Maintaining the Mental Health of Child Protection Practitioners
Overview
The Department of Health and Human Services (DHHS) is responsible for protecting Victoria’s children and young people from abuse and neglect. DHHS’s child protection practitioners (CPP) receive, assess, and investigate reports of suspected child abuse and neglect—and where necessary, provide protective services to children.
Like police, emergency services and youth justice, child protection is ‘frontline’ work that is highly complex and requires specialist skills—and frontline workers are considered to be at particular risk of developing mental health issues.
DHHS has a duty of care to CPPs under the Occupational Health and Safety Act 2004 (OHS Act) and must provide, so far as is reasonably practicable, a safe work environment that is without risks to employees’ health, including psychological health.
This audit examines whether Victoria’s CPPs maintain good mental health and wellbeing. We looked at whether:
- DHHS promotes mental health and works to prevent mental illness in CPPs
- potential and existing mental health risks are identified and appropriately managed
- WorkSafe Victoria is monitoring and enforcing compliance with parts of the OHS Act relevant to mental health.
We made seven recommendations.
Transmittal letter
Ordered to be published
VICTORIAN GOVERNMENT PRINTER May 2018
PP No 392, Session 2014–18
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report Maintaining the Mental Health of Child Protection Practitioners.
Yours faithfully
Andrew Greaves
Auditor-General
10 May 2018
Acronyms
| CCYP | Commission for Children and Young People |
| CIRM | Critical Incident Response Management |
| CPP | Child protection practitioner |
| DHHS | Department of Health and Human Services |
| DINMA | Disease / injury / near miss / accident |
| EAP | Employee assistance program |
| FTE | Full-time equivalent |
| MHWC | Mental Health and Wellbeing Charter for the Victorian Public Sector |
| OHS | Occupational health and safety |
| OHS Act | Occupational Health and Safety Act 2004 |
| PAFW | Positive and Fair Workplace |
| PMS | People Matter Survey |
| TIL | Time in lieu |
| CPP Workforce Strategy | Child Protection Workforce Strategy 2017–2020 |
| VAGO | Victorian Auditor-General’s Office |
| VPS | Victorian Public Service |
Audit overview
The Department of Health and Human Services (DHHS) is responsible for protecting Victoria's children and young people from abuse and neglect. It does so through its child protection program, where child protection practitioners (CPP) receive, assess, and investigate reports of suspected child abuse and neglect. Where a child or young person needs protection, CPPs intervene and provide protective services.
Like police, emergency services and youth justice, child protection is 'frontline' work that is highly complex and requires specialist skills. CPPs are exposed to a range of mental health stressors, including:
- long and unpredictable working hours
- repeated exposure to trauma, violence, and on occasion, death
- difficult interactions with the public
- high professional expectations.
DHHS has a duty of care to CPPs under the Occupational Health and Safety Act 2004 (OHS Act) and must provide, so far as is reasonably practicable, a safe work environment that is without risks to employees' health, including psychological health.
WorkSafe Victoria is the state's occupational health and safety (OHS) regulator, responsible for monitoring and enforcing compliance with the OHS Act, among other duties.
In this audit, we examined whether CPPs are maintaining good mental health and wellbeing. In doing so, we considered how DHHS promotes good mental health, and whether DHHS identifies and appropriately manages potential and existing mental health issues. We also considered WorkSafe Victoria's role in monitoring and enforcing compliance with the OHS Act.
Conclusion
CPPs struggle to maintain good mental health in the face of unreasonable workloads and inadequate organisational support. While the mental health risks to CPPs arising from unreasonable workloads are largely beyond DHHS's control, it knows it needs to improve its organisational support for them.
DHHS's new Child Protection Workforce Strategy 2017–2020 (CPP Workforce Strategy), released in January 2018, aims to address many longstanding issues that contribute to the mental health risks that CPPs often face. However, without more CPPs to reduce workloads and meet the constantly growing demand, DHHS's actions will not be enough to alleviate the pressure on the overall system or the CPPs themselves.
Findings
The mental health and wellbeing of CPPs
DHHS has improved its focus on promoting and supporting good mental health for its staff. This includes the adoption of the Mental Health and Wellbeing Charter for the Victorian Public Sector (MHWC), the Victorian Public Service (VPS) Mental Health and Wellbeing Education and Training Framework, and its Building Positive Workplaces initiative.
However, DHHS is not meeting its obligation to ensure that CPPs are maintaining good mental health. When considered together, evidence from different sources—including records from DHHS's child protection workload management monitoring and review panels (workload review panels), survey data, staff interviews, and CPP WorkCover payments—shows that many CPPs are struggling to maintain their mental health in the face of significant barriers.
There are multiple risks affecting CPPs' mental health. While there are clear role‑based risks (those directly related to the nature of the CPP's role), it is the psychosocial risks (those resulting from their organisational environment) that pose the greater threat to CPPs' mental wellbeing. Unreasonable workloads are the primary risk to CPPs' good mental health. Multiple secondary psychosocial risks are also affecting CPPs, such as inadequate organisational support for good mental health management and a lack of professional respect from the community, other professionals, colleagues and the court environment.
Unreasonable workloads
The primary risk affecting CPPs' management of their mental health is unreasonable workloads. DHHS's assessment of the CPP workforce is that it needs to be about double its current size in order to return workloads to sustainable levels. Its most recent estimates are that about $325 million is needed annually over the next four years to address the workforce shortage.
Victoria's child protection program is widely acknowledged as 'stretched beyond its capacity'. Multiple reviews—from organisations such as the Victorian Ombudsman, the Commission for Children and Young People (CCYP), and Parliamentary inquiries, among others—all express the view that the child protection program is 'overloaded'.
Persistent underinvestment in child protection means that demand for child protection services has far exceeded the capacity of the CPP workforce. Between 2010 and 2016, the number of CPPs rose by around 26 per cent, but this has not kept pace with the:
- 121 per cent increase in child protection reports (from 48 403 in 2009 to 107 095 in 2016)
- 42 per cent increase in CPPs' average allocated case loads (from 12 in 2009 to 17 in 2016)
- increased requirements for CPPs to work on cases not assigned to them (known as unallocated cases), and thus not reflected in their work programs
- increasing administrative burdens associated with child protection activities—driven by the requirement for more comprehensive recordkeeping, increases in court‑ordered contact, and more court‑related administration tasks such as court reports, subpoenas, and coordinating specialist consultations.
Further, the inconsistent nature of funding for child protection has also limited DHHS's capacity for budget and workforce planning. Because of the lengthy nature of recruitment and development of new CPPs, and the continuously rising demand, the impact on the CPP workforce has been severe.
DHHS has a responsibility to make government fully aware of the potential liabilities of exposing CPPs to mental health issues due to unreasonable workloads. Its submissions to government have discussed the impact of resource restrictions on the delivery of protective services. However, the submissions have not sufficiently detailed the potential legal and financial implications of CPPs being exposed to unreasonable workloads.
We gained a preliminary understanding of CPPs' experiences in managing their mental health by reviewing CPPs' responses to the annual People Matter Survey (PMS), administered by the Victorian Public Sector Commission. We supplemented this by also:
- conducting our own survey of Victoria's CPPs
- interviewing more than 100 CPPs and child protection executives from various offices across the state
- visiting CPP worksites and holding focus group discussions at three metropolitan offices, two regional offices and the child protection program's central office in Melbourne.
The negative mental health impacts of unreasonable workloads were a common theme in our focus groups and interviews with CPPs, as well as in responses to our survey.
Records of the child protection program's workload review panels—established to monitor and address workload demand issues—show regular discussions of teams being unable to meet workload requirements. The records also reflect ongoing concerns with CPPs' mental health.
DHHS's OHS reporting program and its commissioned reviews, along with PMS results and CPP WorkCover payments data, support the finding that CPPs face unreasonable workloads.
CPPs' responses to the PMS reflect increasing work‑related stress levels over time. In 2013, 51 per cent of CPP respondents agreed that they did not feel too stressed at work. In 2016 however, only 33 per cent of CPP respondents reported no to low or mild stress levels. Likewise, in 2015, 58 per cent of CPP respondents agreed that they could manage their workload. In 2016, only 34 per cent agreed that their workload was appropriate for the job they do.
Over the last four years, CPPs have consistently reported high levels of dissatisfaction with work-life balance in the PMS, and 50 per cent of CPPs who responded to our survey felt that they could not reasonably manage the demands of work as well as their personal lives.
CPPs' struggle to cope with mental health risks is also reflected in WorkCover claims. DHHS data shows that in 2016–17, 49 per cent of the 37 CPP WorkCover claims related to mental health. WorkSafe Victoria's site visits to child protection offices are also primarily in response to complaints of excessive workloads.
In our interviews, CPPs repeatedly reported feeling that meeting workload requirements comes at the cost of their mental health. Pressure to meet demands around case loads, supervised contact and court-related administration impedes CPPs' efforts to maintain good mental health and wellbeing.
CPPs described how meeting these demands meant regularly working overtime. However, a fear of being seen as needing more than a 'standard working day' to complete assigned work influences their decisions to under-report their working hours. The requirement to complete heavy workloads within strict statutory time lines, coupled with the need to keep CPP teams staffed at all times, also creates competition for access to work breaks and leave.
In addition, from 2015 to 2017, records of DHHS's workload review panels repeatedly comment on the impact of the heavy workloads on CPPs, describing their high levels of fatigue and stress.
Supporting CPP mental health management
A range of secondary risks also affect CPPs' ability to manage their mental health.
Of the 190 CPPs who responded to our survey, 80 per cent either somewhat agreed or strongly agreed that DHHS provides services to support their psychological health. However, in CPP focus group discussions and interviews, a common theme was that those services, discussed below, did not adequately meet their needs.
Inconsistent or inadequate provision of mental health support
DHHS does not consistently apply its key processes for supporting mental health management. Regular, scheduled supervision between CPPs and their line manager is child protection's primary support tool. However, to meet statutory time lines, CPPs at all levels regularly de-prioritise either providing or attending supervision sessions.
DHHS actively promotes its employee assistance program (EAP). However, CPPs report that access challenges when the EAP service is offsite, and privacy concerns when it is onsite, can make CPPs reluctant to use the service. Further, while CPPs appreciate having these services available, they typically reported needing a more clinically advanced level of support.
The absence of professional respect
In discussions with CPPs and DHHS executives, we learned that an absence of appropriate respect for the child protection profession fuels frequent poor behaviour by clients and community members, in court environments, and even in child protection workplaces. Poor behaviour towards CPPs has also been a subject of concern in past Parliamentary reports.
The need for education and training on mental health and wellbeing
DHHS's OHS training has historically focused on 'traditional' health and safety areas such as manual handling, injury prevention and occupational violence risk assessment. However, its December 2016 adoption of the MHWC includes implementing an education and training framework to improve employees' capability in identifying mental illness and awareness of the support available.
As a part of this, DHHS is delivering a series of mental health and wellbeing awareness programs for staff at all levels. While the programs are not specific to the mental health of CPPs, it is reasonable to expect that CPPs will benefit from increased department-wide capability in supporting mental health.
Confusing mental health reporting processes and lack of oversight of CPP mental health
DHHS's health and safety incident reporting process does not sufficiently consider mental health and DHHS does not appropriately monitor CPPs' excessive working hours, or balance them with compensatory leave.
There are multiple avenues that CPPs can use to identify a need for mental health support. These include scheduled supervision sessions, OHS incident reporting, EAP services, workload review panels, DHHS's Critical Incident Response Management (CIRM) framework and its Positive and Fair Workplace (PAFW) policy.
While having many ways to identify mental health concerns is a positive thing, inconsistent direction about which tools they should use under which circumstances is confusing for some CPPs. Further, offices with consistently high staff turnover can struggle with retaining organisational knowledge, which can exacerbate this confusion.
In combination, these issues muddy DHHS's data on mental health, delay resolution processes and can reduce CPPs' confidence in reporting processes. Further, they prevent DHHS from having a consolidated view of CPPs' mental health concerns identified through the various reporting avenues. Consequently, it does not have an informed understanding of the current state of CPPs' mental health, the systemic risks they face, or the effectiveness of the support tools available.
Results from the PMS and our own survey show that while CPPs have confidence in their immediate line managers, this does not extend to the broader organisational environment, processes for reporting issues and concerns, or processes for ensuring staff accountability.
While WorkSafe Victoria is the state's OHS regulator, its small workforce prevents it from actively monitoring organisations. However, its 2017–18 business plan identifies social assistance services—≠which includes CPPs—as one of its top priorities.
The impact of inadequate mental health support on CPPs
The cumulative impact of primary and secondary risks to CPPs' mental health also creates downstream implications for DHHS.
The majority of CPPs' mental injury WorkCover payments from 2012 to 2016 were for work‐related harassment and/or workplace bullying.
In 2016, work‐related harassment and/or workplace bullying WorkCover payments accounted for 61 per cent of all CPP mental injury payments. The second most common type of CPP WorkCover mental injury payment was for work pressure.
From 2012–13 to 2016–17, the average tenure of child protection's core case‑carrying staff, CPP-3s (practitioners) and CPP-4s (advanced practitioners), was 2.56 years and 6.14 years respectively. This creates a need for constant recruitment and training—an avoidable financial burden for DHHS.
DHHS's reform of child protection
To address concerns about the mental health of CPPs, DHHS has committed to improve its support to CPPs. This includes the implementation of its CPP Workforce Strategy (released in January 2018), which is also underpinned by the MHWC. The strategy focuses on:
- attracting and recruiting the best people
- growing and developing staff
- engaging and retaining staff
- maintaining the wellbeing of CPPs
- building a professional identity for the workforce.
Many of the initiatives in the strategy, if implemented effectively, will help to address the secondary mental health risks that CPPs face. These initiatives include improved CPP wellbeing support programs and better processes for recruitment and retention, professional development and professional recognition.
In addition, DHHS's commitment to the MHWC is an opportunity for DHHS to gain a more sophisticated understanding of CPPs' mental health. By better managing information, DHHS should also be able to address current inadequacies in its understanding about the mental health of the CPP workforce. It should also help DHHS to better demonstrate its need for additional resources.
In 2017, DHHS received non-recurrent funding totalling $72.242 million for the child protection workforce. This funding is enabling DHHS to trial new administrative supports to help ease CPP workloads. However, as DHHS recruits new staff, the funding will transfer to staffing and these support programs will cease.
Recommendations
We recommend that the Department of Health and Human Services:
- advise government of:
- the current level of risk to the mental health of the CPP workforce due to unreasonable workload and (see Section 2.3)
- the resources required to fully address current and future demand, based on accurate time and resource modelling (see Section 2.3)
- develop and implement modelling tools to support demand forecasting (see Section 2.3)
- establish a holistic view of child protection practitioners' mental health through the use of consolidated mental health data sources; and use this view to monitor CPP mental health, and identify trends and areas requiring focus or further investigation (see Section 3.5)
- determine the effectiveness of current mental health support tools for child protection practitioners (see Section 3.5)
- establish and consistently provide specialist mental health support services for child protection practitioners (see Sections 3.2, 3.3, 3.4 and 3.5)
- ensure that child protection practitioners are sufficiently aware of the available mental health support services and the correct processes for raising mental health concerns (see Section 3.5)
- establish and implement a plan to improve CPPs' experiences in the court environment, in consultation with the courts, the Department of Justice and Regulation, and Victoria Legal Aid (see Section 2.4).
Responses to recommendations
We have consulted with DHHS and WorkSafe Victoria, and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report to those agencies and asked for their submissions or comments. We also provided a copy of the report to the Department of Premier and Cabinet.
The following is a summary of those responses. The full responses are included in Appendix A.
DHHS acknowledged the report's findings and that more is required to support the CPP workforce. It also accepted the recommendations and provided an action plan detailing how it will address them.
While the recommendations were not directed to WorkSafe, it has also acknowledged the report's findings and recommendations.
1 Audit context
1.1 Child protection in Victoria
Under Victoria's Children, Youth and Families Act 2005, DHHS is responsible for protecting children and young people from abuse and neglect. As of 30 June 2017, DHHS employed 1 933 CPPs in 24 field offices across four divisions to carry out this mandate. This includes:
- receiving reports of suspected neglect and abuse
- conducting investigations to determine the need for protective services
- intervening when a child is in need of care and protection
- taking matters before the Children's Court
- supervising children on child protection orders
- determining case plans
- providing case management services for children and young people who are either living with family or in out-of-home care
- engaging with other providers with a role in protecting children, including Child FIRST providers, schools, police, doctors, community health services and courts.
|
Child FIRST is a state government initiative that aims to connect vulnerable children, young people and their families to relevant services. |
Like emergency services workers such as police and paramedics, CPPs are exposed to mental and emotional stress due to the nature of their work. They regularly deal with traumatic incidents, substance‑affected people and violence, which may, on occasion, threaten their personal safety.
DHHS has a duty of care to ensure that CPPs maintain good mental health and wellbeing while working to protect some of Victoria's most vulnerable citizens.
CPPs
CPPs perform different functions depending on their level within the child protection system. The levels are classified from CPP-2 through to CPP-6. The CPP workforce consists broadly of support workers, CPPs and leadership positions. Figure 1A summarises the CPP classifications and roles. See Appendix B for descriptions of each role.
Figure 1A
Child protection classifications and roles
|
Classification |
Role |
|---|---|
|
CPP-2 |
Case support worker |
|
CPP-3 |
Practitioner |
|
CPP-4 |
Advanced practitioner |
|
CPP-5 |
Team manager |
|
CPP-5.1 |
Senior child protection practitioner |
|
CPP-5.2 |
Practice leader |
|
CPP-6 |
Principal practitioner |
|
CPP‑6.1 |
Deputy area manager Area manager Area manager, regional services |
|
CPP-6.2 |
Child protection operations manager |
Source: VAGO based on DHHS Child Protection Manual.
All CPPs who manage cases must have relevant qualifications, the most common being social work, welfare work and psychology. DHHS also provides ongoing training, with programs tailored to different child protection career levels.
|
DHHS's Child Protection Manual classifies child protection reports as:
|
Establishing the need for child protection services
Family support services are provided through three key systems:
- The universal (primary) service system—delivers services to Victorians, and aims to prevent abuse and neglect (antenatal, maternal and child health, and education services).
- The secondary service system—provides support through requests or referrals, and aims to reduce drivers of abuse and neglect (integrated family services, respite care, mental health and substance abuse support, and counselling services).
- The statutory (tertiary) service system—intervenes when the primary and secondary systems are unable to ensure a child or young person's safety (child protection and out‑of‑home care for children who cannot live at home).
After receiving a report, CPPs assess whether the child or young person's circumstances fall within the legal definition of 'requiring protective intervention'. If a CPP classifies a report as requiring protective intervention:
- urgent investigations must occur within 48 hours
- non‑urgent investigations must occur within 14 business days.
Phases and decision-making in child protection
Child protection is highly complex, requiring adequate time and support to make informed and effective decisions that are based on the unique circumstances and requirements of each child.
CPPs use a 'best interests' case practice model to determine the level of danger facing the child and the likelihood of future harm occurring. They use this model across the five key child protection phases—shown in Figures 1B and 1C—though the phases are not necessarily consecutive. Figure 1D illustrates how child protection cases move through the child protection program, and Appendix C illustrates the different phases in detail.
Figure 1B
Child protection phases
|
Phase |
Description |
|---|---|
|
Intake |
CPPs receive reports and determine the appropriate response, provide advice, help children and families access support services and, where appropriate, make referrals. |
|
Investigation |
CPPs assess the risk to the child and determine whether they need protection. This involves direct assessment and interviews with the child and custodial carer(s), and consultation with relevant people, including professionals, to determine whether to substantiate a report and if further protective intervention is required. |
|
Protective intervention |
Once CPPs substantiate protective concerns, they prepare a case plan for the child. Throughout protective intervention, CPPs monitor and assess the child's needs and parental capacity, and determine the types of:
Protective intervention ceases when:
|
|
Protection order |
If CPPs are unable to work effectively with the family to ensure a child's safety, they will make a protection application to the Children's Court. CPPs' primary role during this phase is ongoing engagement with the child and family to assess risks and provide for the child's safety and wellbeing. |
|
Closure |
A case can be closed from any of the above points. CPPs must:
|
Source: VAGO based on DHHS Child Protection Manual.
Figure 1C
Overview of child protection processes
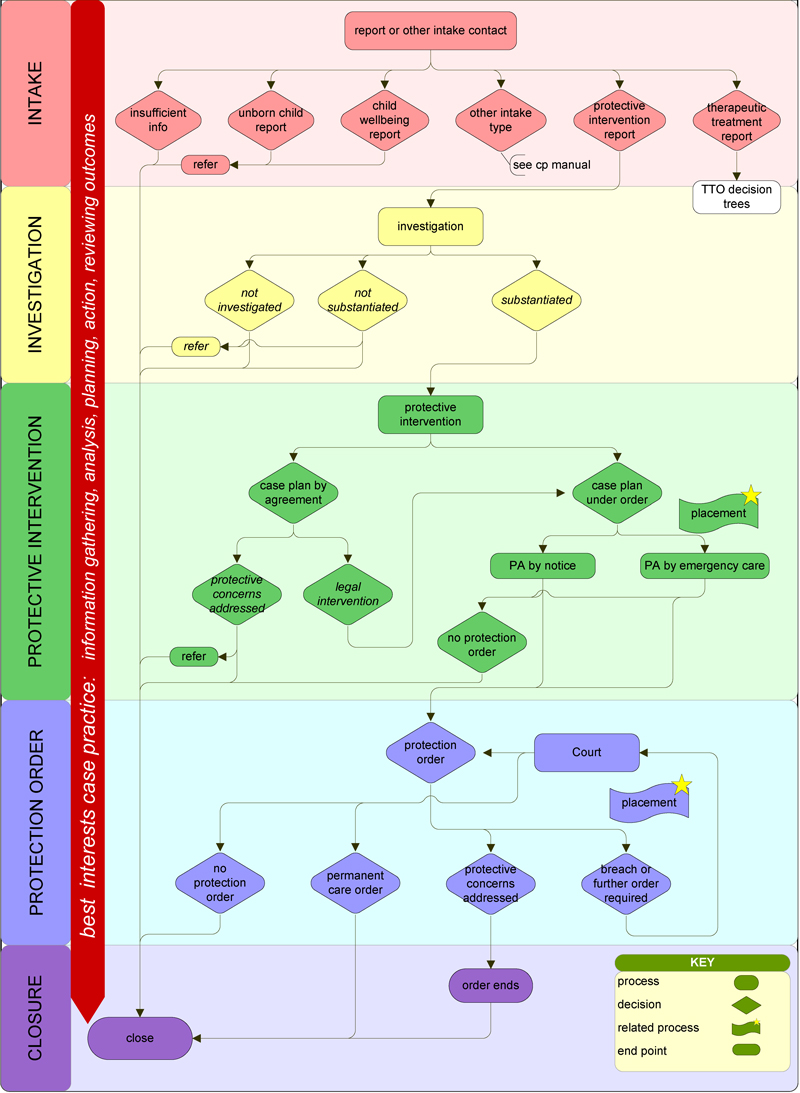
Source: DHHS Child Protection Manual.
Figure 1D
Flow of cases through the child protection program
Note: Figures correct as at 20 November 2017.
Source: DHHS, Proposed strategies to reduce and manage cases awaiting allocation (2017).
1.2 Workplace mental health
The role of good mental health in delivering public services
On a global scale, employers are increasingly recognising the role of good mental health in a productive workforce. Poor mental health directly affects productivity and turnover, as well as the achievement of organisational goals.
According to WorkSafe Victoria, mental injury is the second highest source of compensable claims in Victoria, following musculoskeletal disorders and joint or ligament injuries. Chronic stress is also linked to immune system disorders, musculoskeletal disorders and chronic pain, as well as a growing list of conditions such as gastrointestinal disorders, skin rashes, migraines and asthma.
WorkSafe Victoria recorded more than 3 100 claims for mental health disorders in 2016 (about 12 per cent of total claims), and it expects the rate of mental injury in the community to increase over the next 10 to 20 years.
At the same time, studies such as beyondblue's 2014 report Creating a mentally healthy workplace: Return on investment analysis indicate that a mentally healthy workplace, on average, may deliver benefits worth more than double the original investment. These benefits typically take the form of improved productivity resulting from reduced absenteeism and 'presenteeism' (reduced productivity while at work), and fewer compensation claims. The study suggests that this estimate is conservative, however, as it does not account for more intangible benefits such as improved morale.
The role of government in promoting good mental health
Under the OHS Act, employers are responsible for providing and maintaining a working environment that is safe and without risks to health—including psychological health—so far as is reasonably practicable. An employer's specific obligations are set out in sections 21 and 22 of the OHS Act.
Over time, the government has increased its focus on integrating mental health into workplace OHS regimes. The government endorsed the MHWC in October 2016. The MHWC commits government organisations to creating a mentally sound and safe workplace through:
- identifying, measuring and treating mental health risks through the OHS system in the same way as physical OHS risks
- leaders championing mental health and wellbeing initiatives
- developing a culture, skills and environment that empowers workers to recognise and raise mental health issues to assist themselves and colleagues
- collecting and reporting data to improve the understanding of mental health and wellbeing in the public sector and to inform continuous improvement in the programs and services offered to employees
- delivering evidence-based training programs that support the capability of managers and workers, including health and safety representatives, in identifying, preventing and addressing mental injury and illness, as well as promoting positive mental wellbeing
- consulting, communicating and providing services that support mental health and wellbeing that can be accessed and used by all employees.
In February 2017, DHHS was the first agency to roll‑out the MHWC. DHHS supports the MHWC with a Health, Safety and Wellbeing Strategy, a People Strategy and the VPS Mental Health and Wellbeing Education and Training Framework.
Mental health of CPPs
The government recently recognised CPPs as 'frontline' workers, along with police, emergency services staff and youth justice workers. Frontline workers are considered to be at particular risk of developing mental health issues. While the nature of CPPs' work may differ from other sorts of frontline work, they experience the same types of stressors as those set out below.
In examining mental health in emergency services personnel, beyondblue's 2014 report Audit of emergency services mental health programs identified several stressors in particular that contribute to poor mental health, including:
- long and unpredictable working hours
- repeated exposure to trauma, violence and death
- difficult interactions with members of the public
- high expectations pertaining to the profession.
In January 2018, DHHS released its CPP Workforce Strategy. The strategy's goal is to build, develop and sustain the capability, wellbeing and professional identity of the Victorian child protection workforce.
The strategy comprises five major priorities:
- attracting and recruiting the best people
- growing and developing staff
- engaging and retaining staff
- maintaining the wellbeing of the CPP workforce
- building a professional identity for the workforce that recognises child protection as a valued profession of the highest integrity and competence.
The fourth priority—maintaining the wellbeing of the CPP workforce—includes implementation of a child protection psychological support program.
WorkSafe Victoria's role in mental health and wellbeing
As Victoria's workplace health and safety regulator, WorkSafe Victoria's role is to ensure that employers are providing a safe and healthy workplace. It is also responsible for:
- monitoring and enforcing compliance with the OHS Act
- providing information about duties, obligations and rights under the OHS Act
- promoting public awareness and discussion of OHS and welfare.
WorkSafe Victoria also chairs Victoria's Public Sector Occupational Health and Safety Improvement Interdepartmental Committee. This committee provides a forum for government departments to share information and establish benchmarks for OHS best practice.
WorkSafe Victoria's focus on mental health and wellbeing has been growing since 2004. As part of its psychological health program, WorkSafe Victoria has produced handbooks and guidance documents on subjects such as stress and bullying. It also developed the People at Work project—a free risk assessment tool that organisations can use to identify psychosocial hazards in the workplace.
WorkSafe Victoria's 2016 Annual Report notes:
'Community expectations of our role in the complex issues of mental injury, bullying and occupational violence are also expanding, requiring us to reassess how we regulate workplace safety and how we deliver our services.'
In April 2017, WorkSafe Victoria announced the next iteration of its psychological health program, which aims to promote and protect the mental health and wellbeing of all Victorian workers.
1.3 Why this audit is important
DHHS has a duty of care to ensure that CPPs maintain good mental health and wellbeing. As CPPs are routinely exposed to environments that carry a high risk of harm to their mental health, there is an expectation that DHHS actively works to minimise or eliminate such risks. Supporting the mental health of CPPs also:
- helps to lower recruitment and training costs associated with staff turnover
- works to reduce the number of WorkCover claims related to mental health
- better enables CPPs to deliver quality services to protect vulnerable children.
1.4 What this audit examined and how
Our audit objective was to determine whether Victoria's CPPs maintain good mental health and wellbeing. In making this determination, we considered whether:
- DHHS promotes mental health and works to prevent mental illness in CPPs
- potential and existing mental health issues are identified and appropriately managed.
We also considered WorkSafe Victoria's role in monitoring and enforcing compliance with the parts of the OHS Act relevant to mental health.
Our audit did not examine the effectiveness of the child protection program.
We examined DHHS's policies and procedures for supporting good mental health, interviewed CPPs and child protection management staff, and reviewed data related to the causes and effects of poor mental health in CPPs.
Survey and interview data
The PMS is an annual survey of Victoria's public service staff. The survey asks a range of questions, addressing topics such as wellbeing, satisfaction with work‑life balance, and experiences with bullying and grievance processes. We used the CPP responses to the PMS from 2013 to 2016 to support our analyses and findings.
There are approximately 100 questions in the PMS. The exact number varies based on the respondents' demographic and individual experiences. Because all responses are voluntary, some questions may receive a higher response rate than others.
During our audit, DHHS expressed concerns about the reliability of PMS data, as some of the questions had poor response rates from CPPs. As such, we have used the results to provide a 'general sense' of CPP opinions.
We supplemented the PMS results by interviewing over 100 CPPs and executive staff in multiple locations, observing their processes and working conditions, and collecting evidence of CPPs' experiences in managing their mental health. While we visited three metropolitan offices, two regional offices and the child protection program's central office in Melbourne, we interviewed staff from many different offices, both metropolitan and regional, across Victoria.
Finally, we conducted a survey of Victoria's CPPs, to learn about their views and experiences in managing their mental health. Our survey was not a comprehensive study of CPPs' mental health, but rather a tool to establish whether views and experiences presented to us in focus groups and one‑on‑one interviews were also held more broadly.
We received 190 survey responses, which represents 9.8 per cent of Victoria's CPPs. While this is a low response level, it nevertheless contributes to the larger body of evidence that informed our findings and conclusions.
We have sought to present CPPs' perspectives by including representative responses to our survey questions and comments made during focus group sessions in the report. Further responses and comments are categorised by theme in Appendix E.
Child Protection Workforce Strategy 2017–2020
At the time of this audit, the CPP Workforce Strategy had only recently been released, it would have been premature to evaluate it during our audit. Consequently, we do not comment on the strategy outside of identifying how it intends to address the issues we have raised.
Conducting our audit
We conducted our audit in accordance with section 15 of the Audit Act 1994 and ASAE 3500 Performance Engagements. We complied with the independence and other relevant ethical requirements related to assurance engagements. The cost of this audit was $550 000.
1.5 Report structure
The remainder of the report is structured as follows:
- Part 2 examines the identified risks to CPPs' mental health
- Part 3 examines how DHHS supports CPPs in managing their mental health
- Part 4 examines the impacts of mental health risks on CPPs.
2 Risks that impact the mental health of CPPs
CPPs are regularly exposed to risks that may affect their mental health and wellbeing. At the same time, CPPs' workloads continue to increase, with the rising number of reports that CPPs are required to investigate and, where substantiated, act on.
This part examines the nature and origin of the risks that are affecting CPPs' mental health.
2.1 Conclusion
Poor management of psychosocial risks limits CPPs' ability to maintain good mental health.
DHHS's CPP Workforce Strategy, if properly implemented, will be a positive step in addressing the secondary risks to CPPs' mental health, which DHHS has historically not managed well.
Its plans to improve the child protection program's relationship with the media and raise CPPs' professional profile have the potential to increase recognition of the specialist nature of CPP activities and clarify where poor child protection outcomes are the result of capacity rather than capability.
In addition, DHHS's introduction of mechanisms to reduce CPP experiences of inappropriate conduct towards them may help to address another key barrier to maintaining good mental health.
However, DHHS's efforts to improve organisational support will not be enough unless the primary issue affecting CPP mental health—unreasonable workloads—is addressed.
2.2 Mental health risks
The mental health risks facing CPPs can be broadly categorised as:
- role-based—risks that are largely inherent in a CPPs' assigned duties
- psychosocial—risks associated with CPPs' organisational environment.
Role-based risks
Role-based risks are those that CPPs are exposed to because of the nature of their work. This includes vicarious trauma, critical incidents, sometimes hostile and, on occasion, violent treatment by a child, their family members, or others associated with the child.
DHHS acknowledges role-based risks as mental health risks and has supports in place to assist CPPs to manage their mental health when exposed to such events. In our discussions with CPPs, they frequently discussed that they felt able to cope psychologically, at least to some extent, with such risks.
Psychosocial risks
While exposure to violent, traumatic and distressing situations is likely to be a strong driver of stress for CPPs, leading experts in clinical and organisational psychology propose that contextual factors tend to have a stronger influence on staff wellbeing than role-based risks.
Academic research into the mental health and wellbeing of CPPs in Australia—such as the Australian Institute of Family Studies 2016 report Caring for our frontline child protection workers—generally identifies workplace concerns as significant stressors.
The impact of organisational factors on mental health also featured in the 2016 Victoria Police Mental Health Review. The review found that 'whilst operational incident exposure is an important contributing factor to mental health risk … all evidence suggests that organisational factors (particularly leadership style, management practices, workload and resourcing issues) are also very important'.
DHHS's comparatively more mature approach to role‐based risks (than to psychosocial risks) is also reflected in its WorkCover payments data which shows that from 2012 to 2016, there were only three WorkCover payments related to occupational violence. In contrast, there were 29 payments related to work pressure and 50 payments concerning work‐related harassment and/or workplace bullying for the same period.
CPPs consider their internal working environment—or psychosocial risks—to be the key driver of poor mental health outcomes. As such, our report focuses on the child protection program's psychosocial risk environment, which can be categorised as:
- a primary risk—unreasonable workloads
- secondary risks—resulting from inadequate organisational support for mental health management.
2.3 Primary mental health risks for CPPs
Unreasonable workloads—case loads, unallocated cases, and administrative burdens
Victoria's CPPs have faced excessive workloads for some time. The difficulties CPPs face in fulfilling their obligations due to unreasonably high workloads are reported at least as far back as 2009 in the Victorian Ombudsman's investigation into child protection. This report described CPPs as 'dedicated staff working under difficult circumstances' in a 'system struggling to meet its operational responsibilities'.
In 2016, DHHS commissioned an independent review of child protection that described it as a 'high voltage program' where:
'The combination of constant interactions with traumatised and damaged families and vulnerable children, large workloads, tight timelines and the intensity of the interface with the Children's Court differentiates it from other programs. Coupled with these factors is a workforce that has a high turnover in comparison with most other programs …'
DHHS's 2016 family support services strategy, Roadmap for Reform: Strong families, safe children, simply states 'Child protection services are overwhelmed'.
Figure 2A shows that the rate of reports per 100 CPPs increased from 4 110 in 2009–10 to 7 501 in 2016–17.
Figure 2A
Rate of reports to child protection, 2009–10 to 2016–17
Note: Figures stated as at 30 June each year.
Note: CPP numbers for 2012–13 were not available.
Note: CPP numbers for 2016–17 exclude the 453 full-time equivalent (FTE) CPPs funded through government's one‑off payment of $72.242 million.
Source: VAGO based on DHHS data.
DHHS has communicated to government that CPPs are subject to unreasonable workloads, stating in 2017:
'The Victorian Child Protection program is under significant and sustained pressure arising from growing and unprecedented demand … the workforce that supports the vulnerable children and families is not being supported itself … In today's system, demand pressures, coupled with resource and funding restraints, mean the workforce cannot always fulfil its role—resulting in responses that do not achieve the desired outcomes for clients.'
|
'Staff are exhausted and are not able to do the good work they would hope to do due to the increasing demand.' —CPP survey respondent |
DHHS argues that one of the strongest indicators of successful interventions is the relationship between the child, the immediate family and the CPP—but it takes time to gain the trust and confidence of all relevant parties in what can be an environment of high tension and active mistrust.
However, many issues—primarily driven by workload—limit the time available to CPPs for this critical activity. CPPs cannot form effective relationships with clients and their families when DHHS records show that CPPs could be managing more than 25 cases (including work on unallocated cases) at any one time. Requiring CPPs to deliver outputs that are not realistically achievable increases the risk that they forego or compress services to meet statutory time frames.
The CCYP noted in its report on the 2016 inquiry into child protection that:
'Having time to critically reflect and make thoughtful decisions is difficult with such an increasing workload … Workers need to have the time and the freedom to reflect on the cases they deal with, and on the decisions they make. They need to be able to consider relevant sources of knowledge in their decision-making, including research evidence and more intuitive forms of knowledge like the wisdom they accumulate over years in practice.'
Our discussions with CPPs and their responses to our survey and the PMS support our finding of unreasonable workloads. Many of the CPP comments from our survey respondents and from our focus groups and interviews—see Appendix E—highlight workload as a major issue. Records from the workload review panels provide further evidence of excessive CPP workloads, discussed in Part 3.
In addition, from 2012 to 2016, WorkCover payments for mental injury claims about work pressure were the second most common type of mental injury claim made by CPPs after work‐related harassment and/or workplace bullying.
The 2017 CCYP report on the implementation of the Children, Youth and Families Amendment (Permanent Care and Other Matters) Act 2014 drew the same key conclusions about excessive CPP workloads. A number of recommendations from the report were designed to address what it refers to as 'system wide challenges relating to demand management and resourcing of the child protection system'.
The report notes that these recommendations are made based on 'significant evidence that the child protection system is under such strain that it cannot support an adequate level of work with children, families and carers to ensure timely progress towards permanent outcomes'.
CPPs' unreasonable workloads are not solely the result of a high number of allocated cases—CPPs are also required to work on cases not assigned to a case manager, known as unallocated cases, as well as managing the administrative burden associated with each case. Figure 2B shows the different contributors to a CPP's workload.
Figure 2B
CPP workload
Source: VAGO.
In a 2014 review of the child protection operating model commissioned by DHHS, CPPs reported spending only around a third of their time working directly with children and families, creating an unsustainable work environment for many staff and severely limiting the time available for CPPs to work intensively and therapeutically with children, young people and families.
Case loads
Our analysis shows that reports to child protection rose by 121 per cent between 2009–10 and 2015−16, increasing from 48 403 reports to 107 095. In meeting this increased demand, average CPP allocated case loads rose by 42 per cent during this period, from an average of 12 to 17 cases.
There is no official position on what represents a reasonable CPP case load, and comparisons with benchmarks from other jurisdictions are also problematic due to differences in legislative requirements, case types, and practice models.
DHHS has historically avoided mapping the time and resource requirements of child protection activities to establish a 'formula' for child protection resourcing. This is partly due to the challenges of trying to establish a uniform approach to planning and resourcing activities that are by their nature subject to sudden and frequent changes—making them highly unpredictable.
A child's circumstances may change on any given day—which changes the complexity of the case and the risks to the child. Unpredictable events are commonplace, especially in cases where the child is exposed to family violence, substance abuse, mental illness or familial instability. Consequently, CPPs' risk assessment is continuous, case allocation decisions are highly individualised, and the type and amount of work associated with a case is not fixed. As CPPs continuously receive new reports, a case's priority can also change in relation to other cases.
|
'I have worked in Child Protection for over 10 years and must say that the climate today is the most challenging. The workload demands are simply unrealistic and the diversionary support programs have not eased our demand.' —CPP survey respondent |
Even details such as the distance between a child's out‑of‑home placement and the family home can add a significant burden to the allocated CPP's workload. This is because they must factor often time‑consuming child transport requirements into their existing work schedule.
Consequently, what constitutes a reasonable case load depends greatly on the details of each case, rather than on just the number of cases.
Nevertheless, the lack of a precise understanding of the time and resources needed for different child protection activities means:
- it is difficult to plan the best use of CPP resources
- the full impact of the increased demand on CPP workloads is unknown.
Currently, CPPs and their team leaders 'negotiate' case allocation, typically during scheduled supervision—see Section 3.3. As such, a team leader must have a clear understanding of each CPP's current workload—comprising their case load and the 'administrative burden' of each case—as well as a range of factors specific to the individual CPP. Figure 2C summarises key factors that impact CPPs' workloads.
Figure 2C
Factors impacting CPPs' workloads
|
Source: VAGO based on DHHS material.
In a 2017 funding submission, DHHS argued that child protection funding has not kept pace with demand and that the child protection program does not have adequate resources to meet further increasing demand. It stated that to meet its statutory obligations and stabilise the child protection system, it is critical to adopt a model that allocates a CPP to every child in the system.
One of the challenges in planning the best use of CPP resources is the lack of a precise understanding of how long different child protection activities take. While acknowledging the challenges in quantifying the time and resource requirements of CPP activities, not doing so means that DHHS has been unable to provide a compelling argument to government that the increased demand has resulted in unreasonable CPP workloads.
Unallocated cases
CPPs have statutory responsibilities to deliver child protection services, and many of the activities that CPPs undertake have legislative or regulatory time lines attached to them. These time lines exist for good reason—to minimise any delay in ensuring a child's safety.
However, for child protection to meet these time lines, DHHS frequently requires CPPs to perform tasks on unallocated cases. This requirement can drive CPPs to de‑prioritise their own cases in order to meet the statutory deadlines of the unallocated cases.
Our discussions with CPPs showed that in addition to their allocated cases—shown to be up to 25 cases in DHHS's reporting system—they may also be required to work on multiple unallocated cases at the same time. However, unallocated cases are not recognised as part of a CPP's assigned case load, making it an invisible additional burden.
CPPs often discussed concerns about having their performance challenged for not meeting time lines for their allocated cases when they had de-prioritised their own case load to meet the statutory deadlines of unallocated cases.
DHHS's 2017 funding submission for additional CPPs highlighted to government the impacts of unallocated cases:
'In order to manage the growing number of unallocated cases, team managers often distribute specific tasks on cases unable to be allocated (such as investigations of abuse and neglect or follow up visits to families) to already overworked child protection practitioners who have an existing and significant case load.
These practitioners rarely have the capacity to undertake the level of case [management] required to support the work required for families to effect real change in their circumstances; or to follow a case through to closure and instead, these especially vulnerable children, young people and families are moved between multiple workers. Such duplication and disruption is inefficient and ineffective, and can inhibit the development of positive relationships with workers, case progress and achievement of positive outcomes.'
From June 2011 to June 2016, the rate of unallocated cases per 100 CPPs rose from 61 to 222. The 2017 CCYP report described the number of unallocated cases as a 'major concern'.
Administrative burdens
In 2016, DHHS engaged a consultant to review the impact of supervised contact and placement‑related transport on child protection operations. The review found that DHHS's core case-carrying staff—CPP-3s (practitioners) and CPP-4s (advanced practitioners)—spend between 26 and 28 per cent of their time managing supervised contact, such as scheduling, transport and administration.
The review noted that this significantly limits their capacity to undertake core responsibilities, engage in practice-based work with children and families, and consequently, to effectively manage case loads.
Activities such as supervised contact and transporting children are an important part of effective child protection. Nevertheless, they add significantly to CPPs' workloads, reducing the time CPPs have for working directly with children, young people and their families. This is despite DHHS guidance stating 'other than the family's characteristics, the quality of the relationship you form with the family is the single most important factor contributing to successful outcomes for the child'.
DHHS has considered ways to minimise the amount of time that CPPs are diverted from their primary purpose of engaging with clients and their families. This includes changed arrangements for supervised contact visits and court‑related administration.
|
'Child protection work in rural areas requires a significant amount of travel that is not taken into consideration by upper management. In many instances, after having worked a full day, practitioners are required to transport clients up to 4 hours one way. This adds further stress to workers.' —CPP survey respondent |
Facilitating supervised contact
If the court decides to remove a child from a parent's care and place them in out-of-home care, it may also require child protection to provide the child and the family with supervised contact. There is no limit to the number of contacts that a court can order, nor the distance that a CPP might have to travel to transport a child to and from a contact visit. As a result, scheduling, organising, and facilitating supervised contacts can take substantial time away from CPPs' core role of directly engaging with children and families.
In our focus groups, participants told us of a number of instances where children were placed hours away from their home. This was particularly common in regional areas. In such cases, the time spent travelling to collect the child, transporting them to the contact destination, supervising the contact with the family, returning the child to the placement, and finally returning the car to the office could be five or more hours.
Further, for school-aged children, contact visits typically occur after school hours. This means that a CPP does not begin transporting a child until the afternoon and returns to the office late in the evening. CPPs do not work in shifts so, in such cases, a CPP's working day can extend to more than 11 hours, finishing around 8 pm or later.
DHHS commissioned a review of supervised contact in 2016. The review found that it was investing significant specialist resources into supervising contact with families and transporting children. While only around 24 per cent of allocated cases require supervised contact and transport, the review estimated that the use of specialist resources to deliver these services costs $22 665 433 annually.
DHHS incorporated these findings in its 2017 Budget bid, which sought funding for non-specialist (thus less costly) staff to manage supervised contact and transport. Because the initiative did not receive any funding, DHHS is currently using funding from unfilled CPP positions to run a trial of the program, and intends to build a business case for a future funding bid.
Court-related administrative burdens
Courts' evidentiary requirements impose a high level of administration. While necessary for the integrity of Victoria's legal system, this administration places a significant burden on CPPs. This particular burden has been the subject of past reports—the 2009 Victorian Ombudsman's investigation into child protection noted concern about the amount of resources necessary to service court requirements.
The investigation found that although only 7.3 per cent of all reports led to legal intervention being initiated (where a protection application follows an investigation), CPPs spent approximately 50 per cent of their time servicing Children's Court work and subsequent protection orders. The Ombudsman described this as 'a waste of scarce resources'.
The true impact of court work on CPPs' time is likely to be much greater again. This is because the broader definition of 'legal intervention' includes about 45 different application types, which can be made after a protection order is granted. In 2016–17, CPPs made 23 661 applications.
DHHS's 2014 review of the child protection operating model also discussed how dealing with subpoenas greatly reduced the time CPPs had available for critical engagement activities. It recommended that administrative tasks—such as evidence discovery, redacting files, and delivering documentation to registrars or court officials—could be performed by staff who do not manage cases. DHHS is trialing this approach as a pilot program.
DHHS's 2017 strategy for reducing unallocated cases describes the impact of statutory deadlines on the way CPPs prioritise their cases. The analysis underpinning the strategy found that because court requirements have statutory deadlines, CPPs tend to prioritise cases with court‑related obligations. This occurs even where cases without court requirements may actually involve greater risk of harm to a child.
While we did not confirm that this is occurring as a part of our audit conduct, we nevertheless agree that where workloads are so high that missing deadlines is often a very real possibility it does create the potential for case managers and senior staff to prioritise meeting statutory deadlines over ensuring a child's immediate safety.
In 2017, DHHS received a one-off payment of $72.242 million for child protection. DHHS is using this funding to recruit 453 FTE CPPs and to continue a small number of services. Figure 2D shows the breakdown of this funding.
Figure 2D
One-off funding for child protection, 2017–18
|
Service |
Funding received ($ million) |
|---|---|
|
Unavoidable demand |
67.024 |
|
Section 18 implementation(a) |
1.140 |
|
Specialist Intervention Unit (lapsing program)(b) |
2.488 |
|
After-hours emergency service |
1.590 |
|
Total |
72.242 |
(a) Section 18 provides for legal guardianship for Aboriginal children subject to a Children's Court protection order.
(b) The Specialist Intervention Unit carries out continuous improvement design and implementation, and provides and performs child protection duties when the child protection program is experiencing acute operational pressure.
Source: VAGO based on DHHS data.
DHHS is also using funding from any unfilled positions to trial new support programs for CPPs. However, as DHHS recruits new staff, the funding will transfer to staffing and these support programs will cease without additional funding.
While the 2017 CCYP report noted that it was pleased with the one‑off payment allocated to DHHS, it nevertheless found that funding has not kept pace with significant increases in demand, and that the child protection system is under 'substantial stress'. The report stated that even though there has been an overall increase in expenditure, the rise in reports, investigations, and substantiations has caused a reduction in recurrent expenditure on each of these activities.
The report also notes the CCYP's 'serious concerns about the capacity of the under‑resourced department to adequately act “as a good parent would” in the context of staff shortages, high numbers of children's cases without an allocated worker (particularly children on protection orders) and high case loads'.
DHHS advised that the $72.242 million that it received for child protection is an 'unprecedented' level of funding. However, we note that the purpose of the funding is to 'maintain' an approach to child protection which is recognised as unsustainable, and shown through this audit to directly impact on CPPs' mental wellbeing.
DHHS's push for reform
DHHS has been conscientious in informing government of the impacts of CPPs’ workloads, but its efforts have met with limited success. Consequently, DHHS has been unable to secure sufficient funding to reduce CPPs’ excessive workloads—the key mental health stressor identified by CPPs.
DHHS has advised government that the child protection workforce is taking on more responsibility and risk, but with less support and time to do their jobs effectively. It has explained that having to perform routine compliance and administrative tasks compromised CPPs’ capacity for key case work. It has also reported that divisional managers are struggling to manage proactively while also reviewing case plans and managing crises.
DHHS contends that if demand pressures could be stabilised, the child protection program could refocus on providing effective, specialist and culturally responsive interventions that collaborate and ensure better practice across all relevant government agencies.
|
'Child Protection cannot keep up with the demand, given this, children and their families are not receiving an appropriate service.' —CPP survey respondent |
DHHS’s most recent best estimate is that to properly support CPPs, it needs to return their average case load levels to 12. To achieve this, it must double the size of the CPP workforce, which requires around $325 million per year for the next four years.
If DHHS is unable to achieve this outcome, it is unlikely that it will be able to mitigate the primary risk to CPP mental health—excessive workloads.
DHHS has a responsibility to make government fully aware of the potential liabilities of exposing CPPs to mental health injuries due to unreasonable workloads.
DHHS has sought additional resources from government to address child protection workload issues. Its submissions to government have discussed the impact of resource restrictions on the delivery of protective services. However, DHHS has not sufficiently detailed the potential legal and financial implications of CPPs being exposed to unreasonable workloads.
DHHS’s future advice to government about child protection should detail:
- the risk to CPPs from unreasonable workloads
- the rate of CPP mental health injuries stemming from exposure to unreasonable workloads
- the time costs of the different CPP activities.
2.4 Secondary risks to CPPs' mental health
Poor professional standing and unprofessional behaviour towards CPPs
|
'The verbal abuse which emanates from clients, but more importantly the expectations and reactions from community service organisation staff, carers, schools, magistrates when we are unable to meet their expectations due to high workload. I currently only link into one particular care team meeting via phone in order to create a buffer between myself and the other participants.' —CPP survey respondent |
Working to ensure the safety and wellbeing of vulnerable children and young people and embedding change within families takes a highly specialised workforce. This workforce needs to have an expert understanding of childhood development, trauma, the dynamics of family violence, and transmission of disadvantage across generations. CPPs also need to be supported by sufficient resources to respond to demand as it arises.
To make decisions that are in a child's best interests, CPPs must hold recognised qualifications in a range of areas. Entry‑level CPPs must have at least a DHHS‑recognised Diploma of Community Services or equivalent qualification. Advanced CPPs typically have a minimum of two years of case work experience in addition to their qualifications, and senior CPPs more experience again.
Despite this, we learned through our interviews and focus group discussions with child protection staff that there is a general consensus across Victoria's child protection program that CPPs do not necessarily receive the same level of respect as other kinds of frontline workers. DHHS is aware of this, and its new CPP Workforce Strategy specifically considers the need to improve CPPs' professional standing in the community, the media and among other professions. It includes a CPP‑specific public relations strategy, to accurately convey CPPs' roles and expertise, and the true value they contribute to the Victorian community.
Child protection as the 'default' service provider
Child protection is the third of Victoria's key family support systems. The child protection program is 'activated' when services in the primary and secondary systems have been unable to ensure a child's safety. While child protection is often referred to as a 'service of last resort', someone raising concerns about a child's welfare may choose child protection as the first point of contact.
While CPPs are not responsible for coordinating other support services, they must nevertheless work in collaboration with many other family support organisations, including legal, health and community services. A 2010 DHHS study, Child protection workforce: The case for change, found that, over the course of the year, CPPs had worked with staff from 95 agencies across Victoria.
Figure 2E illustrates the interactive nature of the CPP role.
Figure 2E
Interactions between CPPs and other services
Source: VAGO.
Across the three systems, services operate under their own mandates and have their own jurisdictional powers. However, staff across all levels of the child protection program reported that the community and other family service organisations often perceive CPPs to be responsible for all family support services. As a result of this misperception, CPPs are often expected to assist with housing, disability, substance abuse support, healthcare and financial support.
DHHS's analysis found that many people and organisations contact child protection with concerns about a child's wellbeing, but a much smaller number report a child at risk of 'significant harm'. As a result, significant child protection resources are used to record and assess reports that may be more appropriately addressed by primary or secondary services. As Figure 2F shows, only around 25 to 29 per cent of reports lead to investigations.
Figure 2F
Child protection reports resulting in investigations, 2009–10 to 2016–17
Source: VAGO based on DHHS data.
While it is important that CPPs are able to work with other service providers to ensure they serve the best interests of at‑risk children, they are not authorised or resourced to coordinate and deliver the entire spectrum of family support services.
Our 2015 audit report Early Intervention Services for Vulnerable Children and Families also found that there is room to improve coordination of the government's family support systems. We found that Child FIRST had not created a visible point in the community for early intervention and connection with the full range of available services and supports.
Considering CPPs as the only available avenue for accessing family services places an unrealistic burden on the child protection workforce. It is not possible for CPPs to perform the 'wellbeing' duties of primary and secondary providers, and fulfil their own obligations at the same time. Such expectations are likely to leave CPPs feeling that they are 'set up to fail', and clients are likely to feel that they are not receiving a quality service.
The 2016 report from the Royal Commission into Family Violence also raised the need for family support services to better work together. Specifically, it reported that primary and secondary systems—such as mental health, drug and alcohol services, aged care, and the health and education systems—must play a more direct role in identifying and responding to family violence.
One of government's key commitments to addressing family violence is the establishment of support and safety hubs. These hubs will co‑locate a number of family services at an initial contact point, so staff will be better able to connect people to the most appropriate service. The hubs aim to provide a pathway for assisting vulnerable children before child protection is required.
Professional respect for CPPs
Child protection work involves decision-making that is much more than 'just common sense'. A paper developed to inform South Australia's Royal Commission into the Child Protection System stated that 'child protection work addresses the most complex social issues, where stakes are high and the work is done under intense scrutiny' and 'at times decisions need to be made quickly to ensure the safety of children'.
Occasionally, such decisions will be wrong. While these errors are sometimes very serious, they represent only a portion of CPPs' work in assessing over 100 000 reports per year. However, unbalanced or sensationalised reporting on child protection when a child comes to harm can create unfounded negative perceptions of CPPs and encourage hostility towards them.
In Section 2.3, we discussed how unreasonable workloads restrict the time CPPs have available to engage with clients and their families. A recent report describes this as a 'failure to engage children'. While inadequate engagement with clients is undoubtedly the outcome, by omitting important contextual information, the report may encourage readers to conclude that the failure is a question of capability rather than capacity.
A more sophisticated and proactive relationship with the media would improve public awareness of the positive outcomes achieved by CPPs, and the context of any negative outcomes. This could in turn help to raise the professional standing of CPPs in the community.
Hostility and abuse from families
Abuse of and violent behaviour towards CPPs is increasing. CPPs who participated in our interviews and focus groups frequently shared experiences of verbal abuse and physical assault from clients' family members, and sometimes from the clients themselves. This included instances of CPPs being assaulted and receiving death threats.
Recent reports on Victoria's child protection support this anecdotal evidence. For example, the 2016 CCYP inquiry into family violence in child deaths noted that in three of the 20 cases it examined (15 per cent), parents were aggressive or had threatened CPPs or other professionals.
When we questioned CPPs as to how they managed the psychological effects of such experiences, they most commonly responded that, unless the incident involved physical violence, they do not tend to make reports. CPPs explained that harassment such as being cursed or spat at was something that they 'just had to put with'. This suggests that abusive behaviour towards CPPs has become a normalised aspect of child protection work.
The government has recently invested in several anti‑violence campaigns on behalf of health care workers, paramedics and other ambulance staff. Despite the escalation of abusive behaviour towards CPPs, a similar campaign for CPPs does not exist.
DHHS's CPP Workforce Strategy commits to developing a 'positive and compelling' public relations strategy for child protection. DHHS intends the strategy to advocate publicly for the child protection discipline and profession.
Lack of professional respect in the courtroom
In our discussions with CPPs, they conveyed that they are regularly subject to poor behaviour from legal professionals during the course of their duties. At each of the five child protection offices we visited and at the child protection program's central office, CPPs mentioned this treatment as a significant cause of distress, describing their experiences as 'brutalising' and 'demoralising'.
|
'A relative of mine recently asked me about my job as they were interested in doing a similar role … I [also] told her about the court system and how disrespectful and, at times, disgusting this place is and how little respect is given to the role of child protection and the workers themselves from the magistrates and legal reps.' —CPP survey respondent |
When we asked CPPs whether they would report unprofessional conduct and/or abusive behaviour, they commonly responded with comments such as 'Why? It's not like anyone will do anything about it … That's just what you have to deal with'. These matter‑of-fact responses from CPPs suggests this sort of treatment—another driver of mental stress—has also been considerably normalised.
Further, while this issue was also widely recognised in discussions with child protection's executive staff, DHHS does not monitor the frequency or specific sources of distress. DHHS does not have a mechanism for recording CPPs' reports of unprofessional conduct they have experienced in the court environment. Consequently, there is no data to help DHHS analyse the origin of these mental health risks, or how best to address them.
This is not the first time that CPPs' negative experiences in court have been reported on. The Ombudsman's 2009 investigation into the child protection program identified CPPs' experiences dealing with the legal system as a prominent reason for low retention of CPPs. The 2012 report from the Protecting Victoria's Vulnerable Children Inquiry echoed this finding, noting that CPPs cited court processes as one of the greatest difficulties that they experience in their work. The inquiry found that interactions with the courts are a significant issue for the child protection workforce.
More recently, Victoria Legal Aid's 2016 consultation and options paper as part of its Child Protection Legal Aid Services Review noted high levels of distrust and disrespect between lawyers and CPPs.
|
'New CPPs are seeing CPPs being reamed in court and saying “I'm not doing that″.' —CPP focus group discussion comment |
Two magistrates that we spoke to indicated that they have, at times, been frustrated if CPPs were not fully prepared for court, as it hinders their own capacity to work efficiently. At the same time, they acknowledged that this may sometimes be the result of resource constraints. CPPs we spoke to recognised that, in such cases, the frustration was primarily directed at DHHS more broadly—but understanding this did not reduce the very personal impact of being publicly criticised for systemic issues beyond their control.
DHHS's CPP Workforce Strategy intends to give potential applicants and new staff more information about CPPs' interactions with the courts. It also intends to develop and deliver training on the best approach for successful courtroom engagements.
Inappropriate conduct in the workplace
|
Under the Equal Opportunity Act 2010, employers can be held responsible for instances of:
|
Victoria's Equal Opportunity Act 2010 requires employers to eliminate workplace discrimination, sexual harassment and victimisation. It also imposes vicarious liability. Unless an employer can demonstrate that it has taken reasonable preventative precautions, it may be responsible should these things occur in the workplace or in connection with a person's employment.
While our survey did not seek specific information about whether CPPs had witnessed or experienced bullying, PMS results show that CPPs increasingly see workplace bullying as an issue. In 2013, 73 per cent of CPP respondents agreed or strongly agreed with the statement 'Bullying is not tolerated in my organisation'. However, by 2016, this figure had dropped to 52 per cent. Figure 2G shows the percentage of CPP respondents who had personally experienced bullying from 2013 to 2016, according to the PMS.
Figure 2G
PMS results, 2013 to 2016: 'I have personally experienced bullying in the last 12 months'
Note: Totals may vary due to rounding.
Source: CPP responses to the PMS.
While the proportion of CPPs reporting having experienced bullying in the workplace has been stable, the fact that it is as high as 29 per cent is of concern. Further, the 2016 PMS results—as shown in Figures 2H and 2I—noted that less than 45 per cent of CPP respondents were confident that:
- if they lodged a grievance, it would be investigated in a thorough and objective manner (43 per cent)
- they would be protected from reprisal for reporting improper conduct (42per cent.
Figure 2H
PMS results, 2013 to 2016: 'I am confident that if I lodge a grievance in my organisation, it would be investigated in a thorough and objective manner'
Note: Totals may vary due to rounding.
Note: Response 'neither agree nor disagree' was introduced in 2016.
Source: CPP responses to the PMS.
Figure 2I
PMS results, 2013 to 2016: 'I am confident that I would be protected from reprisal for reporting improper conduct'
Note: Totals may vary due to rounding.
Note: Response 'don't know' was used from 2013 to 2015, and replaced with 'neither agree nor disagree' in 2016.
Source: CPP responses to the PMS.
Our own survey provided additional insight into CPPs' lack of confidence in DHHS's grievance processes—48 per cent of respondents disagreed somewhat or strongly with the statement 'People in my organisation are held accountable for their actions'.
The low levels of confidence go some way to explaining why the 2016 PMS results also shows that:
- 75 per cent of CPPs who had experienced bullying in the previous 12months chose not to lodge a formal complaint, as shown in Figure 2J
- 66 per cent of CPPs who had lodged a formal complaint were not satisfied with the way it was handled, as shown in Figure 2K.
Figure 2J
PMS results, 2013 to 2016: 'I have personally experienced bullying and lodged a formal complaint'
Source: CPP responses to the PMS.
Figure 2K
PMS results, 2016: 'I am satisfied with the way the formal complaint was handled'
Note: This question was first introduced in 2016.
Source: CPP responses to the PMS.
Following our 2016 audit on bullying and harassment in the health sector, DHHS commenced work on an initiative to 'build positive workplaces'. The initiative includes three phases:
- build the confidence and capability of managers to create a positive workplace
- check-in on staff wellbeing
- create team-based development programs.
This initiative is also underpinned by DHHS's People Strategy, which includes a commitment to prioritising health, safety and wellbeing, and a culture of 'safety always'.
The Secretary of DHHS spoke out against inappropriate workplace behaviours more generally in an address to all staff in May 2017:
'We are responding to what you've told us through the People Matter Survey about what we need to do better—such as providing a supportive workplace where bullying and inappropriate behaviour is simply not tolerated.'
While DHHS's work is aimed at the department as a whole, the CPP workforce will also benefit from the focus on a more respectful and engaging workplace.
Further, the CPP Workforce Strategy commits child protection leaders to being more responsive to employee issues and support needs, and to help drive a culture of safety and wellbeing.
3 Supporting CPP's to manage their mental health
A 2014 study on the impact of mental health conditions by Australia's Mentally Healthy Workplace Alliance advises that:
'A critical starting point [for improving staff mental health] for organisations is ensuring that policies are developed and implemented which support employees to identify that they have a mental health condition, and access appropriate treatment and support.'
In addition, centralised monitoring and reporting on mental health—particularly for staff whose roles include multiple potential drivers of mental illness—provides valuable data. It enables senior management to identify emerging mental illness trends, analyse their root causes and recommend effective interventions and supports. It also demonstrates a commitment at a senior level to supporting staff to manage their mental health—a central component of psychosocial risk management.
During this audit, 80 per cent of CPPs who responded to our survey agreed that DHHS provides services to support their psychological health. However, in CPP focus group discussions and interviews, a common theme was that those services did not adequately meet their needs. In this part, we discuss the effectiveness of DHHS's mechanisms for identifying CPPs at risk of poor mental health, and supporting them to manage those risks.
3.1 Conclusion
DHHS needs to strengthen its approach to supporting CPPs to manage their mental health. Poorly designed support tools, inconsistent guidance and provision of support, and disincentives to accessing available services all reduce the effectiveness of the support programs that DHHS has in place.
The existence of multiple avenues for raising mental health concerns or seeking support is a positive approach and reflects DHHS's desire to give CPPs every opportunity to do so. However, the absence of a mechanism to bring together the data from the disparate sources prevents DHHS from achieving a full understanding of CPPs' mental health and support needs.
3.2 Mental health education and training
For early intervention to work successfully, it is essential that managers at all levels are trained to recognise early warning signs and have the skills to respond appropriately.
DHHS does not have CPP‑specific programs that focus on managing mental health. CPP training has historically been more focused on 'traditional' areas of health and wellbeing, such as occupational violence. However, as part of its implementation of the MHWC, DHHS must ensure all staff are trained and can understand:
- what mental illness is
- how to support their own mental health and wellbeing along with that of those around them.
To meet these commitments, DHHS is implementing the VPS Mental Health and Wellbeing Education and Training Framework. The training programs in the framework are shown in Figure 3A.
Figure 3A
Training programs under the VPS Mental Health and Wellbeing Education and Training Framework
|
Audience |
Training |
|---|---|
|
All staff |
|
|
Managers and supervisors |
|
|
Executive staff |
|
Source: Adapted from the VPS Mental Health and Wellbeing Education and Training Framework.
DHHS's targets are to have this training completed by:
- a minimum of 80 per cent of executives, HR staff, managers and supervisors by 2018
- 100 per cent of executives, HR staff, managers and supervisors by 2019
- 100 per cent of staff by July 2020.
DHHS plans to run refresher training every three years. It also delivered a pilot of the framework's all‑staff awareness component to managers and supervisors in February 2018.
Mental health and wellbeing in CPP training programs
DHHS's 'Beginning Practice' is an in‑house training course that focuses on equipping new CPPs with the skills and knowledge to be effective in their role. Staff joining DHHS as CPP-3s complete the course before being allocated cases. 'Beginning Practice' includes some information and training on mental health self‑care, including vicarious trauma.
Staff in the 'Beginning Practice' team determine training requirements for CPPs, and schedule and deliver the course centrally. Team managers monitor attendance.
The 'Supervision and Leadership Program' is a learning program for new CPP-5s. The program covers topics such as mental health self-care and promotes the use of emotional intelligence in managing staff OHS issues.
DHHS has also offered several types of non‑mandatory mental health courses to CPPs, covering resilience, self-care and vicarious trauma. In addition, divisions offer staff non-compulsory training based on their assessment of their staff's training needs. This means that access to voluntary training programs may vary across divisions.
Eighty-four per cent of respondents to our survey agreed somewhat or strongly that their manager encourages and supports their participation in learning and development opportunities. Nevertheless, uptake of DHHS's courses has been limited. In our discussions, CPPs indicated that this is primarily due to workload pressures and resource constraints that make spending time away from core duties challenging.
The CPP Workforce Strategy includes a new CPP capability framework and refreshed learning and development programs. The strategy also includes activities to improve workforce and workload planning and aims to increase opportunities for CPPs to attend more training.
3.3 Supervision
Supervision—the key tool for monitoring risks to CPPs' mental health
The child protection program requires CPPs to participate in supervision. This is where CPPs meet regularly with a more senior practitioner to discuss their workload and receive professional support. Case management advice is also a component of supervision.
Child protection guidance recognises supervision as 'a key element of staff satisfaction and therefore critical to a stable workforce'. The guidance also states that 'regular scheduled supervision is the most appropriate way to ensure … optimal and safe workloads for individual staff members'.
The mandatory components of supervision include:
- supervision tools such as formal guidance and record templates, to ensure CPPs and their managers consider all variables that will help to develop or maintain a safe and sustainable workload
- discussion of the support or training needs that may impact a CPP's capacity.
Divisions report compliance with supervision requirements centrally. Figure 3B shows CPPs' compliance with supervision requirements, across DHHS's four divisions. For information on the types and regularity of supervision required for each CPP level, see Appendix D.
Figure 3B
Compliance with CPP supervision requirements, June 2015 to March 2017
Source: VAGO based on DHHS data.
|
'I haven't had any professional supervision in the last 12 months—not a single 1–1 meeting with a supervisor as per the CPP practice manual. I know that managers report on this to head office—so what is being reported?' —CPP survey respondent |
Structured supervision is the primary mechanism for monitoring CPPs' mental health. However, both CPPs and their managers spoke openly about supervision frequently not taking place as required, or the time being used solely for case direction—primarily due to workload issues. Records from the child protection workload review panels also reflect a lack of supervision—see Section 3.4—which, in some cases, show that teams were without supervision for several months.
Despite the high reported levels of compliance with supervision requirements, evidence shows that it is not occurring. This strongly suggests that DHHS's senior management lacks sufficient visibility of CPPs' ongoing mental health. It also suggests that, as a consequence, the risks to CPPs' mental health are not being properly identified and managed.
3.4 'Downtime'
Leave, 'flex', and time-in-lieu
The importance of balancing effort and recovery in the workplace is well understood. Recovery time allows for rest, exercise, nutrition and interaction with loved ones, which are important for managing stress and maintaining resilience. This is why employees' workplace agreements generally provide for regular breaks, leave entitlements and access to compensatory programs for excess working hours such as time in lieu (TIL).
The model for preventing and managing work-related psychological injury used by Comcare, the Commonwealth Government's OHS regulator, notes that 'even a workgroup with high morale is unlikely to continue to be able to cope with high work demands indefinitely without adequate recovery time'.
Workload review panels
Each CPP division has a workload review panel made up of CPPs and managers. Panels are autonomous, so they can operate in different ways, but they are required to meet at least monthly to:
- support ongoing management of CPPs' workloads
- provide an avenue for CPPs to escalate a request for a review of their workload.
Our review of panel records found regular discussion of CPPs being overloaded with work. Comments included:
- 'concerned for staff regarding work/life balance'
- 'staff are feeling stressed due to high case loads—affecting wellbeing'
- 'getting smashed'
- 'any day you survive is a good day'.
The frequency of comments such as these indicate that, while the panels do attempt to manage CPPs' workloads, there is an implied acknowledgment that little can be done.
Our review of minutes from panel meetings found insufficient evidence that the meetings were effectively escalating workload concerns. In many cases, minutes of panel meetings reiterated the severity of excessive workloads month after month, while noting that CPPs continue to 'do their best' under immense pressure.
While the panel meetings are appropriately operational by nature, the child protection program as a whole would benefit from a centralised and strategic approach to analysing workload data and recommending approaches to alleviate the burden on CPPs.
DHHS's CPP Workforce Strategy notes that 'a key component in providing our workforce with improved wellbeing outcomes is through reducing the need for staff to work overtime'. However, because DHHS does not capture TIL data for CPPs at a program level, it could not provide us with consolidated data for CPPs' TIL accrual and usage. Instead, senior managers keep TIL records on behalf of their individual teams.
Without program‑level information about CPPs' excessive work hours, DHHS cannot determine trends in CPPs' TIL. Further, it cannot be sure that its improvement initiatives are addressing the root causes of CPPs accumulating TIL.
DHHS's implementation plan for the CPP Workforce Strategy includes an analysis of CPPs' TIL and overtime. The analysis is intended to help DHHS better understand the specific situations that cause workloads to reach levels that pose risks to CPPs' metal health.
DHHS will also review the workload review panel model to consider how it might better support CPPs to manage their workloads.
Under-reporting excessive working hours
Records from workload review panels indicate that, while there are some areas where excessive workload does not appear to be a concern, in the majority of cases, it is the standard operating environment.
|
'The Department is severely under staffed and as a consequence since the introduction of the New Child Protection Model workers now work longer hours with many working and not claiming this.' —CPP survey respondent |
Despite having to work excessive hours, many CPPs told us that they regularly under-reported any additional hours they worked, or did not report them at all. When we questioned them about this practice, CPPs commonly expressed concern that management would implement performance management processes rather than acknowledge their heavy workload.
One CPP manager described repeated pressure to implement performance management whenever a CPP missed a statutory deadline. The manager would commonly—but unsuccessfully—argue that the missed deadline was due to unreasonable workload rather than underperformance.
Similar statements appear in CPPs' responses to our survey—see Appendix E—and Section 3.5 discusses suggestions of performance management in response to CPPs raising issues of 'day‑to‑day pressures' such as their workload.
Ability to use leave
To understand CPPs' experiences in accessing work breaks, we asked CPPs in our survey to state their level of agreement or disagreement with the statement 'My organisation supports me taking my entitled work breaks'.
Figure 3C shows that while 67 per cent of respondents somewhat or strongly agreed with the statement, 33 per cent of respondents somewhat or strongly disagreed.
Figure 3C
CPP survey results, 2017: 'My organisation supports me taking my entitled breaks'
Source: VAGO CPP survey.
The most common reasons for CPPs not feeling supported to take entitled breaks included competition for leave, the risk of falling further behind with work, and a culture of delivering at any cost.
'Competition' for leave
CPPs repeatedly discussed an established practice of only one CPP from each team being permitted to take leave at any time. CPPs advised that they were acutely aware of the impact that taking leave of any kind, including sick leave, has on an already overburdened workforce, particularly when teams were understaffed. They nevertheless felt that this practice unfairly set them up 'in competition' with their colleagues.
When taking time means making up for lost time
Some CPPs reported being reluctant to use accrued TIL. These CPPs explained that doing so frequently resulted in them 'only falling further behind' with their work.
Delivery at any cost
CPPs also conveyed that, in cases where they felt unable to attend work due to fatigue, they would typically report the absence as a physical illness or injury instead. CPPs believed that their workplace had a 'deliver at any cost' approach, and taking time off for anything 'non-physical' would result in them being stigmatised, labelled as underperforming, or told that perhaps the job was not for them.
3.5 Reporting mental health concerns
Speaking up about mental illness
DHHS has a number of avenues through which CPPs can raise concerns about their mental health, or the mental health of their colleagues. Figure 3D illustrates these avenues.
Figure 3D
Avenues for CPPs to raise mental health concerns
Source: VAGO.
Employee assistance program
The EAP provides employees with access to short‑term, confidential, professional counselling.
Many CPPs stated that while they appreciate the service being available, they have not found it to be especially helpful. The key reason for this was that EAP providers lacked in‑depth knowledge of the child protection program and tended to provide high‑level advice only.
EAPs may be helpful for staff not in frontline roles, but CPPs' mental health management needs are significantly more complex. CPPs working in open-plan areas also expressed concern about maintaining privacy when making or attending EAP appointments.
Our focus groups in regional areas were particularly critical of the EAP. CPPs reported significant difficulties in accessing the EAP, often having to wait a number of weeks before receiving an appointment. Some areas are trialling dedicated onsite EAP services. In these areas, CPPs spoke more favourably of the program and their ability to access its services, albeit with the same privacy concerns. In addition, shorter waiting times for appointments in these areas meant that the mental health assistance that CPPs received was more timely and thus more effective.
Acknowledging the more complex mental health needs of frontline workers, a 2016 review of Victoria Police's approach to mental health discussed the need for a statewide specialist mental health network of psychiatrists and clinical psychologists. These specialists would be experienced in treating emergency services workers and accessed on an outpatient basis. This type of support would benefit the child protection workforce.
DHHS advised that it intends to incorporate clinical relevance and availability requirements into its upcoming tender for EAP support services. In addition, the CPP Workforce Strategy includes a psychological support program designed to:
- reduce psychological risks associated with child protection work
- reduce the stigma of mental health and facilitate CPPs seeking early support and access to appropriate care.
Disease / injury / near miss / accident process
DHHS uses a standardised reporting process to record OHS incidents known as disease / injury / near miss / accident (DINMA) reporting. Staff record incidents in a DINMA book for management review and actioning. However, the approach is primarily geared towards recording physical injuries, with little to no prompting for mental health information.
CPPs discussed the inadequacy of the DINMA proforma as a key reason for not reporting mental health incidents. An additional reason was that CPPs considered that very little was done to address OHS incidents when they related to mental health.
Records from workload review panels support this opinion, frequently noting issues with the DINMA process. Issues ranged from the DINMA book being 'missing for some time', incidents not being addressed, and even references to CPPs not completing the DINMA proforma because of workload issues.
The way the DINMA process categorises stressors makes root-cause and trend analysis challenging. In 2016–17, CPPs made 142 stress‑related DINMA reports. Figure 3E shows that work pressure is the most common stress trigger reported, followed by 'other mental stress factors'. However, our analysis of the 'other' category found that it included incidents for which categories already existed—for example, workload and work‑related stress were reported as 'other' instead of as 'work pressure'.
Some DINMA categories also overlap with other DHHS processes, including its PAFW policy and CIRM framework.
Figure 3E
Stress‑related DINMA reports, 2016–17
Note: Data from 1 July 2016 until 31 March 2017.
Source: VAGO based on DHHS data.
The lack of a strategic and systematic approach for managing DINMA reporting has impeded DHHS's analysis of OHS issues. DHHS recognises that its approach needs improvement, so it is redesigning the DINMA proforma to better document mental health injuries. It is also implementing an electronic DINMA reporting process.
A staged rollout of the electronic DINMA reporting system commenced in March 2018. DHHS intends this system to:
- provide real-time incident reporting
- improve the process's transparency by notifying the employee's manager via an email workflow
- require managers to plan corrective actions with emphasis on implementing and enforcing appropriate risk controls.
This new approach is also likely to help DHHS identify trends and root causes in all OHS matters, in addition to mental health.
Critical Incident Response Management framework
Another DHHS mental health support service is DHHS's CIRM framework. The framework is a contracted service for employees in personal distress due to having experienced critical incidents at work. DHHS defines critical incidents as 'sudden, unexpected and unusual', including:
- serious injury or death of an employee or client
- incidents involving serious physical or psychological threat or sudden loss
- situations that attract significant media attention
- a series of distressing events in a short period of time
- situations involving conflict or interpersonal stress.
Other eligibility criteria for the framework include—somewhat inconsistently—prolonged stress or unusual and overwhelming demands, and extraordinary and prolonged energy expenditure. CIRM guidance also states that, in cases where the distress stems from day‑to‑day pressures, it may be more appropriate to introduce performance management, supervision, professional development or the EAP.
Suggesting performance management as a response to staff distress may explain to some extent CPPs' concerns that it is an automatic response to them seeking mental health support. DHHS advised that it does not support such an approach, and that the use of 'performance management' in this guidance was intended to mean the recommendation of performance development planning.
DHHS funds a number of providers to deliver CIRM services, but only one provider is required to report on the use of its services. As such, the true uptake of CIRM services is unknown. Figure 3F shows that CPPs were the second largest group accessing the provider's CIRM services in 2015–16. This indicates that CPPs may also be large users of the services offered by other CIRM providers.
Only 11 of the 248 users of the reporting CIRM services provider in 2015–16 (4.4 per cent) provided an evaluation of the service. Because of this and because other providers do not report on usage, we were unable to draw conclusions about the service provision.
The CIRM provider collects information about users such as their location, role and reasons for requesting services. However, its reporting to DHHS is general in nature, focusing on service provision location, type and timeliness. While this information helps DHHS to evaluate service efficiency and response speed, more detailed information about the various mental health risks facing different DHHS roles would help it to conduct more in‑depth analyses.
DHHS is reviewing the CIRM service, to identify ways to improve service provision and how it captures and reports data about staff using the service.
Figure 3F
DHHS groups' use of CIRM services, 2015–16
Source: VAGO based on DHHS data.
Positive and Fair Workplaces policy
DHHS rolled out its PAFW policy in 2010. Under the policy, DHHS defines a positive workplace as one that is rewarding, enjoyable, healthy and productive for all employees, where:
- expectations are clear
- employees are safe and treated fairly
- employees' contributions are valued and recognised
- employees are able to work harmoniously with others
- bullying, discrimination or harassment is addressed in a timely and sensitive manner.
If staff believe they have been subject to behaviour or actions that breach the PAFW policy but local intervention has been unsuccessful, they can register their concerns through a formal review process.
We reviewed the 12 PAFW requests lodged by CPPs from 2013−14 to 2017−18. Half of the requests concerned inappropriate behaviour by line managers towards staff. The other half related to allegations of bullying by management (three incidents), by a team manager (one incident), by a line manager (one incident) and by a team member (one incident).
The impact of corporate knowledge gaps on CPP mental health support
DHHS provides many ways for CPPs to identify a need for mental health support or raise concerns about a colleague's support needs. This means that, without appropriate training, new staff and those unfamiliar with the different channels may not fully understand when each should be used.
When visiting different offices, we observed that CPPs were not always aware of the different purpose of each process—for example, staff may use a DINMA proforma instead of PAFW request to report bullying concerns. Similarly, staff might use informal channels to raise workload issues, rather than the workload review panel or CIRM service.
This was particularly evident in one office that had experienced multiple staff changes and shortages over the last five years. Ongoing retention issues had resulted in a significant loss of corporate knowledge. Many CPPs that we interviewed advised that not only were they not aware of the different avenues available to them, they were also not aware of which staff might be able to advise them.
This issue highlights the importance of continuously communicating how staff can access the different support services. One regional office that has experienced years of workforce instability created a poster to help staff navigate the range of services—see Figure 3G.
Figure 3G
Workplace systems awareness poster
Source: DHHS.
Agencies' capacity for trend and root-cause analysis
DHHS's use of different and sometimes general terms to classify mental health stressors—discussed earlier—makes it challenging to analyse the data about CPPs' mental health.
WorkSafe Victoria also recognises that it is challenging to analyse the origins of mental stress claims. Its Psychological Health Program's delivery approach paper discusses weaknesses in the current approach to classifying mental injury claims. Specifically, it does not allow for the identification of an 'injury mechanism'—that is, the origin or cause of the mental stress. This makes it difficult to determine the factors causing mental injuries, and thus better tailor prevention approaches.
WorkSafe Victoria is updating its coding system to address this weakness. The update is intended to better identify and classify mental injuries stemming from psychological hazards. WorkSafe Victoria anticipates that this work will help it identify opportunities for tailored prevention interventions.
DHHS does not currently have a process that brings together all the different data sources about CPPs' mental health. Such a process would provide a rich source of information to inform policies and initiatives to improve the management of CPPs' mental health.
DHHS's commitment to the MHWC includes the development of a mental health and wellbeing minimum dataset. This dataset intends to provide a consistent method for assessing and benchmarking psychological health and safety performance across government departments.
Developing this dataset should help DHHS to address its current lack of information about CPPs' mental health. It should also help DHHS to continue improving the support it provides to CPPs.
4 Mental health and wellbeing of CPPs
CPPs work in a stressful environment and face constant demands—in both their workloads and the type of work they do. A 2008 report, The Cost of Workplace Stress in Australia, found people are more likely to experience high stress levels at work when they are under pressure—for workload or responsibility—and feel unable to meet their deadlines or control their output.
CPPs' heavy case loads are a significant challenge. Unlike other forms of social work, Victoria's child protection program must action all reports and cannot refer clients elsewhere when considered to be 'at full capacity', regardless of the resulting workload. Increasing legal and administrative [1] case requirements such as court-ordered contact mean that case load burdens have also risen. In addition, longstanding staff retention challenges add to the pressure on existing CPPs to carry the increased burdens.
This part of the report discusses the impacts of these pressures on CPPs' mental health and wellbeing.
4.1 Conclusion
The combination of multiple mental health stressors has resulted in a working environment that puts CPPs' mental health at risk. The child protection program's team unity and collegial support is particularly strong. However, it cannot compensate for the many barriers to their ability to maintain good mental health. Currently, CPPs face a lack of organisational support for mental health management, rising stress levels, persistent high turnover and inadequate work-life balance caused by unrealistic work demands. Their good mental health is also threatened by hostility and inappropriate behaviour toward CPPs and a lack of confidence in management. Evidence shows these stressors are a key cause of ongoing staff turnover and WorkCover mental injury payments.
4.2 Impacts on CPPs' mental health
The PMS measures staff wellbeing though questions about stress levels, work-life balance, bullying, and confidence in grievance processes. Paired with our survey results, we found that CPPs face a concerning number of triggers for poor mental health.
In the 2013 PMS, in response to the statement 'Generally I do not feel too stressed at work', 51 per cent of CPP respondents agreed or strongly agreed, as shown in Figure 4A.
Figure 4A
PMS results, 2013: 'Generally I do not feel too stressed at work'
Source: CPP responses to the PMS.
However, in response to the 2016 PMS question about work-related stress levels, 67 per cent of CPPs reported experiencing moderate to severe work-related stress—see Figure 4B.
Figure 4B
PMS results, 2016: 'How would you rate your current, overall stress level in relation to work-related stress?'
Source: CPP responses to the PMS.
Perceptions of support—management versus leadership
Comcare considers that staff perceptions of a workplace's leadership practices and decision-making processes are a core influence on their mental health. As such, it is critical that agency heads and leadership teams are committed to addressing work-related stress risks. Without management's support, individual support actions are unlikely to improve workplace culture and mental health.
|
'Meeting deadlines is more important than staff wellbeing.' —CPP survey respondent |
The collegial nature of the child protection environment is exceptional—in their survey responses and their conversations with us, CPPs continuously conveyed their appreciation and respect for their team members and managers. Almost without exception, CPPs described team managers as 'doing it just as tough' as CPPs themselves. Overwhelmingly they felt that teammates were their primary and most effective source of mental health support.
However, our survey results indicate that CPPs do not have the same level of confidence in their broader organisational environment. In response to the statement 'My immediate supervisor cares about my emotional wellbeing', 81 per cent of respondents agreed somewhat or strongly—see Figure 4C.
Figure 4C
CPP survey results, 2017: 'My immediate supervisor cares about my emotional wellbeing'
Source: VAGO CPP survey.
In response to the statement 'My organisation cares about my emotional wellbeing', the proportion of CPPs who agreed and strongly agreed dropped to 58 per cent, and the proportion of respondents who disagreed or strongly disagreed increased to 42 per cent—see Figure 4D.
Figure 4D
CPP survey results, 2017: 'My organisation cares about my emotional wellbeing'
Note: Totals may vary due to rounding.
Source: VAGO CPP survey.
These results show a difference in how CPPs perceive the support of their day-to-day management compared to their organisational leaders. Results of the 2016 PMS provide further evidence of this difference—27 per cent of respondents that indicated they intended to leave child protection cited 'lack of confidence in senior leadership' as a major factor in their decision to leave.
The underlying reasons for this difference are unknown—without consolidated information about how senior management addresses CPPs' mental health issues, we are unable to identify the key issues preventing greater confidence.
Interestingly, experts such as Doctor Peter Cotton—a leading Australian expert in clinical and organisational psychology—emphasise the role of leadership in occupational wellbeing. Specifically, programs that focus on improving the quality of leadership practices and organisational climate are likely to have a greater impact on reducing workers' compensation premiums than traditional OHS risk management approaches.
Workload and work-life balance
The impact of CPPs' excessive workloads was evident in the 2015 PMS. Figure 4E shows that only 58 per cent of CPP respondents agreed or strongly agreed with the statement 'I am able to effectively manage my workload'.
Figure 4E
PMS results, 2015: 'I am able to effectively manage my workload'
Source: CPP responses to the PMS.
Figure 4F shows that in 2016, only 34 per cent of CPP respondents agreed or strongly agreed that their workload was appropriate for the job they do.
|
'I have two young children (6 and under) and I am always working early finishing late. My inability to manage an effective work-life balance will mean I will seek other employment soon.' —CPP survey respondent |
Figure 4F
PMS results, 2016: 'The workload I have is appropriate for the job I do'
Source: CPP responses to PMS.
Across a number of years, PMS results consistently show CPPs' high dissatisfaction with their work-life balance and, more recently, with support for work-life balance—see Figures 4G and 4H.
Figure 4G
PMS results, 2013 to 2016: 'Considering your work and life priorities, how satisfied are you with the work/life balance in your current job?'
Note: Totals may vary due to rounding.
Source: CPP responses to the PMS.
Figure 4H
PMS results, 2016: 'My organisation encourages and supports employees to have a good work-life balance'
Note: Totals may vary due to rounding.
Source: CPP responses to the PMS.
Our survey results support the PMS data on the impact of CPPs' workloads on their personal lives—50 per cent of respondents disagreed somewhat or strongly that they can reasonably manage the demands of both their work and personal lives, as shown in Figure 4I.
Figure 4I
CPP survey results, 2017: 'I am able to reasonably balance the demands of work and personal life'
Note: Totals may vary due to rounding.
Source: VAGO CPP survey.
In 2016, 56 per cent of CPP respondents to the PMS who indicated that they intended to leave child protection cited excessive workload as the reason.
WorkCover claims
WorkSafe Victoria is the state's health and safety regulator. As its remit covers all Victorian workplaces, it is physically impossible for WorkSafe Victoria to actively monitor every organisation. Accordingly, it uses a risk-based approach to identify and monitor high-risk industries, and respond to reports of breaches of the OHS Act. WorkSafe Victoria may inspect child protection workplaces if it receives reports from health and safety representatives. It also follows up provisional improvement notices and conducts site visits to verify that DHHS has addressed any reported health and safety issues.
WorkSafe Victoria's site inspection reports repeatedly show that understaffing is driving poor mental health outcomes for CPPs.
WorkSafe Victoria's research in 2017 found healthcare and social assistance services—which includes CPPs—accounted for the highest volume of mental injury claims in Victorian workplaces. Accordingly, WorkSafe Victoria's 2017–18 business plan identifies social assistance services as one of its top priority industry subdivisions, as shown in Figure 4J.
Figure 4J
Priority industry subdivisions in WorkSafe Victoria's 2017–18 business plan, in order of priority
|
1. Public order, safety and regulatory services 2. Social assistance services 3. Residential care services 4. Building construction 5. Transport support services |
Source: WorkSafe Victoria's 2017–18 business plan.
The cost of psychological injury
WorkSafe Victoria estimates that a mental injury claim costs, on average, 30 per cent more than a musculoskeletal disorder claim. In addition, Comcare's guide for preventing workplace psychological injury states that employees who make psychological injury claims generally take two to four times more unplanned leave than other employees prior to submitting the claim.
Australia's Mentally Healthy Workplace Alliance released a study in 2014 focused on the cost of mental health conditions in one year across Australian workplaces. It estimated that mental health conditions cost $4.7 billion in absenteeism, $6.1 billion in presenteeism and $146 million in compensation claims. The study notes that the combined figure of almost $11 billion does not include the additional costs associated with management, turnover and insurance.
At the same time, Dr Peter Cotton has estimated that up to 60 per cent of psychological injury claims can actually be prevented by improving morale and building supportive leadership and work teams.
CPP mental health claims
Mental health claims are an indicator of an organisation's psychological health and safety status.
DHHS data shows that in 2016–17:
- 31 per cent of all DHHS WorkCover claims related to mental health
- 49 per cent of all CPP WorkCover claims related to mental health.
From 2012 to 2016, WorkSafe Victoria data shows $9 816 914 in payments was made for claims related to CPPs' mental health, as shown in Figure 4K.
Figure 4K
WorkCover payments related to CPPs' mental injury claims, 2012 to 2016
Source: VAGO based on WorkSafe Victoria data.
|
'My mental health has deteriorated cumulatively in the four years I have worked with the department, due mainly to the unreasonable hours I am expected to work without recompense.' —CPP survey respondent |
Accurate trend analysis is limited because the relatively small number of claims made each year by CPPs means even one claim can raise total payout levels significantly. Instead, looking at the types of mental injury payments made and their prevalence over time can provide useful insights—see Figure 4L.
Figure 4L
Types of WorkCover payments related to CPPs' mental health, 2012 to 2016
Note: Totals may vary due to rounding.
Source: VAGO from WorkSafe Victoria data.
From 2012 to 2016, work-related harassment and/or workplace bullying and work pressure made up the majority of CPP WorkCover payments for mental injury claims. In 2012, 2013, 2014, 2015 and 2016, they comprised 75.0, 72.2, 60.0, 80.0 and 94.4 per cent of claims, respectively.
These results are consistent with our finding that workload is the primary contributor to poor mental health.
|
'In Ireland and the UK staff work in child protection for life but here I understand from students that lecturers at university have informed them the longest period of time they can expect to work in child protection is four years. I was alarmed when I first heard this directly from students but can now see it is an accurate estimate. Add to this the demands of attending court, being verbally abused on the stand, interrogated as to whether one is qualified enough to even speak to a child, fear and intimidation from clients and disrespectful interactions with external agencies leads me to believe this job is not possible to maintain.' —CPP survey respondent |
Bullying and harassment is also an increasingly reported concern in PMS results, along with a lack of confidence in DHHS's grievance processes—see Section 2.4. This lack of confidence may be contributing to the prevalence of CPPs' harassment and bullying WorkCover claims. There is value in DHHS working to understand whether there is a link between the two—and if so, what improvements would build staff confidence.
Persistent turnover in CPPs
CPPs need to be resilient, have management's confidence to work effectively, and be confident that management will appropriately support them to do so. Where this is missing, workplaces can lack cohesion, be blame-oriented, and be subject to unnecessary challenges to decision-making at all levels.
Such environments make it difficult to retain staff and may result in reduced service quality and continuity for clients. This can, in turn, give the organisation a poor reputation and hinder recruitment. It can also increase costs due to an ongoing need for recruitment and induction.
DHHS's CPP Workforce Strategy describes the child protection workforce as 'a specialist, expert workforce'. It also discusses DHHS's heavy reliance on internal progression because of insufficient alternative entry pathways for experienced recruits.
DHHS states that 'the creation of a continued pipeline of suitably skilled practitioners at entry and advanced levels is critical to a well-functioning child protection service'. With excessive workload driving CPP mental health risks and contributing to turnover, DHHS has also advised government that without investment to increase the child protection workforce, the current high staff turnover—shown in Figure 4M—will continue.
Figure 4M
Annual staff turnover for DHHS overall and CPPs, 2012–13 to 2016–17
Note: DHHS was unable to provide CPP turnover rates for 2014–15.
Source: VAGO based on DHHS data.
The impact of the persistently high turnover of CPPs is well documented in records from workload review panels. Teams across the state frequently report on what could be described as the crippling impact of staff absences—resulting in other team members working overtime, and delaying or cancelling activities that are not crisis-oriented.
The impact can be particularly severe when core case carrying staff—CPP-3s and CPP-4s—leave the workforce soon after completing the mandatory 'Beginning Practice' training. Figure 4N shows the average length of employment for CPP-3s and CPP-4s from 2012–13 to 2016–17.
Figure 4N
Average length of CPP-3 and CPP-4 employment, 2013 to 2017
Source: VAGO based on DHHS data.
The CPP Workforce Strategy discusses the challenges of recruitment and retention of CPPs, stating 'a high volume of staff performing higher duties … and fixed-term staff backfilling ongoing roles further impacts on the total number of vacancies and ability to recruit'.
From 2012–13 to 2016–17, the core case-carrying workforce—CPP-3s and CPP-4s—had an average tenure of 2.56 and 6.14 years respectively. Figure 4O shows the recruitment and training costs for these two classifications during this period.
Figure 4O
Recruitment and training costs for CPP-3 and CPP-4, 2012–13 to 2016–17
|
Classification |
Quantity |
Cost per CPP |
Total |
|---|---|---|---|
|
CPP-3 |
1 643 |
$4 644 |
$7 630 092 |
|
CPP-4 |
659 |
$8 700 |
$5 733 300 |
|
Total recruitment cost |
$13 363 392 |
||
|
Total training cost |
$4 120 000 |
||
|
Total recruitment and training cost |
$17 483 392 |
||
Source: VAGO based on DHHS data.
Because this data does not include the costs of recruiting and training other CPP levels (2, 5 and 6), or training programs in addition to 'Beginning Practice', the total cost of persistent practitioner turnover is likely to be higher again.
Our analysis shows that if DHHS had been able to lower the CPP attrition rate to the DHHS average, it could potentially have saved more than $650 000 in avoidable recruitment and training costs for 2012–13 to 2016–17.
DHHS's 2011 study of the child protection workforce provides the most recent data on the challenges facing CPPs in the first year of their employment. At one month, 23 per cent of CPPs reported concerns about work-life balance. By four months, this had risen to 46 per cent and, by nine months, 90 per cent.
DHHS's CPP Workforce Strategy intends to address the program's recruitment and retention issues through an informed workforce planning model to better forecast workforce needs. It also plans to offer a support service for all newly engaged CPPs, through which they will receive specialised and intensive administrative support during their first 12 months as a CPP.
[1] In this instance, ‘administrative’ refers to the various case management tasks that are separate from client and family/guardian engagement. Examples include court-related administration, contact facilitation (scheduling, transport and administration), and intelligence exchange with other service professionals.
Appendix A. Audit Act 1994 section 16—submissions and comments
We have consulted with DHHS and WorkSafe Victoria, and we considered their views when reaching our audit conclusions. As required by section 16(3) of the Audit Act 1994, we gave a draft copy of this report, or relevant extracts, to those agencies and asked for their submissions and comments. We also provided a copy of the report to the Department of Premier and Cabinet.
Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
RESPONSE provided by the Secretary, DHHS
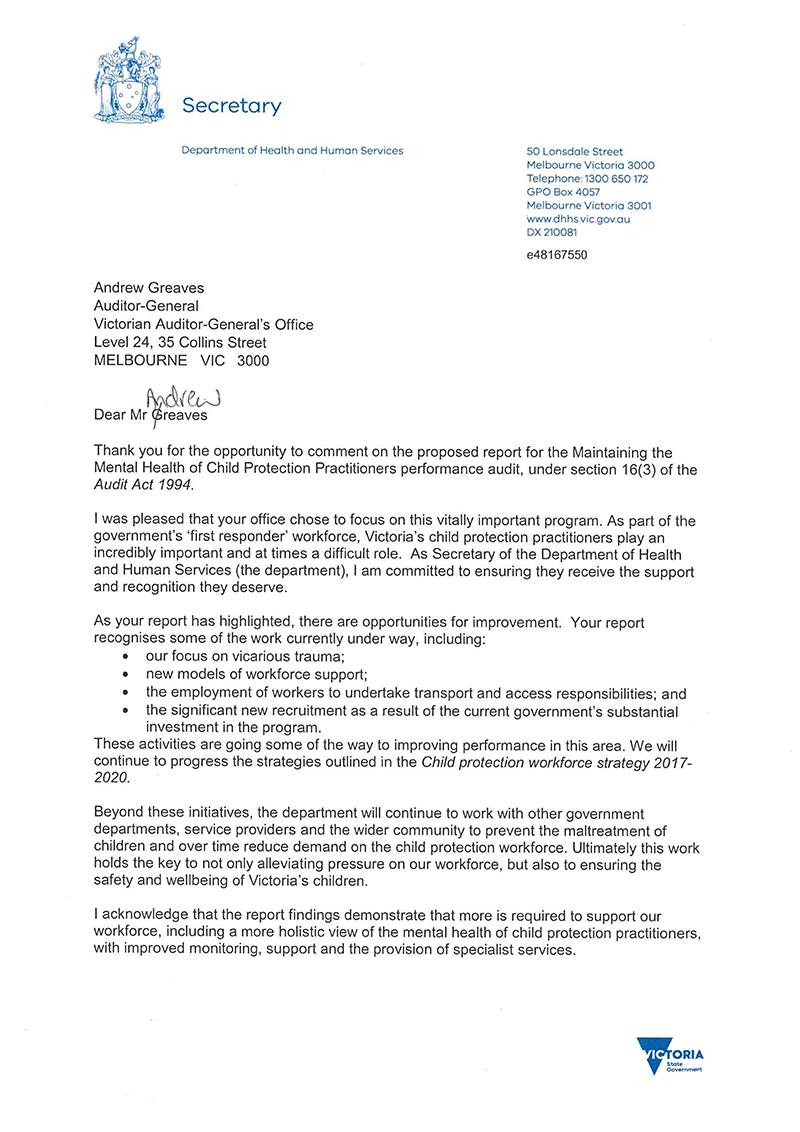
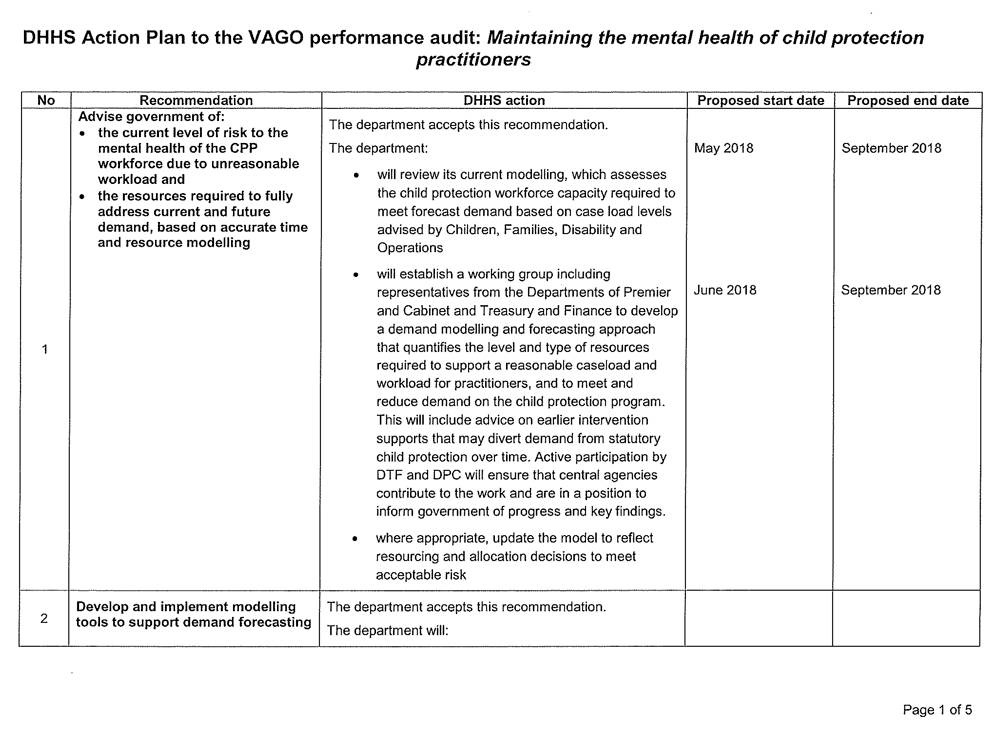
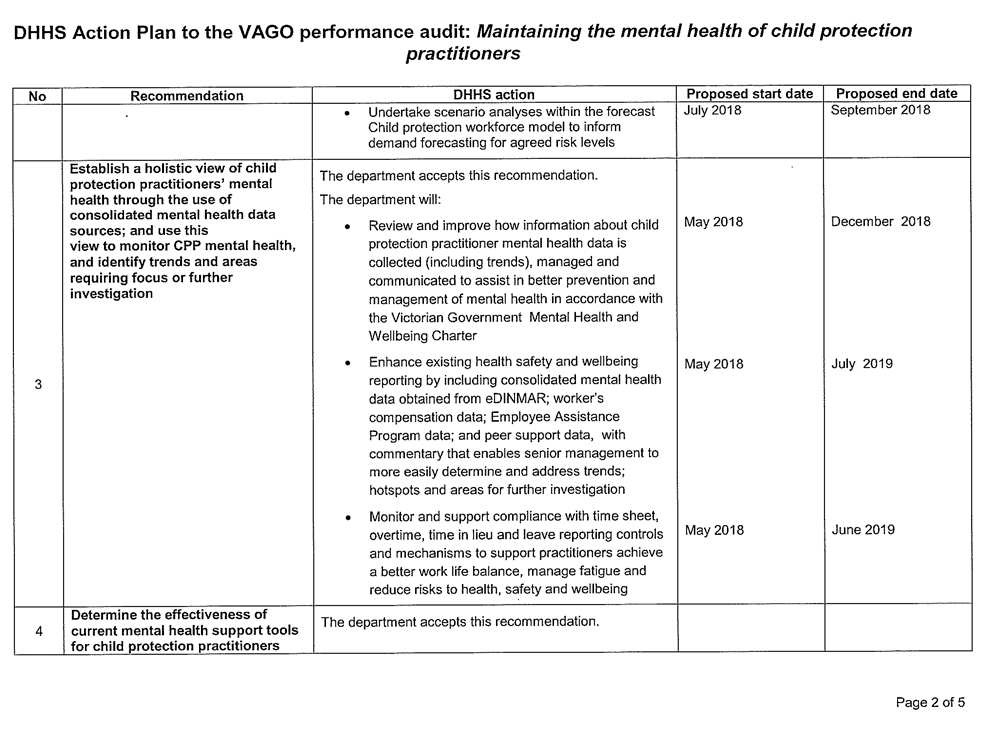
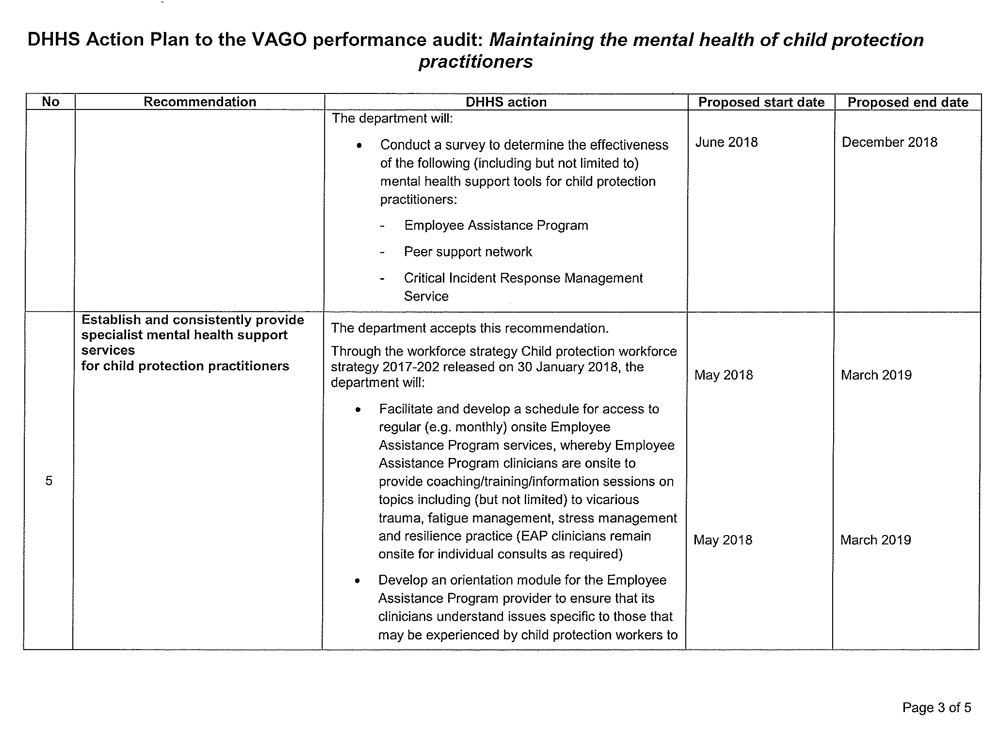
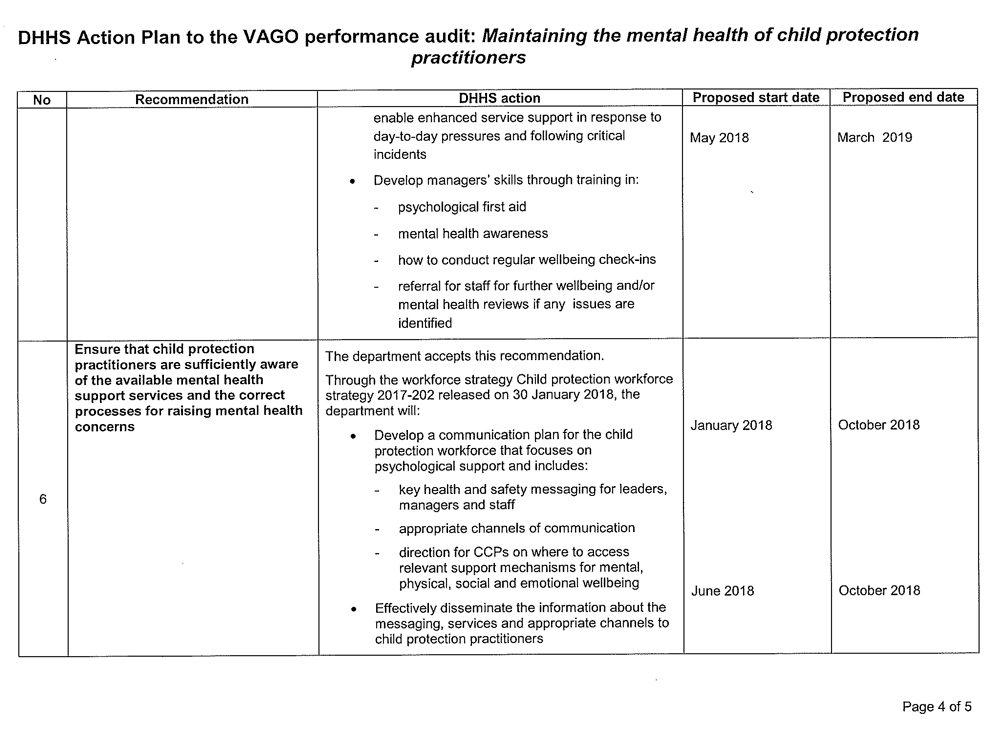
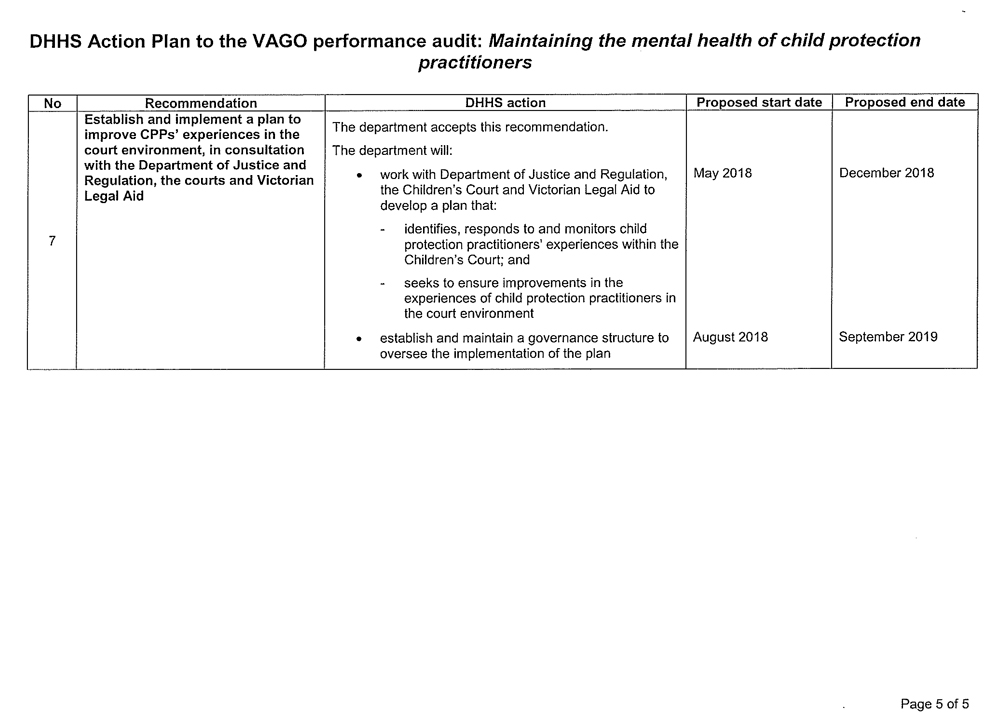
RESPONSE provided by the Chief Executive, WorkSafe Victoria
Appendix B. CPP classifications and roles
Figure B1
Classification and description of CPP roles
|
Classification |
Role |
Description |
|---|---|---|
|
CPP-2 |
Case support worker |
Tasks include facilitating contact visits, transporting children and other case support duties. |
|
CPP-3 |
Practitioner |
Entry level for child protection CPPs, with case management responsibilities. |
|
CPP-4 |
Advanced practitioner |
Perform case management and other functions at an advanced level. |
|
CPP-5 |
Team manager |
Have a broad range of delegations, including some budgetary and formal HR responsibilities, and endorsing statutory case planning decisions. |
|
CPP-5.1 |
Senior child protection practitioner |
Report to team managers and undertake co-work, mentoring and formal supervision of up to three CPP-3 staff. Carry a case load commensurate with their other duties. Some senior CPPs do not have supervisory responsibilities. |
|
CPP-5.1 |
Senior child protection practitioner (community based) |
Co-located in a registered family services agency and a child protection office. Report to the practice leader and manage unborn reports and case transitioning to Child FIRST. The role does not have direct supervisory responsibilities. |
|
CPP-5.1 |
Senior child protection practitioner (court officer) |
Assist CPPs at court with legal advice, and facilitate court skills training. The role does not involve formal supervisory responsibility, but does provide live supervision, mentoring and support to CPPs at court. |
|
CPP-5.2 |
Practice leader |
Report to area managers and undertake co-work, mentoring, live supervision of CPP-3, -4 and -5 staff, and supervision of community‑based advanced CPPs. Carry a case load commensurate with their other duties, and are responsible for quality auditing, capability development, case practice, and case planning guidance. |
|
CPP-6 |
Principal practitioner |
Provide peer support and practice guidance resources for divisions. Carry a case load commensurate with their other duties. |
|
CPP‑6.1 |
Deputy area manager |
Responsible for assisting the area manager in regional operational management. Provides leadership in local service planning and stakeholder engagement. Directly supervises the team managers and practice leaders in the local area. |
|
CPP-6.1 |
Area manager Area manager (regional services) |
Provide strategic leadership across the area—including local service planning, ministerial briefings, stakeholder engagement, and operational management across the local child protection catchment (financial, some budget, HR and performance management). Responsible for supervising area team managers, practice leaders and deputy area managers. |
|
CPP-6.2 |
Operations manager |
Responsible for management and oversight of all aspects of divisional child protection operations—including strategic directions, workforce, operational decision making and review, quality assurance and performance monitoring. |
Source: DHHS Child Protection Manual.
Appendix C. Phases in the child protection process
DHHS's Child Protection Manual outlines the different phases and processes in child protection. The figures in this appendix summarise the steps involved in each phase or process, as shown in Figure C1.
Figure C1
Child protection phases shown in this appendix
|
Figure |
Phase/process |
|---|---|
|
C2 |
Case planning |
|
C3 |
Investigation |
|
C4 |
Protective intervention |
|
C5 |
Protection order / protective application |
|
C6 |
Legal process |
|
C7 |
Direction to resume parental responsibility |
|
C8 |
Placement process |
Source: VAGO.
Figure C2
Child protection process: Case planning
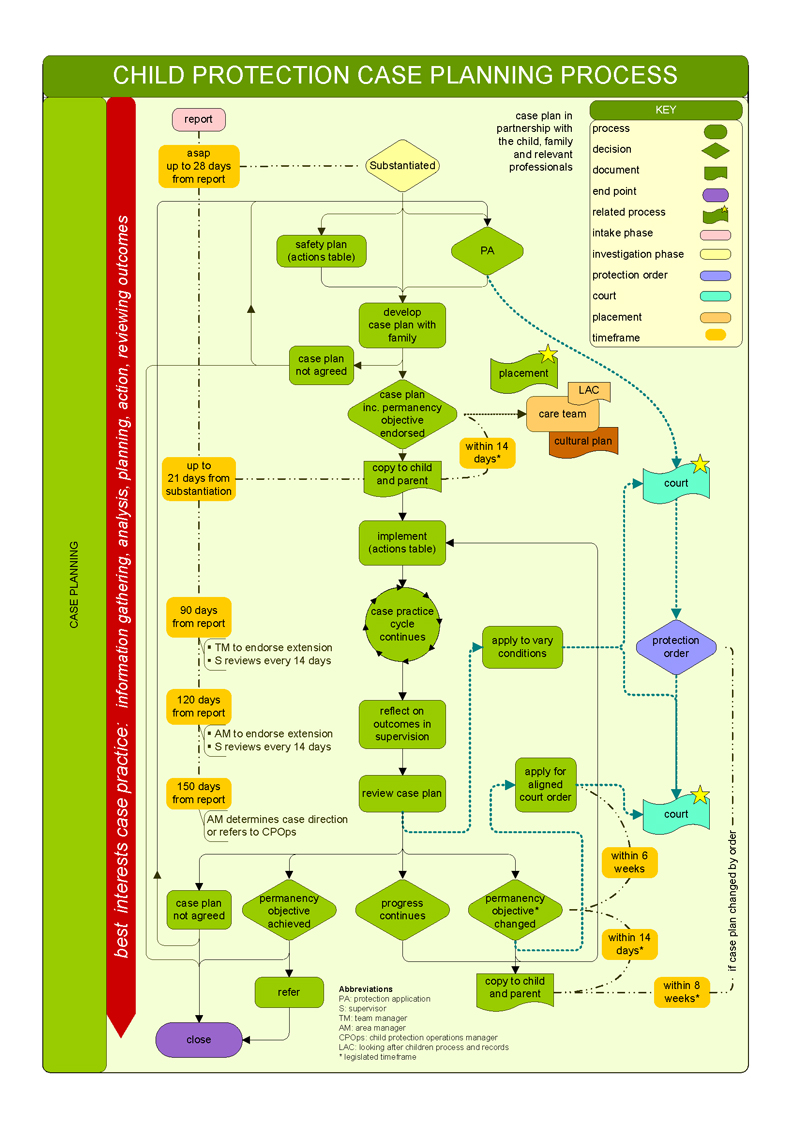
Source: DHHS Child Protection Manual.
Figure C3
Child protection phase: Investigation
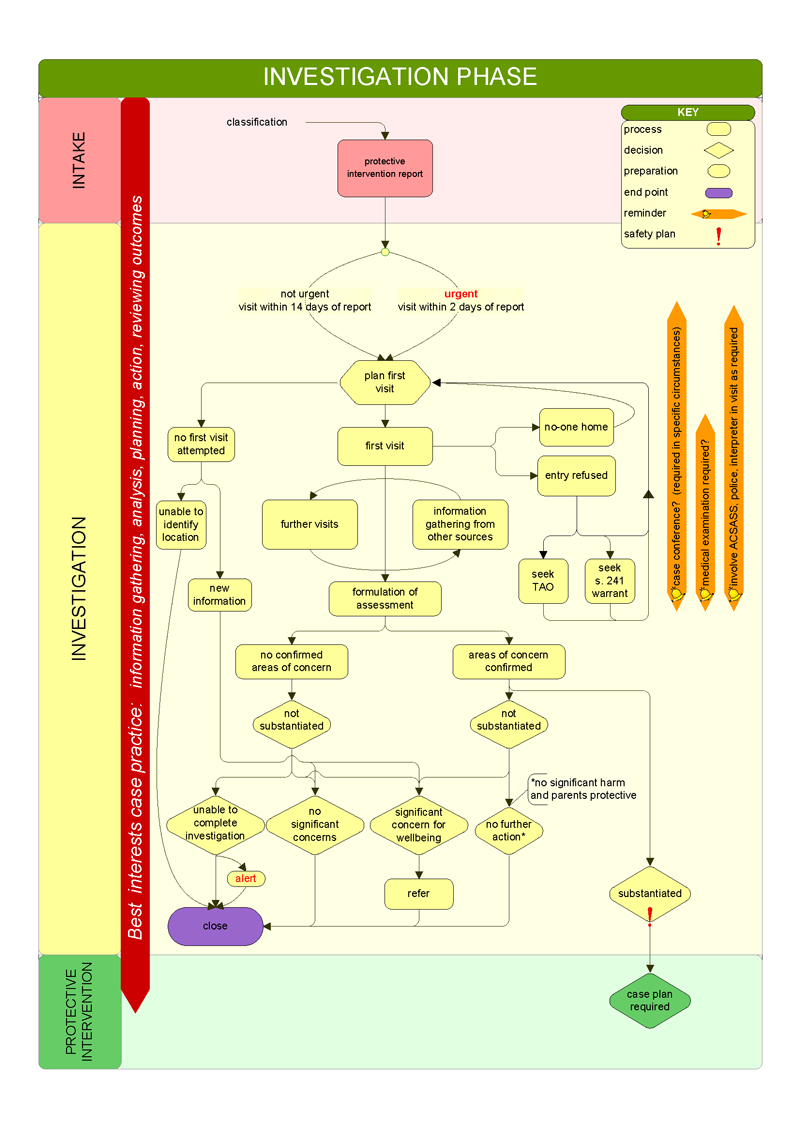
Source: DHHS Child Protection Manual.
Figure C4
Child protection phase: Protective intervention
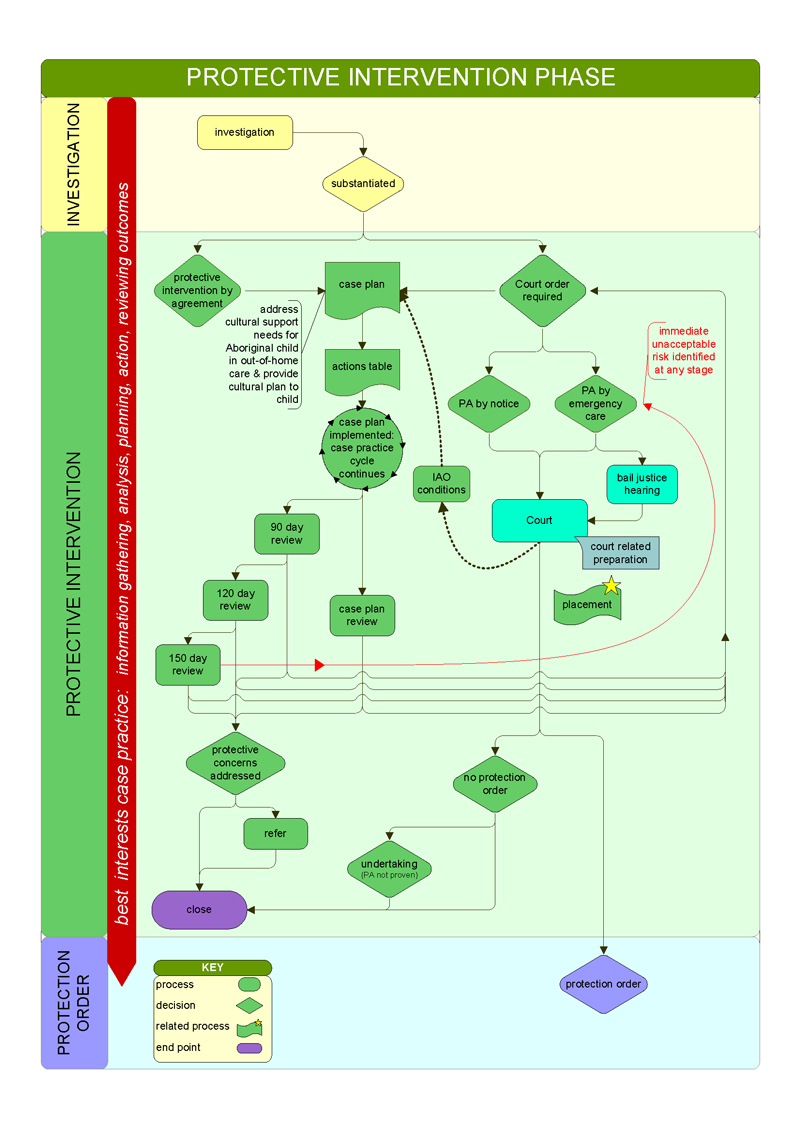
Source: DHHS Child Protection Manual.
Figure C5
Child protection phase: Protection order / protective application
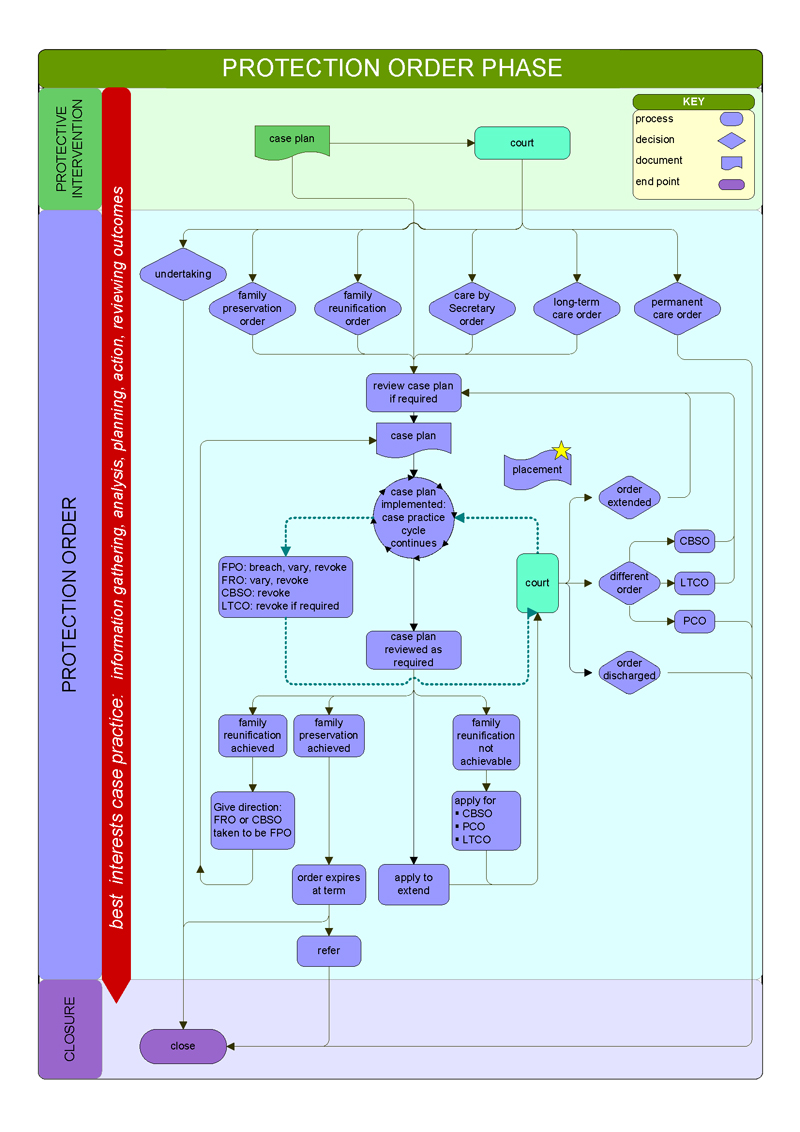
Source: DHHS Child Protection Manual.
Figure C6
Child protection process: Legal process
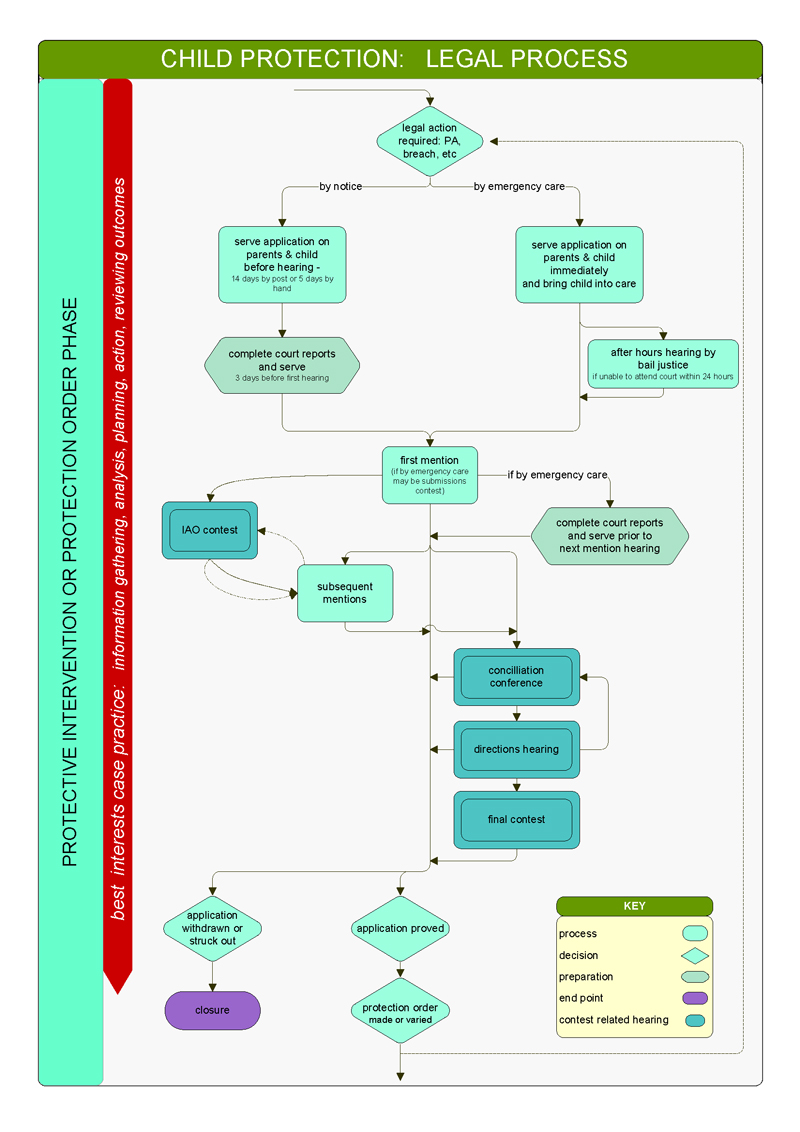
Source: DHHS Child Protection Manual.
Figure C7
Child protection process: Direction to resume parental responsibility
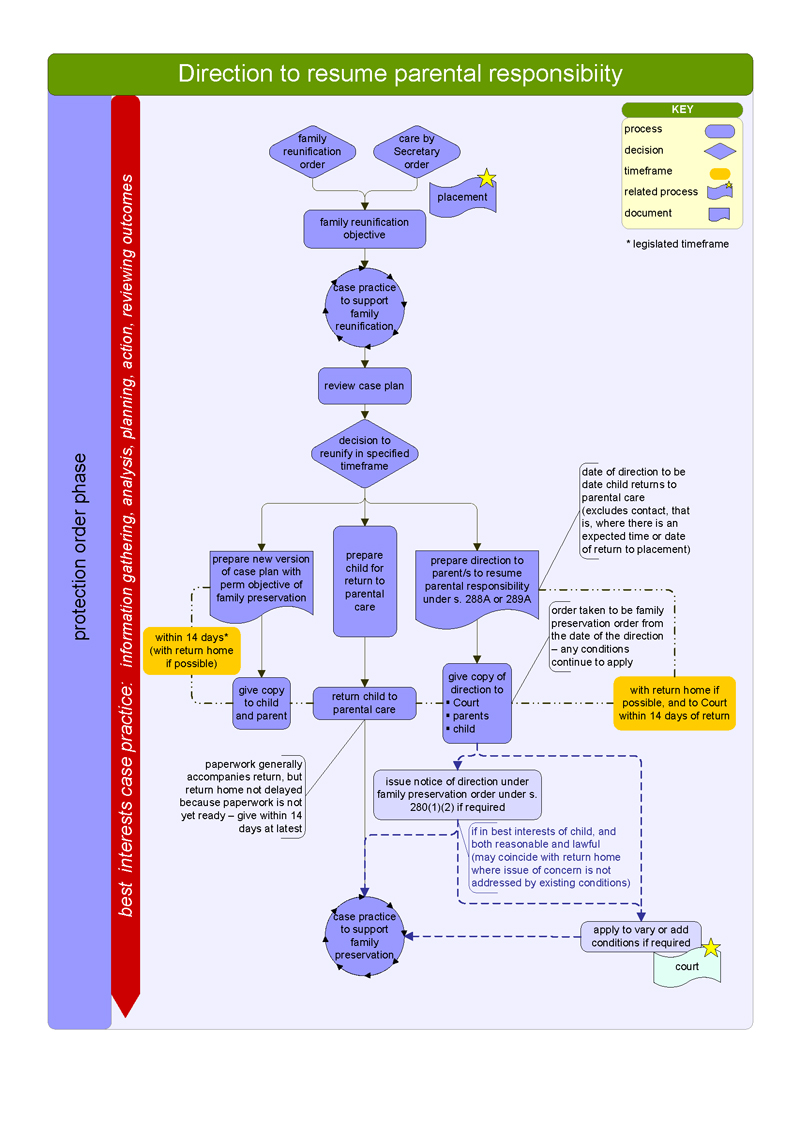
Source: DHHS Child Protection Manual.
Figure C8
Child protection process: Placement process
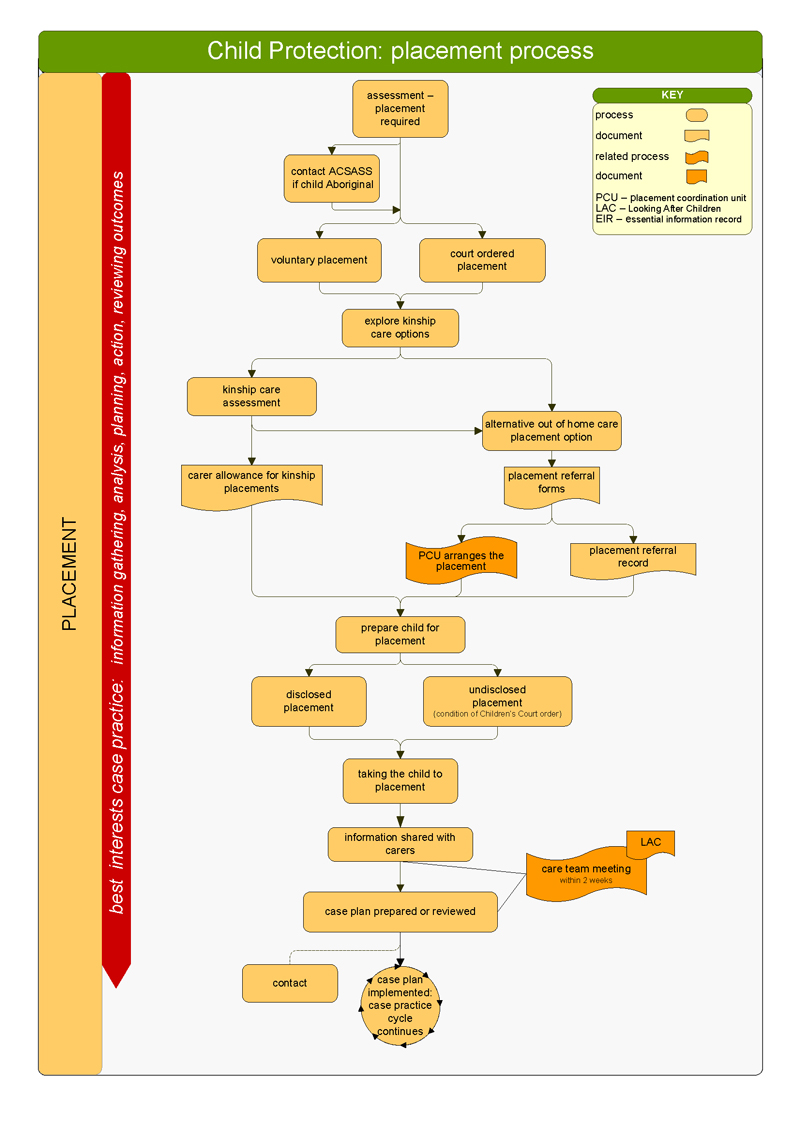
Source: DHHS Child Protection Manual.
Appendix D. CPP supervision requirements
Figure D1
Supervision requirements for CPPs by classification
|
Classification |
Total hours(a) |
Scheduled hours(b) |
Balance of supervision(c) |
|---|---|---|---|
|
CPP-2 |
2 per month |
1 per month |
|
|
CPP-3 beginning practice |
3 per fortnight |
2 per fortnight |
During the weeks when beginning CPPs are attending the 'Beginning Practice' clinics the supervision requirement will revert to two hours of supervision per fortnight including one hour of scheduled supervision. |
|
CPP-3, 4 and 5 case carriers and managers who supervise staff and cases |
2 per fortnight |
1 per fortnight |
|
|
CPP-3, 4 and 5 central after-hours service staff (including AHCPES(d), AHCPPS(e), and Streetwork Outreach Service) |
6 per roster cycle (6 weeks) |
1 per roster cycle |
|
|
CPP-5 child protection court officers |
2 per month |
1 per month |
Divisional principal CPPs will also undertake supervision with a statewide principal practitioner. |
|
CPP-6 principal practitioner |
1 per fortnight |
1 per fortnight |
– |
|
CPP-6.1 and 6.2 area manager / child protection operations manager |
1 per month |
1 per month |
– |
|
Student |
2 per fortnight |
1 per fortnight |
|
|
Part-time or casual |
The frequency of supervision for part-time and casual staff is the same as for full‑time staff, but the duration is determined on a pro-rata basis. |
||
(a) The total number of hours of supervision that must be provided to staff.
(b) The number of hours of supervision (out of the total) that must be provided to staff as scheduled supervision.
(c) The ways in which the remainder of the total number of hours of supervision are permitted to be provided to staff.
(d) AHCPES = After Hours Child Protection Emergency Service.
(e) AHCPPS = After Hours Child Protection Placement Service.
Source: VAGO based on DHHS's Child Protection Manual.
Appendix E. Comments from CPPs
The following are a representative selection of the comments that were made in response to our survey questions and during CPP forums during site visits and CPP interviews.
Workload
|
'There are never enough hours in the day and sometimes there is a sense of “damned if you do and damned if you don't”.' |
|
'Demand is such workers no longer feel they are doing a good job—they feel everything they do is “light touch”.' |
|
'There are unrealistic expectations placed on CPPs around workload and the time it takes to complete an endless amount of tasks—all of equal importance under the ridiculous assumption you can achieve it all in 7.36 hours per day.' |
|
'The department relies on the goodwill of staff to go the extra mile, work extra hours, etc.—but this cannot go on forever without having a significant impact on staff wellbeing.' |
|
'Child Protection has to do more and more. The workload and additional administrative tasks in the role continue to increase. The role is much less about achieving positive outcomes for children at risk and supporting them being safe at home or placed into more appropriate care options. The role is now just constant reporting about the DPAC [Departmental Divisional Performance and Assurance Committee], performance data, meeting KPIs and crises driven.' |
|
'I regularly work 80 hours a week and have to set my alarm at 4am to start work in case I get caught up in another urgent matter which I had not previously featured into my diary.' |
|
'The main issue seems to be workload. It's too high for anyone to reasonably keep on top of, and do a good job.' |
|
'It is not unusual for a sole worker to have worked all day and then have to travel for hours to deliver a child to a placement, and then have to drive back again on their own.' |
|
'The Department holds workers responsible for not completing tasks, even when it is very clear that there is not enough time to complete them. If workers are not completing tasks the Department puts them on a work performance supervision program and increases the distress and anxiety workers are suffering.' |
|
'If a [CPP-3 or CPP-4] is protected with their wellbeing by workload management—you can be guaranteed the CPP-5s are burdened beyond reasonable standards. There is no protection for management rather the expectation that CPP-5s protect their supervisees (as well they should) but at their own expense.' |
|
'Workloads are the biggest issues for Child Protection staff.' |
|
'This practice enables workers to be able to do very little work on their cases, it provides just enough to keep it from falling behind.' |
|
'I do not have one office but three to cover, leaving me travelling from place to place to the point of exhaustion; this does not include having to attend meetings at other venues, often at short notice.' |
|
'There is nothing proactively done about workload management and it is only when either an incident occurs, physical health deteriorates that options for “well-being” come into effect.' |
|
'I think staff get sick a lot, possibly this is … likely to be because of the workload, stress and adrenalin and late nights.' |
|
'Although practitioners have knowledge of self-care skills, this is rarely implemented and the practitioners are often forced to sacrifice their “work life balance” to have work completed.' |
|
'There are a lot of unallocated clients (that is a client where there is no CPP assigned to the case). These clients are managed as tasks arise and there is a need, not in a proactive way.' |
|
'Every program area is under this pressure. Managers are under pressure. No matter how the work is allocated throughout the organisation there is always too much work and not enough CPPs to do the work.' 'The demand is relentless and there are times when I feel so overwhelmed it is almost paralysing.' 'The organisation will say that there is the workload monitoring and review panels. These do not change the workload. These panels have been ongoing for many years and the issues of workload persist. The organisation will also say that “workload is a question of an individual's capacity, all individuals are different therefore each worker needs to talk to their manager about what they can achieve”. The way the individual worker has to deal with this is to negotiate directly with their supervisor about their workload. There are inherent problems with this. There is a power imbalance between the worker and their manager, it is difficult for the individual worker to tell their manager that they are being allocated too much work and are struggling and stressed. The worker will be concerned that they will be viewed by management as:
It is not appropriate for a CPP to base their workload on negotiating with their manager as the manager has all these unallocated children and is under pressure from their manager to get all the work done. This pressure is passed on to the CPP which causes a work environment were the worker is under constant pressure, is stressed and feels like no matter how hard they work they will never get on top of all the work. It is not fair for a new CPP to be negotiating with an experienced manager who needs to allocate a lot of work.' |
|
'We are told by management all the time that we need to ensure self-care, take breaks, leave etc. and it is constantly implied that it is our responsibility however a workplace framework that allows you to do these things and be able to manage a work-life balance does not exist.' |
|
'The families that Child Protection get involved in are difficult, damaged families and they need a lot more than three phone calls from our community agencies before they close.' |
|
'Also be aware that the department will say that the average case allocation per CPP is well under 24 children. The way this number was arrived to needs to be scrutinised as the average CPP is not allocated any less than 24 children.' |
Staff retention
|
'A huge impact on mental health at work is lack of retention of staff and staff shortages. When programs are not fully staffed the workload substantially increases for individual workers and teams.' 'When this environment is sustained over a period of time it has a cumulative detrimental impact on mental health. People work long hours, become tired, sick and resentful.' |
|
'There are multiple CPP vacancies however this is not taken into account with workloads and regardless of the number of vacancies in a team the existing staff are expected to cover everything.' |
|
'They [CPP-3s and CPP-4s] are exhausted and a high number leave after 18 months.' |
|
'DHHS allows some managers to bully others and not to follow a professional standard simply because finding replacements would be hard.' |
|
'This is the first time in my life when I have questioned whether I want to continue in this field as these are the worst working conditions I have ever experienced.' |
|
'I attended my GP last week at the point of exhaustion who informed me I was burned out which I know is work related but I cannot see any way forward other than to leave a job I have loved for a quarter of a century and one which I have always been able to manage the demands and achieve a work life balance.' |
|
'We cannot get to complete good work with our families and engage them in the process of change due to time restraints due to staff shortage and lack of support from management.' |
Professional standing
|
'When other professionals in the community have a poor view of CPP staff, as a result of staff being stressed, under resourced and trying to manage a broken system, this also adds to a sense of worthlessness and alienation.' |
|
'Child Protection is a fairly thankless task and the perception by the community does have an impact on job satisfaction at times.' |
|
'There is no positive media about Child Protection, there should be a media campaign about all the good we do rather than only ever hearing about the tragedies and our inadequacies.' |
Supervision
|
'My immediate supervisor is under a great deal of stress and pressure due to operational issues that he is struggling to provide the quality support required.' |
|
'Supervision does not happen or happens occasionally due to work demands.' |
|
'Limited supervision provided often task focused.' 'Supervision is often administrative in nature. Because supervision is conducted by the worker's direct line management, there is a concern that what is discussed in supervision will be factored into performance appraisal. This makes it difficult to discuss anything that might be considered a “weakness” (such as wellbeing issues).' |
Conduct towards CPPs
|
'One senior manager … told me that the conduct … did not apply to one individual despite their poor behaviour. The reason cited was that the individual was an experienced worker and needed to be retained at all costs. This statement was made in front of [redacted]—who corrected them, but still the behaviour was allowed to continue without being held to account.' |
|
'Workers who have had formal complaints about bullying have been promoted within the organisation into a higher position than they were in previously.' |
|
'Issues such as bullying go unaddressed for extended periods of time and processes to address these behaviours often do not result in any changes to the concerning behaviours …' |
|
'There is also a concern as to workplace bullying and the obvious impact that this has on mental health.' 'I still think that not a lot is done to address workplace bullying despite departmental initiatives.' |
|
'There is lateral violence observed between Team Managers and Senior Practitioners and between Team Managers so they can be seen as the best person for the role and adhering to the various KPIs that exist. In Team Managers meetings they unfortunately put practitioners down and discuss them in a negative manner.' |
|
'Bullying behaviours are rewarded and there are no consequences to behaviours. Practitioners are reluctant to discuss these issues with their Team Managers who are frequently in strong friendships with the bully and little to nothing is done to address this issue which is rife.' 'Perpetrators who demonstrate violence (emotional and psychological) to practitioners are hard to prove; even though there is an internal formal investigation, the outcome is not effective with perpetrators of bullying behaviour often rewarded for their behaviours by engaging in promotions as a Practice Leader or Principal Project Officer positions. This demonstrates to practitioners that disclosing bullying behaviours is not worth the risk.' |
Experiences in the court environment
|
'Brutality.' |
|
'The Team Managers and Team Leaders must learn though exposure to the court environment, although these exposures are often negative ones.' |
|
'The people in the court system have little regard or respect for CPPs.' |
|
'CPP workers are devalued by the Children's Court process where workers are treated shabbily by Magistrates and opposing legal counsel. There are no sanctions for legal reps who make personal attacks on workers and question their professionalism as we try to do our work. Many workers have been traumatised by their experiences at Court.' |
|
'If we do a good job then no one says anything in the organisation, and we never hear about the clients. If something goes wrong then usually the Court will reprimand the CPP publicly, or management will have one of those “supportive” conversations with you.' |
|
'When something goes wrong, no-one thinks about what the magistrate said.' |
|
'The courts make impractical decisions—such as a child with multiple fractures being transported for four hours a day in a car seat (which distresses the child).' |
|
'The court system is the primary difficulty—the demands are not unreasonable, it's just that they're physically impossible.' |
|
'The judges lack an understanding of our workload.' |
|
'All other areas are given extensions/deferments due to workloads or delays—but not us.' |
|
'Magistrates are hugely powerful—and unsympathetic to the administrative difficulties of child protection.' |
|
'Court has the expectation that there are government resources that can be called on—court considers that it is making the best directions in care of the child, and the resources to do so are your concern.' |
|
'CPPs do not have enough time to do quality work and are then torn to shreds on the witness stand.' |
|
'[at court] I'm getting told off for a system that's in crisis.' |
|
'You get yelled at by judges.' |
|
'Judges bully you.' |
|
'We are bullied by barristers.' |
|
'Unprofessional behaviour and definite bullying, “getting dressed down”.' |
|
'Workers have come back crying.' |
|
'The independence of the judge tends to result in magistrates not being accountable for their behaviours.' |
|
'We are subject to personal attacks from judges and legal representatives.' |
|
'Solicitors think that they are in another league to CPPs—they are rude and there are no repercussions for them.' |
|
'Parents feel empowered by poor behaviour and then do likewise.' |
|
'The Children's Court is the only court environment where lawyers are allowed to be so disrespectful—they [mother, father and lawyer] hunt as a pack.' |
|
'People in the court are disrespectful, unprofessional, belittling, bullying and use standover tactics and intimidation.' |
|
'There's a higher focus on the parents' needs than the child's—it's all about solicitors talking about parents' needs.' |
|
'Threats to physical safety are not being taken seriously by magistrates (personal safety plans are overridden by magistrates).' |
Perceptions of supervisors and the organisation more broadly
|
'I believe my immediate supervisor cares about my emotional wellbeing but she is overloaded with demands of her role and can't afford time to focus on my needs.' |
|
'She absolutely cares however I don't believe she has the capacity or time to support me as she is busy with her own case load…' |
|
'My immediate supervisor is under a great deal of stress and pressure due to operational issues that he is struggling to provide the quality support required.' |
|
'I would like to feel valued for the job I do. I do from my Team Manager, however I mean from higher up.' |
|
'The organisation cares as long as you are well. If you are emotionally unwell, even for a short period of time, and this is known to management or other staff around you, management see this is as you not having the capacity to cope and effects any career advancement opportunities…' |
|
'Good work is rarely recognised but any issues are harshly challenged.' |
|
'When an organisation allows its workforce to become depleted, stressed and overworked and does not attempt to address any of the identified issues, until the workforce feels that the only avenue to address the problems and obtain assistance from the union, it does not lead to a healthy and productive workgroup.' |
|
'Priority appears to be the business needs of the unit over work-life balance and health and wellbeing of employees.' |
|
'The practice of senior managers focussing only on meeting targets and KPIs is detrimental to the organisation's capacity to care about their workers/staff and to support the maintenance of a healthy workforce.' 'Senior management is located in metropolitan areas, which means that we rarely see them, they lack insight into the challenges of rural work and if we wish to access them, there can be a wait until this can be achieved.' |
Taking TIL/leave/work breaks
|
'There's always a sense of raised eyebrows.' |
|
'If workers take sick leave or stress leave, this is viewed negatively and as though they are not coping, rather than the system is at fault.' |
|
'Though leave is encouraged it is unavailable as staff are competing for time off.' |
|
'On multiple occasions I have had leave or TIL denied, even with it being booked months in advance.' |
|
'Workloads are such that entitled breaks are not taken—can cause more stress to have the time away from your work.' |
|
'Flexible work arrangement i.e. applications for purchased leave are often not approved.' |
|
'This is frowned upon. The idea of missing a meeting/deadline because of the need to have a break is really critically viewed.' |
|
'Though leave is encouraged it is unavailable as staff are competing for time off.' |
|
'If I discussed [the constant need to work overtime to perform my role effectively] with my supervisor I know I would be counselled to get used to feeling behind.' |
|
'The culture in Child Protection is such that the workload is so high, that taking time off for rest or as a mental health day is faced with a heavier workload when you return to work. This sometimes requires you to gain further TIL which in turn is not taken as the cycle would only continue.' |
Support (generally)
|
'I have not felt supported in my role and a few contributing factors which have affected my wellbeing … no information was given about “in/outs/conventions” of role—a welcome pack would have been very helpful.' 'It is understandable that staff are busy, yet first day back from completing Beginning Practice training, it would have helped to have a structured conversation about my nine clients, and the next steps of where to go.' 'There is a culture of “just ask questions”—as a beginning CPP, there is a lot of information to process and sometimes you don't know what questions to ask.' |
|
'Often I see workers self-medicating to deal with vicarious trauma—mostly with alcohol in order to relax, sleep and reduce anxiety.' 'Many workers will claim sick days for physical conditions, when the issues relate to their mental health, as they are concerned about being judged and their capacity as workers questioned. This issue is further exacerbated by:
|
|
'I am finding I do not want to come to work and that does not happen for me. I am tired all the time and feel that we keep talking about the issues, giving lots of easy quick solutions to some of these areas and nothing happens or changes.' |
|
'It is felt that Child Protection is just a difficult job so if you say that you're not coping you get labelled as not being able to do the job so people are afraid to speak up as they feel it may prevent them from progressing as this has happened to people previously.' 'At present I do not feel valued or supported as an individual or as a team. I feel like I cannot speak up as I just get shot down and that has prevented me from being successful in roles I have previously demonstrated I am more than capable of doing … I am currently looking at options outside of the Department as I am unable to work in such a negative environment.' |
|
'Supports such as IT, office maintenance, payroll, human resources, and placement coordination are all located in larger metro areas and are not easily accessible to us. I.e. if you have an IT issue sometimes you are required to wait until an IT worker is scheduled to attend the office to rectify the problem … It is also my experience that if you are mentally unwell, i.e. experiencing depression, stress or just not coping, there is no support provided by the organisation unless you have a WorkCover claim in place.' |
|
'The opinion was “if you can't hack it leave”.' |
|
'Think that Child Protection program significantly under-report incidents of abuse that impact on individual's wellbeing. Data from DINMAs etc. would not be a true reflection of the incidents' occurrence.' |
