mental health triage is the initial process to determine whether a person needs further assessment by a mental health service, and the type and urgency of the response required from mental health or other services. |
DHHS introduced a Statewide Mental Health Triage Scale and guidelines in 2010 and has not reviewed it in the nine years since. The scale is still used by all audited CYMHS. It focuses on clinical urgency, specifically risk of physical harm to self or others. It does not give any focus to developmental or cumulative risks that are critical for children and young people, does not capture the severity or longevity of mental health problems, and does not enable prioritising access for high-risk and vulnerable groups of children or young people.
A quality triage process requires a clinical tool to assess urgency, but the tool itself does not and cannot take into consideration other important factors that must influence the triage process, such as severity, complexity, quality of care, workload and staffing. DHHS does not provide any current guidance to CYMHS on triage processes or assessing any of these matters.
The triage approach is the same across all age groups, despite the 2010 guidelines identifying the following six challenges particular to triaging mental health issues in children and adolescents, namely:
- not recognising lower-order autism spectrum disorders
- confusing post-traumatic stress disorder symptoms with psychosis
- failing to identify depression, especially when it is masked by aggression or other forms of acting out
- dismissing some symptoms—for example, self-harming behaviour in girls, rage attacks in prepubescent boys—as personality or behaviour issues not requiring mental health services
- underestimating the risks involved when self-harming behaviour is new, as opposed to longstanding
- not acknowledging that obsessive eating behaviours may be early signs of eating disorders.
While the triage tool does not cater to the needs of children and young people, if it is used by clinicians experienced in working with children and young people some of the risks could be minimised. However, our data analysis from the five audited health services showed that 118 children aged 18 years and under were triaged through either an adult or aged-care system response. A further 115 were admitted to an adult Crisis Assessment Team, who provide a 24-hour urgent assessment and brief, intensive treatment service. The audited CYMHS advise that their triage systems only operate during business hours and week days, and outside of these times, clients calling or attending emergency departments will be diverted to an adult triage service. This creates the risk that a clinician without CYMHS experience may underestimate the risk factors specific to young people and may triage the young person incorrectly.
DHHS has not taken any action to develop a triage approach that recognises the developmental risks for children and adolescents, or that would enable health services to prioritise access for particular population groups.
Aboriginal and Torres Strait Islander young people
There is no data available about the mental health of Aboriginal and/or Torres Strait Islander (Aboriginal) young people in Victoria, specifically. However, Aboriginal young people experience significantly worse mental health outcomes nationally, with four times the rate of suicide, for example.
DHHS's Balit Murrup: Aboriginal social and emotional wellbeing framework 2017–2027 does not make any specific commitments about young people because its focus areas are mostly at the community level. The framework describes relevant new investments, which include some young people-focused initiatives—a youth mentoring program and support for Aboriginal children in out‑of‑home care and youth justice. DHHS advises that a project targeting families at risk of children needing out-of-home care is underway with positive results and an evaluation planned, but was unable to provide evidence of the progress of any other initiatives targeting children and young people or progress against the strategy itself.
The 2016 census showed that 1.4 per cent of 0–24 year-olds residing in Victoria identified as Aboriginal, although a considerably higher proportion of CYMHS clients, 2.4 per cent in the five audited health services, identified as Aboriginal. Without comparable Victorian population data on mental health problems in Aboriginal young people, we cannot determine whether 2.4 per cent is an appropriate proportion of Aboriginal clients to be accessing CYMHS. However, as Aboriginal children are 12 times more likely to be in out-of-home care than non-Aboriginal children, and Aboriginal people are nearly three times as likely to experience high or very high level of psychological distress, DHHS should monitor the rate that Aboriginal young people access CYMHS to ensure that they are getting the mental health support they need.
Homelessness and supported accommodation
In our analysis of five health services over three years, 596 CYMHS clients, or 3 per cent, lived in supported or unstable types of accommodation. The majority of these (56 per cent) were in community or supported residential accommodation. A further 10 per cent had their residence recorded as an acute or psychiatric hospital though, as discussed in Section 3.9, there are no business rules around recording this data so it is not clear what this represents.
Homelessness was recorded for 0.3 per cent of CYMHS clients at the five audited health services, while the 2016 census showed that a higher proportion, 0.5 per cent of Victorians aged 0–24 years, were homeless or living in unstable housing. The prevalence of mental health problems in young people who are homeless is not known, but DHHS data collected from 13 617 rough sleepers found that mental health problems had contributed to 27.5 per cent of those surveyed becoming homeless. We would expect that young people who were homeless or in unstable housing would have a higher rate of mental health problems and be a larger group of CYMHS clients.
DHHS does not publicly report on the number of young people living in supported accommodation, so we cannot confirm whether these young people are accessing CYMHS at the expected rate. DHHS could use their internal data to explore this question further and should do so.
Figure 4B
CYMHS clients in five audited health services 2016–18 by age and housing
Note: Business rules are not defined for CMI housing fields. It is unclear under what circumstances a young person would be registered as living in an acute hospital or a psychiatric hospital.
Source: VAGO analysis of CMI data provided by five audited health services. See Appendix D for data analysis scope and methodology.
Children in out-of-home care
The OCP developed a guideline for health services on prioritising access for young people in out-of-home care in 2011 but has not reviewed it despite the guidelines having been scheduled for review in 2013, and the Act changing significantly in 2014. One audited health service was not aware that the guideline existed. DHHS advises that it is available on its website, but it is not on the Chief Psychiatrist's website page where other guidelines are listed. It can be found online as part of the DHHS Child Protection Manual.
Only one of the five audited health services had a documented procedure for prioritising access to children in out-of-home care. Two other services had statements about prioritising access to children in out-of-home care, one of which extended to also include Aboriginal and Torres Strait Islander children with psychosis, eating disorders and school refusal, but neither had a documented process for how this occurs. The remaining two services had no policy or procedure on prioritising access.
The child specialist program, which was newly funded in 2016–17, has a deliverable that services develop protocols between CYMHS and child protection, but there is no evidence of any progress with this nor any evidence that DHHS is attempting to monitor progress.
DHHS's reporting system does not collect any information about whether a child is in out-of-home care or if there are any other legal orders around their guardianship, disability or other health or welfare problems. The registration forms health services must complete for every mental health client include a place to record that a client has legal orders under the Children, Youth and Families Act 2005, but it is on the second, non-mandatory, page of the form and is one of several options under the heading 'other legislation', as shown in Figure 4C.
Figure 4C
Excerpt of mental health service registration form PR1A, which health services complete for all mental health clients
Source: Excerpt of DHHS's client registration forms provided by Austin Health.
Even if this field is ticked on the hard copy form, there is no place in the electronic database to input the information. Subsequently, DHHS has no way to monitor whether children in out-of-home care are accessing CYMHS or any information about this priority population group at all. Most health services operate parallel client management databases where this additional information can be recorded and is accessible to clinicians.
When this issue was identified, we attempted to determine the extent to which children in out-of-home care had been able to access CYMHS through other means. There are database fields which could potentially provide this information, but they fail to provide a reliable source of information, as follows:
- 'Referral source' is an optional field and was only populated for 9.7 per cent of the 18 460 clients whose data we analysed, which was insufficient to undertake any meaningful analysis.
- 'Housing' does not contain a response option for 'out-of-home care' or any similar term.
- 'Carer relationship' is predominantly used to record a client's general practitioner, although 95 clients were identified here as having either a 'case manager', 'appointed guardian' or 'appointed administrator', but there are no definitions for each field so their use cannot be relied on to inform accurate data.
4.3 Clinically unnecessary inpatient stays
Young people frequently stay in inpatient mental health facilities for longer than they need to be because their guardianship and/or housing arrangements change during, or as a result of, their hospital admission. One senior staff member advised us, 'you can't discharge children to homelessness'.
DHHS has not recognised the extent to which this occurs and the significant negative impacts on the young people and families involved as well as the very significant resource and workforce implications the issues present to health services.
DHHS does not strategically monitor extended stays (stays beyond clinical necessity), or any other matters relating to young people with multiple and complex needs, despite being advised of it repeatedly over many years by health services. While some of the drivers of these problems are complex social and family issues, DHHS has not taken any strategic action to address the system issues around service coordination for these people, which they do have the ability to improve.
DHHS does not have long-term housing or care options for young people with multiple and complex needs. In 2015–17, a young person was a CYMHS inpatient for two years because no agency could find a suitable housing service to meet their needs. DHHS had to find and modify a house for this patient to be discharged to. In other similar cases, DHHS waits for the young person to turn 18 so they can be discharged to adult accommodation.
How often this happens cannot be determined through the current systems of data collection and monitoring, but during our audit we worked closely with senior CYMHS clinicians and an independent subject matter expert to design an approach that would allow us to explore the extent of clinically unnecessary inpatient stays.
Health services advised that there are too many occurrences where a portion of a consumer's time in the hospital is clinically unnecessary for the service to document every case during the time of the audit. Instead, a selection of examples from recent years was provided to the audit team by senior clinicians who were involved in providing and coordinating care to the relevant clients and who also had the skills and authority to determine at what point in the person's inpatient stay it became clinically unnecessary.
Case studies of clinically unnecessary inpatient stays
The five audited health services provided us with 29 detailed examples of young people whose recent inpatient stay included a period that was clinically unnecessary. These inpatient stays ranged from two to 254 days, making a cumulative total of 1 054 days, or almost three years. Time periods for the case studies varied, but all were within the past 12 months and one service presented eight such cases within a six-month period.
Figure 4D
Summary of case studies of clients with wholly or partly clinically unnecessary extended inpatient stays
|
Age group |
Presence of intellectual or developmental disabilities |
Total length of stay |
Length of stay clinically unnecessary |
|---|---|---|---|
|
12–15 years |
Yes |
approx. 268 days + ongoing |
approx. 254 days + ongoing |
|
18–25 years |
No |
212 days + ongoing |
212 days + ongoing |
|
16–18 years |
Yes |
267 days |
189 days |
|
18–25 years |
No |
125 days |
70 days |
|
18–25 years |
No |
169 days |
60 days |
|
16–18 years |
No |
42 days |
34 days |
|
18–25 years |
No |
52 days + ongoing |
30 days + ongoing |
|
13–15 years |
Yes |
53 days |
30 days |
|
13–15 years |
No |
71 days |
30 days |
|
16–18 years |
Yes |
approx. 55 days + ongoing |
at least 21 days + ongoing |
|
16–18 years |
No |
43 days |
16 days |
|
16–18 years |
Yes |
Ongoing (58 days) |
14 days |
|
13–15 years |
Yes |
12 days |
12 days |
|
13–15 years |
Yes |
13 days |
10 days |
|
16–18 years |
No |
11 days |
9 days |
|
16–18 years |
Suspected |
12 days |
9 days |
|
0–12 years |
No |
approx. 35 days |
approx. 7 days |
|
0–12 years |
Yes |
10 days |
7 days |
|
13–15 years |
No |
13 days |
6 days |
|
16–18 years |
No |
12 days |
6 days |
|
16–18 years |
No |
13 days |
5 days |
|
0–12 years |
Yes |
6 days |
5 days |
|
16–18 years |
No |
5 days |
4 days |
|
16–18 years |
No |
3 days |
3 days |
|
13–15 years |
No |
5 days |
3 days |
|
13–15 years |
Yes |
2 days |
2 days |
|
16–18 years |
No |
3 days |
2 days |
|
13–15 years |
Yes |
2 days |
2 days |
|
16–18 years |
Yes |
2 days |
2 days |
Note: We conducted fieldwork in the last two weeks of January 2019. 'Ongoing' refers to consumers who were inpatients at that time with no fixed discharge date.
Source: VAGO, based on clinician interviews.
To protect these young people's privacy, the audit will not report the case studies collected and analysed, but instead focus on the system issues that our analysis of the case studies revealed.
System failures identified
We found four main types of system failure through analysis of the case studies, namely:
- the family's (or out-of-home carer's) inability to cope at home with the young person's challenging behaviours
- the family's inability to participate in therapeutic care at hospital
- failure of disability services, including failure to repair damaged disability accommodation and failure to receive NDIS supports
- failures relating to child protection, including failure to engage or organise placements in a timely manner, including when abuse is disclosed during an inpatient stay.
If health services' local relationships fail to resolve system issues for complex clients, there are no mechanisms to escalate them. The Chief Psychiatrist's support and advice is frequently sought, though not routinely, and there is no established mechanism that can be applied to resolve barriers to discharging children who are 'stuck' in inpatient units.
Health services described examples where they had failed to gain a timely response from local disability and child protection workers. In several cases, senior clinicians attributed the delay to a lack of understanding of the serious negative impacts on a child or young person from being in a mental health facility beyond clinical necessity. This included a perception from other services that the child was in a safe place. This view contrasts with the opinion of mental health practitioners that the young person's health and wellbeing was deteriorating because of the inpatient stay.
The resource implications of clinically unnecessary inpatient stays are also significant. The 1 054 bed days in the past 12 months that we found through our case studies equates to $750 448 of direct funding, given the DHHS bed price for child and adolescents is $712 per day. Given that the actual cost of inpatient mental health beds exceeds the funding provided, as discussed in Section 2.3, and that higher staffing ratios and use of facilities—such as multiple beds for one complex client—are common place, as discussed in Section 4.5, the actual cost will far exceed this amount.
Failure to get NDIS supports in place for young people with dual disability
There were several examples of the NDIS contributing to a young person's inpatient stay extending beyond clinical necessity. In at least two cases, an NDIS plan did not exist yet or did not include a high enough level of support for the child to be discharged from hospital, and CYMHS staff were writing applications or appeals to the National Disability Insurance Authority while the young person remained an inpatient. In another example, an extensive NDIS plan had been approved and funded, but the family had not engaged the services, preventing discharge.
During the audit, DHHS undertook a 'data snapshot' with responses from nine health services. It identified 11 consumers, in an unknown timeframe, who had clinically unnecessary inpatient stays totalling 336 days, and a further 15 consumers with a total of 966 days of clinically unnecessary stays in bed‑based rehabilitation settings. DHHS did not report if any of these consumers were children or young people, and noted the low response from health services means the data is likely a significant under-estimate of the problem.
DHHS is referring to this issue as 'social admissions', with the following definition:
Social admissions involve participants being relinquished by their carers or NDIS providers at Emergency Departments and subsequently admitted into inpatient care, without a clinical need to be admitted or remain in hospital. This cohort often presents with complex support needs, primarily in relation to acute behaviours of concern associated with multiple disabilities which in many cases is not associated with a mental health presentation.
This data snapshot is part of a detailed analysis of 'social admissions', which is an emerging issue for clinical mental health services. The snapshot considers drivers and impacts, as well as service gaps that contribute to the problem. The analysis notes that DHHS is putting other interim data collections in place to calculate clinical hours dedicated to NDIS-related activity and the numbers of 'social admissions', with plans to amend the ongoing data collection to include these issues.
DHHS's actions to understand and address this issue have been insufficient and slow. During the audit, in 2019, DHHS was identifying funding requirements resulting from the impact of the transition to the NDIS on clinical mental health services and its clients. In February 2019, DHHS launched a website to increase the clinical mental health workforce's 'literacy on the NDIS'. These actions are occurring three years after the full NDIS rollout commenced 1 July 2016 and six years after the trial sites began in 2013. Our audit found examples of CYMHS clients having clinically unnecessary stays as a result of problems with access to NDIS funding for accommodation dating back to 2016 and that DHHS was aware of the issue at this time.
There is activity underway to improve client information sharing and other collaboration between clinical mental health services and the National Disability Insurance Agency. This is being progressed through a series of inter-jurisdictional committees.
The focus of DHHS's work around mental health and the NDIS is people with psychosocial disability, which is a term used to describe a disability that may arise from a mental health issue. Most young people with 'dual disability', which CYMHS support and this audit examined, do not meet the criteria for having a psychosocial disability. Instead, they have intellectual or developmental disabilities that are complicated by serious mental health problems. There is no evidence that DHHS's work to improve the interface between clinical mental health services and NDIS includes this group of clients nor has any focus on CYMHS's particular issues or needs, which can be different from the adult mental health system
DHHS needs to expand the work that it is now commencing to improve the interface between clinical mental health services and the NDIS to specifically include the needs of CYMHS and young people with dual disability as soon as possible.
Long stays in CYMHS inpatient facilities
Long stays in inpatient facilities can be both a partial indicator of clinically unnecessary stays and a system failure in their own right that should be monitored.
Children and young people's mental health and wellbeing can deteriorate when their inpatient stay are long, and even more so when they are clinically unnecessary. They commonly experience escalations in their frustration, which can lead to aggressive behaviours. This can have the following consequences:
- Staff may need to use restrictive interventions (such as seclusion, sedation or restraint) to manage a child or young person's behaviour, which can be traumatising for them.
- Children and young people may be violent and abusive to staff in the inpatient unit.
- Children and young people who have escalated, especially those who are not staying in a high-dependency area and are free to move about the unit at will, may frighten other children and young people. These other young people may not only be traumatised by aggressive behaviour they have witnessed in the unit, but may not have received adequate treatment and as a result may be more likely to present in crisis at a later date.
- Agitated children and young people may damage facilities, leading to expenses for the health service and further bed closures while the unit is repaired.
Monitoring long stays is quite achievable with the current data collection systems, and is done for the adult mental health system, but DHHS does not monitor long stays for CYMHS. DHHS could not provide any rationale for this.
Our data analysis showed that over three years there had been 228 inpatient stays greater than 35 days (a long stay) for clients aged 0–25 years in the four health services we looked at. Figure 4E shows that long stays are only 3 per cent of the total number of inpatient stays, which may explain them being missed by DHHS. However, they represent a significant resource burden that should be monitored and better understood.
Figure 4E
Number of admissions by length of stay for four audited health services 2016–18
Note: Admissions recorded as zero days are generally part of a planned discharge or recovery program where the young person is admitted to the inpatient facility for a day and returns home before evening.
Source: VAGO analysis of information from audited health services, January 2019.
The long stays are distributed across the four audited health services that we analysed despite their different models of care, as shown in Figure 4F below.
Figure 4F
Number of long inpatient admissions (35 days or more) for 0–25 year-olds during 2016≠–18, by audited health service
|
Health service |
Number of long admissions |
|||
|---|---|---|---|---|
|
0–17 year-olds |
18–25 year-olds |
Age unknown (a) |
Total |
|
|
AWH |
4 |
24 |
28 |
|
|
Austin Health |
49 |
45 |
94 |
|
|
Eastern Health |
18 |
48 |
4 |
70 |
|
RCH |
36 |
0 |
36 |
|
|
Total |
107 |
117 |
4 |
228 |
(a) Age at admission unknown but these clients were identified as 0–25 years during 2016–18 through other service contacts.
Note: Monash Health was excluded because our data analysis could not separate the long inpatient stays from community residential stays in their Y-PARC or PARCs.
Source: VAGO analysis of information from audited health services.
Our analysis did not allow for separating Monash Health's Y-PARC data from its inpatient unit admissions, so we cannot report a count of long stays at Monash Health that is comparable to the other audited services. DHHS could undertake further analysis of the CMI data that it collects to determine the extent of long stays at Monash.
There are also significant impacts on the workforce from long and/or clinically unnecessary inpatient stays, which audited health services describe as including:
- personal wellbeing burden on staff experiencing sustained aggression from clients with challenging behaviours
- increased supervision for staff involved in care to debrief difficult shifts and develop skills in working with challenging behaviours
- increased sick leave rates and therefore increased costs for backfill
- challenging staff morale.
These are clearly clients with complex needs, as our data analysis showed that they accounted for a total of 652 admissions and 25 per cent of the total bed days that we reviewed. Of the clients with a long admission of 35 days or more, 64 per cent had other admissions during the three-year period we analysed.
We reviewed the diagnostic codes that health services had recorded against these clients to understand the types of mental health problems and complexity that this group experienced. Their diagnoses include the following:
- acute psychiatric, for example schizophrenia—70 per cent
- anxiety disorder—38 per cent
- problems with the social or home environment—45 per cent
- additional medical diagnosis requiring hospital treatment—63 per cent
- depressive mood disorder—29 per cent
- eating disorder—28 per cent
- self-harm—19 per cent
- developmental disability—18 per cent
- maltreatment syndromes, assault or adverse childhood—17 per cent
- suicide ideation—14 per cent
- autism—11 per cent
- homelessness—6 per cent.
Our data showed that multiple stays, which add up to long periods of time as inpatients, are also common in child and youth mental health. When we added clients' multiple stays together, we found 394 young people over three years who had each been inpatients for a total of 35 or more days. Of these, 72 young people (2 per cent) had been inpatients for more than 100 days out of the three years.
Figure 4G
Number of admissions by total bed days for four audited health services, 2016–18
Source: VAGO analysis of information from audited health services, January 2019.
Referral practices as a system blockage
Disputes around referral practices and discharge processes in one region create delays in discharging all young people from inpatient care while their follow-up care is arranged because it is provided by a different CYMHS.
Several interrelated system issues contribute, which include disagreement between the two CYMHS over the information that needs to be provided and received as well as the processes for receiving referrals and communicating with clients, including the role of case managers. Significant demand pressures on both CYMHS across both their inpatient beds and outpatient case managers exacerbates the issues.
Inpatient stays are being extended beyond their clinical necessity while the referral and discharge processes are negotiated.
DHHS advises that it has resolved this issue as follows:
Clinical Directors have been advised to establish structured monthly liaison meetings and escalate any matters that cannot be resolved to the Chief Psychiatrist.
Health services advise that this is an ongoing issue that DHHS needs to monitor.
DHHS intervention in long or clinically unnecessary stays
DHHS has not taken strategic action in response to health services' advice about the challenges of managing 'dual disability' clients who have extended stays in inpatient units aside from the RCH project and the Alfred Health MHIDI pilot project, both of which are outlined in Section 4.5.
There is no evidence of systematic or reliable notifications of extended stays in CYMHS, and there is no mechanism for the Chief Psychiatrist to monitor and intervene in such cases in a timely manner. As an example, the Chief Psychiatrist only became aware of one of these examples more than two months into the period deemed to have been clinically unnecessary, and not via communication of the extended stay, but when reviewing another issue.
Health services have no mechanisms to effectively and efficiently escalate and resolve cases where clients no longer require mental health treatment, but cannot be re-engaged with services to support their other complex needs, such as disability supports. Where direct attempts to engage the necessary services fail, health services sometimes contact the OCP or rely on personal and professional relationships to escalate issues to more senior people in child protection or disability services within DHHS.
Each of DHHS's 17 'management areas' operates a Complex Client Panel, with membership from across DHHS program areas, local service providers, Victoria Police, hospitals, and other government departments such as DJCS. DHHS advises that the panels discuss 'a range of complex clients' and the panel members 'assist in service access, referral and support'. There is no evidence that these panels have been used to address service coordination or access issues that are causing clinically unnecessary inpatient stays in CYMHS, or that CYMHS have ever participated in these panels.
Not all complex clients 'stuck' in in-patient services will have their service needs met through local or area-based coordination. One audited health service suggested the need for a statewide version of the high-risk youth panels that some CYMHS convene to assist with service access and case planning for the most complex clients.
Multiple and Complex Needs Initiative
Currently, 14 young people aged 17–25 years with a diagnosed mental illness are receiving case management support through the MACNI program managed by DHHS, with funding contributed by DJCS. Only one of 28 referrals for young people under 25 years to the MACNI program in 2018 was from CYMHS. Figure 4H shows the referral source for younger MACNI clients.
Figure 4H
Referral sources for MACNI clients aged under 25 years in 2018
Source: VAGO analysis of information provided by DHHS.
MACNI provides up to three years of case management for people aged 16 years and over with complex needs, which include two or more of the following:
- mental illness
- substance-use issue
- intellectual impairment
- acquired brain injury.
To qualify for MACNI, people must also have exhibited dangerous behaviour, or behaviour that is likely to put themselves or another person at risk of serious harm.
Possible cases are referred to the DHHS MACNI coordinator in the client's region, and a panel of senior staff from DHHS programs and local service providers will first consider whether the person is eligible and then develop a care plan to respond to the person's needs and negotiate the services that their agency will contribute.
DHHS advised in November 2018 that it does not 'market' MACNI because despite a recent funding increase, MACNI is almost at capacity. In April 2019, DHHS advised that MACNI does have capacity to take on new clients in all areas. There is no evidence that DHHS has ever 'marketed' to or communicated with CYMHS about the MACNI service. DHHS should advise CYMHS leaders of the process for referring a client to MACNI, the criteria for clients that are eligible and update this guidance regularly, as well as directing MACNI coordinators in each area to ensure they engage with their local CYMHS.
Audited health services report that they do not engage MACNI to support care coordination for the complex clients they have 'stuck' in inpatient facilities for several reasons:
- Clients are not eligible if they are under 16 years.
- Strict eligibility criteria around mental health diagnosis can often not be met for complex young people, so they are ineligible for MACNI.
- It takes too long to be useful because its process involves 12 weeks to establish a care plan and monthly meetings of regional MACNI panels.
One audited health service reported that a young person remained an inpatient beyond clinical necessity when their forthcoming 16th birthday would make them eligible for a MACNI referral. If MACNI or a similar support with a more flexible age eligibility was available, the young person could have potentially been discharged earlier.
In the Western region, DHHS has recognised that there are young people below MACNI's eligibility age of 16 who do require a similar service, and it was trialling a High-risk Youth Panel for 12–16 year-olds during the audit that was based on the principles of MACNI. There is no evidence that the pilot will be continued, nor are there any plans for how its evaluation findings and lessons will be shared.
4.4 Service coordination around multiple and complex needs
Despite clear evidence that CYMHS clients frequently have multiple and complex service needs, and international evidence that coordination of care and systems is crucial for improving outcomes, DHHS has taken no action to direct, facilitate or enable CYMHS to participate in any form of service or care coordination with other service agencies.
DHHS data linkage work has shown that in 2014–15 the following proportions of each service's clients were also registered mental health clients:
- 42 per cent of youth justice admissions
- 19 per cent of out-of-home care clients
- 31 per cent of Child FIRST family services clients.
These findings resulted from an exploratory piece of analysis by the then-new data linkage group within DHHS, and further analysis of this data that was planned has not been completed.
The most promising evidence for improving outcomes for children and adolescents as well as adults with complex needs and serious mental health problems appears when a 'systems of care' or 'wraparound' approach is used to improve the quality and consistency of service delivery. These approaches centre on integration or coordination of the multiple services involved in these complex young people's care. The approach has been shown to reduce the severity of mental health problems and decrease functional impairment that results from mental health problems.
This 'systems of care' approach is not a discrete program or project that can be trialled on a small scale—it requires substantial system reform. For example, in one large-scale initiative in the United States with positive outcomes, single centralised authorities with responsibility for the mental health service system were established in each local area and these authorities were mandated responsibility to develop and coordinate the wide range of services in the public sector including housing, income support, job training, psychosocial rehabilitation, advocacy and general health services, alongside specialist mental health services.
Key features of the 'systems of care' models that have been implemented and evaluated with positive outcomes are:
- a family focus and involvement in care and service planning
- cultural competency for staff
- interagency involvement and partnership across multiple sectors including welfare, health, justice, education and mental health
- coordination and collaboration between professionals to avoid duplication and eliminate gaps in care
- community-based service provision within close geographic proximity to the targeted community
- accessibility in terms of physical location, scheduling and financial constraints
- care individualised to the specific needs and strengths of the child
- use of the least restrictive setting possible.
Evaluation research conducted around the development of 'systems of care' approaches for both adults and children with complex mental health problems has consistently demonstrated that government-supported strategies can effectively enhance integration of services at a system level and consequently improve outcomes for children and young people.
Local care coordination
Each health service invests significant time and resources into developing and maintaining relationships with service providers who they need to engage in service coordination, most frequently child protection, but when local relationships fail to resolve matters there is no mechanism for CYMHS to escalate matters other than alerting the Chief Psychiatrist.
All audited health services actively participate in monthly or bimonthly meetings with their local child protection services in which high-risk children are discussed and CYMHS clinicians provide advice about management of mental health problems. The purpose of these forums is both case management of high-risk clients and upskilling the child protection workforce in working with mental health problems and behavioural disorders. One health service reported it has a similar arrangement with its local disability service provider, although the others reported that engagement with disability services had ceased since DHHS-funded services had been withdrawn with the transition to the NDIS.
Two health services described a 'high-risk youth' or 'complex care' panel that they convene internally to coordinate the most complex clients and escalate to involve senior staff in the most high-risk or complex cases. One of these panels involves senior staff from external agencies such as child protection and disability to participate as relevant.
Service coordination practice in Victoria
DHHS's 2016 Mental Health Workforce Strategy identifies that skill development in care coordination and service coordination is required. This acknowledgement came 16 years after DHHS began a strong policy and program focus on service coordination for DHHS's many other program areas, as described in Figure 4I.
Figure 4I
Service coordination in Victoria
|
Since 2000, DHHS and its predecessors have had a strong policy and program of funded initiatives to enable service coordination between the many different types of services available across Victoria's health and human services system. The Victorian service coordination framework helps health service providers work together to align practices, processes and systems so:
Service coordination places consumers at the centre of service delivery. The idea is to maximise consumers' likelihood of accessing the services that they need. Service coordination also enables organisations to remain independent of each other, while cooperating to give consumers a seamless and integrated response. Resources to support service coordination practice in Victoria include:
|
Source: VAGO, from DHHS materials.
Over the past two decades, funding and programs to develop capability for service coordination throughout Victoria has been largely managed through Primary Care Partnerships (PCP). These are alliances of many different health and human services that work together to improve population-based planning and coordination of care for consumers. The work of PCPs has included negotiation and documentation of shared principles, protocols, governance arrangements, service agreement templates and other resources that provide guidance to service providers seeking to enhance interagency collaboration.
When last reviewed in 2010, less than 50 per cent of Victoria's 31 PCPs had engaged any of their local mental health services in their service coordination work. There is no evidence that DHHS has provided guidance or direction to mental health services to engage with PCPs or their service coordination initiatives, nor facilitated or enabled such engagement.
The Chief Psychiatrist's intervention
Under the Act, the Chief Psychiatrist has the responsibility 'to promote cooperation and coordination between mental health service providers and providers of other health, disability and community support services'. The Secretary of DHHS has the same responsibility under the Act, and there has never been any planning about how that responsibility would be coordinated or jointly implemented or monitored between the two.
The Chief Psychiatrist does not directly engage with the Secretary nor have any process to escalate complex matters that require a coordinated response from different program areas across DHHS. The Chief Psychiatrist role is positioned in the organisational structure four reporting lines below the Secretary. A review of the Chief Psychiatrist's role in 2016 made a recommendation on this matter which DHHS has not responded to:
|
The Public Advocate is appointed by the Governor of Victoria. Their roles and powers are outlined in the Guardianship and Administration Act 1986, which involve promoting and safeguarding the rights and interests of people with disability. The Public Advocate's 'community visitors' program involves volunteers who make scheduled but unannounced regular visits to all inpatient mental health services and draw up reports of their observations. The right to make these visits and how they will be conducted are described in the Mental Health Act 2014. |
That the Chief Psychiatrist meets formally with the Secretary twice a year to provide feedback on issues concerning the quality and safety of care in clinical mental health services. This briefing should occur independently of the director of Mental Health and the Deputy Secretary of Health Service Performance and Programs (HSPP). The Chief Psychiatrist should also have the opportunity to meet at least twice a year with the HSPP Deputy Secretary.
The Chief Psychiatrist meets regularly with the Public Advocate and has asked them to escalate issues to the Secretary on their behalf. There is a formal arrangement that the Public Advocate meets regularly with the Secretary.
Around one complex case with a young person 'stuck' in a CYMHS inpatient unit, the Chief Psychiatrist led a process that involved fortnightly meetings with other program areas in DHHS over a period of 18 months. There were no formal mechanisms that could be enacted to enable this process, and finding the right people to participate with sufficient authority caused significant delays in resolving the complex needs of this young person.
The Chief Psychiatrist meets regularly with their equivalent legislated positions in the disability services and child protection areas, but there is no evidence of outcomes achieved and no evidence of shared identification of priority issues across their sectors or for shared clients. The positions are located in separate divisions of DHHS, as shown in Figure 4J, which may be impeding their capacity to collaborate.
Figure 4J
Position of the Chief Psychiatrist and Chief Practitioners for child protection, disability services, and allied health in the DHHS organisational structure
Source: VAGO analysis of DHHS organisational structures.
There are no structures or mechanisms to guide cross-sector collaboration within DHHS, nor are there governance arrangements over complex clients who require service coordination that cannot be resolved through area-level Complex Client Panels or the small cohort that qualify for the MACNI program, both of which have limitations for CYMHS clients that were described in Section 4.3. DHHS should consider establishing a mechanism that allows CYMHS to escalate complex clients who are deteriorating due to clinically unnecessary stays to a cross-sector group of senior officials who can mobilise rapidly and make decisions about service gaps and service coordination barriers for the most complex and vulnerable clients.
4.5 Managing dual disability in CYMHS
Caring for young people with complex needs where mental health problems coexist with intellectual disabilities and/or autism and challenging behaviours creates significant challenges for CYMHS. These challenges include the use of restrictive interventions, impacts on a workforce who may lack the skills and training to work with the clinical issues these clients bring, as well as the issue of extended stays, which have previously been discussed.
RCH described this challenge for CYMHS in their response to DHHS's 10-year plan, as follows:
Difficulties such as severe challenging behaviours in adolescents with Autism Spectrum Disorder pose a major practical, physical and emotional difficulty for carers as well as lead to substantial burden on the residential care system. Across the state, clinical services through regular CAMHS/CYMHS and private practitioners is difficult or impossible to obtain. These young people represent a 'blind spot' or service gap, with high morbidity and cost.
Some young people with dual disabilities also present challenges in terms of the type of inpatient accommodation they require. The case studies that we examined included examples of young people who damaged property, had significant personal hygiene challenges, and who needed to be separated from other patients for safety reasons. In some instances, these patients had to be allocated two rooms to enable staff to clean and maintain their accommodation to a safe standard.
RCH accommodates patients with dual disability who bring very challenging behaviours in a 'pod' that would usually accommodate four patients. At the time of the audit, this pod had been almost continually occupied by just one patient at a time—four different ones—for 18 months. DHHS is aware of this issue and the impact it has on the availability of mental health inpatient services to young people who need them; however, it has not taken any meaningful action to understand or rectify the issue.
Frequency of dual disability in CYMHS
Our data analysis identified 303 CYMHS clients who had intellectual disability of different severity levels, recorded as:
- 246 (81 per cent) mild
- 50 (17 per cent) moderate
- 6 (2 per cent) severe
- 1 (0.3 per cent) profound.
Our analysis also showed that many of these clients had multiple conditions or risk factors, as follows:
- autism (41 per cent)
- anxiety disorder (33 per cent)
- congenital developmental disability (30 per cent)
- problems with social/home environment (29 per cent)
- acute psychiatric, for example schizophrenia, (29 per cent)
- other medical diagnoses requiring hospital treatment (28percent)
- depressive mood disorder (17 per cent)
- maltreatment syndromes including assault and adverse childhood (15 per cent)
- alcohol and other drug issues (12 per cent)
- conduct disorder (12 per cent)
- eating disorder (11 per cent)
- suicidal ideation (11 per cent)
- self-harm (8 per cent)
- homelessness (1 per cent).
This analysis excluded 25 per cent of clients where the health service had not recorded any diagnostic codes for that client in their database. The majority of clients whose diagnoses are unknown are outpatient or community clients because 96 per cent of inpatients had diagnostic codes recorded.
Although mental health diagnoses are not recorded for all clients, we have assumed that access to CYMHS indicates the presence of a moderate to severe mental health problem.
In order to protect their privacy, we cannot report the age breakdown for these clients, but our data analysis shows a significant peak in numbers at the five audited health services at age 16. Of 302 clients, 12 per cent were aged 16 years at 31 December 2018. Given our data shows the age at that time for clients who have accessed CYMHS at any point in the three years prior, these clients may have been aged between 14 and 16 years at the time of accessing CYMHS.
This peak at age 16 is consistent across Monash Health, RCH and Eastern Health's data, but was not seen in Austin Health or AWH's data. The number of clients with intellectual disability recorded as a diagnosis was also significantly lower at Austin Health than the other audited services, which may reflect different data entry or diagnostic processes. Further investigation is required to understand the different service responses and access arrangements for young people with dual disability.
MHIDI initiative at Alfred Health
DHHS sought expressions of interest from all CYMHS in 2016 and awarded $5.5 million over four years to Alfred Health to develop and deliver MHIDI. The project included $250 000 of establishment funds to develop resources, protocols and policies.
Other CYMHS have expressed strong interest in learning what they might be able to adapt to their own service from Alfred Health's initiative. However, DHHS has not taken action to disseminate the resources developed, outcomes or lessons learned. While the project has not been independently evaluated, an extensive report which outlines achievements and challenges, lessons learned and strategies trialled was provided by Alfred Health to DHHS in April 2018.
Alfred Health made four recommendations to DHHS about system issues for young people with dual disability, which were:
- critical need for step-up, step-down residential options such as a PARC service that can specifically cater to young people with a dual disability aged 12–18 years
- an urgent need for access to special beds/pods for 13–18 year-olds in current inpatient settings for a longer length of stay in order to conduct effective psychiatric reviews with specialised treating teams competent in dual disability
- more overnight respite options for families
- improving placement options for children who are not able to stay in the family home and better systems to support families during a process of relinquishing care, including clarifying the options where the state-funded disability services that used to be central to these cases no longer exist with the transition to NDIS.
DHHS has not responded to the recommendations or acted on them. While these recommendations involve complex system issues that will not be resolved quickly or easily, DHHS needs to act to better understand and address the needs of young people with dual disability.
RCH Dual Disability Service
RCH established a 'Dual Disability Service' in 2016, in which doctors from their developmental medicine area work together with CYMHS to assess and plan treatments for children and young people who have neurodevelopmental disorders and mental health problems, such as adolescents with autism who have severely challenging behaviours.
In their response to the 10-year plan, which DHHS became aware of during the audit, RCH advised DHHS of the high demand for this service and noted that they had collected data through its pilot phase that could assist with 'scaling up and expansion' of the model.
Our data analysis showed that RCH had 114 CYMHS clients with intellectual disability, the largest of any of the audited health services. It is possible that the existence of a dedicated service increases the recording of diagnoses, which contributes to the higher number of clients that we identified in the data analysis at RCH.
DHHS was not aware of the RCH Dual Disability Service and does not provide funding or support for it. Other CYMHS that reported challenges managing these complex clients with dual disability were also not aware of the RCH service or any lessons from it.
Since DHHS ceased to convene its quarterly 'CYMHS leaders' meetings in 2016, there have not been formal opportunities to circulate information among CYMHS, which is a missed opportunity to improve CYMHS service delivery. DHHS needs to re-establish and facilitate a network where operational and clinical leaders of CYMHS can share lessons and challenges to address CYMHS system issues.
Appendix A. Audit Act 1994 section 16—submissions and comments
We have consulted with DHHS, AWH, Austin Health, Eastern Health, Monash Health and RCH, and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report, or relevant extracts, to those agencies and asked for their submissions and comments. We also provided a copy of this report to the Department of Premier and Cabinet.
Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
- DHHS
- AWH
- Austin Health
- Eastern Health
- RCH
RESPONSE provided by the Secretary, DHHS
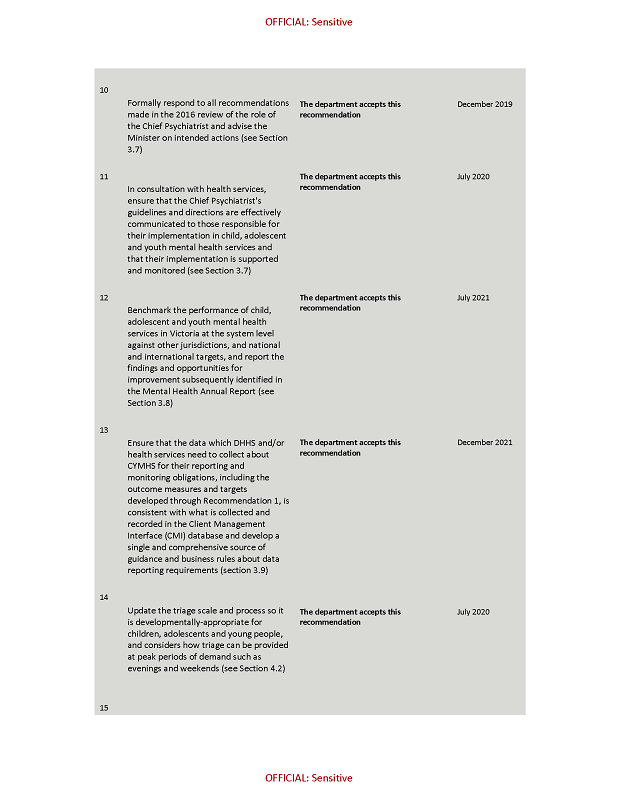
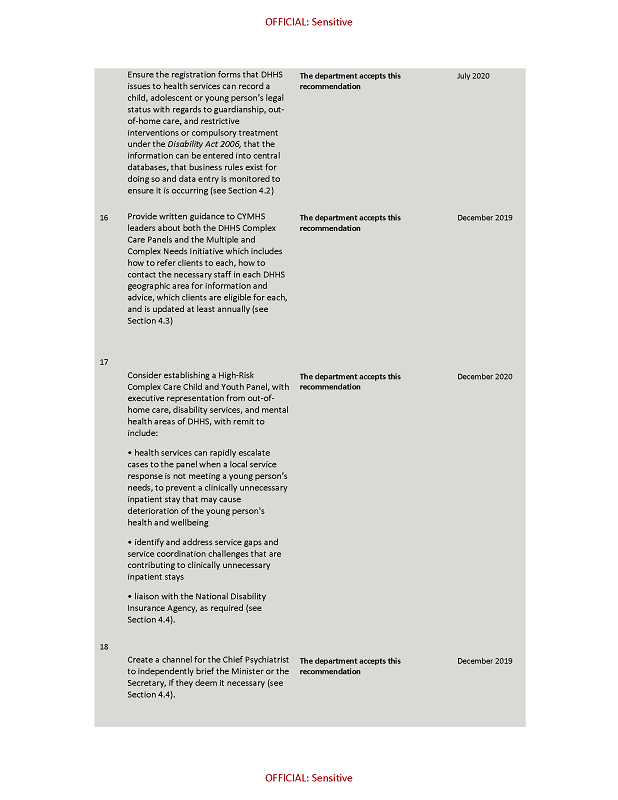

RESPONSE provided by the Chief Executive Officer, AWH
RESPONSE provided by the Acting Chief Executive Officer, Austin Health
RESPONSE provided by the Chair, Eastern Health
RESPONSE provided by the Chief Executive Officer, RCH

Appendix B. DHHS funding for child and youth mental health 2018–19
|
Health Service |
Inpatient funding ($) |
Child and adolescent treatment services ($) |
Other specialised programs ($) |
Total CYMHS ($) |
|---|---|---|---|---|
|
Monash Health |
9 267 475 |
8 972 474 |
6 489 481 |
24 729 430 |
|
Austin Health |
5 981 334 |
7 098 963 |
2 943 371 |
16 023 668 |
|
Royal Children's Hospital |
4 160 928 |
10 856 000 |
2 471 153 |
17 488 081 |
|
Eastern Health |
3 120 696 |
7 889 115 |
4 768 661 |
15 778 472 |
|
Melbourne Health |
4 160 928 |
0 |
3 535 171 |
7 696 099 |
|
Alfred Health |
0 |
4 621 759 |
3 346 207 |
7 967 966 |
|
Bendigo Health |
2 193 367 |
3 213 003 |
2 092 409 |
7 498 779 |
|
Barwon Health |
0 |
2 498 146 |
2 538 710 |
5 036 856 |
|
Latrobe Regional Hospital |
520 116 |
2 527 136 |
1 963 522 |
5 010 774 |
|
Ballarat Health |
520 116 |
2 124 821 |
1 698 458 |
4 343 395 |
|
Peninsula Health |
2 193 367 |
0 |
1 621 403 |
3 814 770 |
|
Goulburn Valley Health |
0 |
2 093 017 |
1 385 686 |
3 478 703 |
|
Albury Wodonga Health |
0 |
2 013 665 |
1 048 713 |
3 062 378 |
|
Ramsay Healthcare |
520 116 |
778 477 |
1 290 282 |
2 588 875 |
|
South West Healthcare |
0 |
1 355 596 |
941 989 |
2 297 585 |
|
St Vincent's |
0 |
0 |
712 836 |
712 836 |
|
Forensicare |
0 |
0 |
144 770 |
144 770 |
|
Total |
32 638 443 |
56 042 172 |
38 992 882 |
127 673 437 |
Source: VAGO, based on information from DHHS.
Appendix C. DHHS program descriptions
|
Program name |
Program description |
|---|---|
|
Child and Adolescent Assessment Treatment |
A range of services including crisis assessment, case management, individual or group therapy, family therapy, parent support and medication-based treatments for children and adolescents experiencing significant psychological distress or mental illness. Services support a timely response to referrals, including crises, delivered on an outreach basis, where appropriate. |
|
Conduct Disorder Program |
Services that provide prevention programs for children and young people at risk and clinical services for those with established conduct disorder. |
|
Early Psychosis Program |
Specialist treatment and improved continuity of care services for young people with an emerging disorder, particularly co-existing substance abuse problems. |
|
Intensive Youth Support |
Provision of mobile intensive mental health case management and support to adolescents who display substantial and prolonged psychological disturbance, have complex needs, which may include challenging, at-risk and suicidal behaviours, and who have been difficult to engage utilising less-intensive treatment approaches. |
|
Community Specialist Statewide Services—Eating Disorders |
A range of specialist clinical community mental health assessment, treatment or consultancy services that support eating disorder groups on a statewide, inter-regional or specific catchment area basis. The focus of these community services is on a clinical service provision to people with a mental illness. |
|
Youth Suicide Prevention |
Youth suicide prevention programs aim to reduce suicide among young people aged 10–25 years. Programs provide preventative support, activities and early intervention services to the young person, their family and friends and the broader community. |
|
Acute Care—Child and Adolescent |
Inpatient units provide short-term psychiatric assessment and treatment for children and adolescents with severe psychological disturbance who cannot be effectively assessed or treated in a less-restrictive community‑based setting. |
Source: DHHS Policy and Funding Guidelines 2018–19 Section 3.4, Chapter 3, page 226–229.
Appendix D. Clinical data analysis methodology
Our clinical data analysis in this audit involved the five audited health services, which provided to us all community contacts and admissions for all clients aged 0–25 years across three years from 1 January 2015 to 31 December 2018.
The data that we received and analysed from CMI/ODS was:
- 18 460 unique clients
- 10 demographic fields that were used in the analysis were populated for 92 per cent of clients, though this included some 'unknown' responses
- 28 191 program incidences (that is, admissions for inpatients or enrolment in a community program), which represented program-level information for 15 988 (87 per cent) clients
- ICD 10 codes for diagnoses were available for 75 per cent of clients (93 per cent inpatients, 69 per cent community)
- outcome measures—at least one was available for 61 per cent of clients, 46 per cent of clients had a HoNOSCA and 31 per cent had at least one SDQ score.
The data analysis sought to explore:
- the current client group's demographics and clinical characteristics including levels of severity and complexity
- the number of clients seen by CYMHS as a whole and each specific service within CYMHS, including emergency department presentations
- the number, length and frequency of inpatient stays
- the age and clinical characteristics of clients with longer inpatient stays.
