Palliative Care
Overview
Palliative care aims to improve the quality of life of people with terminal illnesses by managing pain and distressing symptoms. With the population ageing and the need for palliative care on the rise, health services face increasing pressure to manage the often complex needs of patients, their carers and families, often in home settings.
This audit assessed whether Victorians with a terminal illness have access to high‑quality palliative care that is timely, coordinated, and responsive to their needs and wishes. The audit examined the policies and procedures of the Department of Health & Human Services (DHHS) and four health services.
The audit found that DHHS has set a clear and ambitious agenda for the palliative care sector but there is room for improvement. In recent years access to services has improved. However some metropolitan community-based services are struggling to cope with demand.
Greater focus is also needed on supporting carers and families. While there have been improvements in areas such as after-hours support for carers and families, further work is needed to ensure carers and families can access support at critical times. In particular, respite provision and access to psychosocial support remain major priorities.
Palliative Care: Message
Ordered to be published
VICTORIAN GOVERNMENT PRINTER April 2015
PP No 28, Session 2014–15
President
Legislative Council
Parliament House
Melbourne
Speaker
Legislative Assembly
Parliament House
Melbourne
Dear Presiding Officers
Under the provisions of section 16AB of the Audit Act 1994, I transmit my report on the audit Palliative Care.
This audit assessed whether Victorians with a terminal illness have access to high-quality palliative care that is timely, coordinated and responsive to their needs and wishes. The audit examined the policies and procedures of the Department of Health & Human Services (DHHS) and four health services.
The audit found that despite establishing a clear and ambitious agenda for the palliative care sector, DHHS has more work to do to streamline its monitoring and reporting processes to better understand gaps and achievements. In recent years, access to rural and after-hours services has improved. However, some metropolitan community palliative care services are struggling to cope with demand and more support is needed for carers and families.
DHHS has a major role to play in guiding the sector through a period of continued change and growth. My audit findings and recommendations will help DHHS and health services to build on recent achievements and respond to future challenges with a flexible and efficient palliative care system.
Yours faithfully
John Doyle
Auditor-General
15 April 2015
Auditor-General's comments
 John Doyle Auditor-General |
Audit team Kris Waring—Engagement Leader Caitlin Makin—Team Leader Emily Arthur—Analyst Engagement Quality Control Reviewer Michele Lonsdale |
Death and dying can be a confronting prospect for anyone with a terminal illness. Understanding your prognosis, finding out what options exist and deciding what kind of care you would prefer can be complex and emotional. Families, friends and carers can also be overwhelmed with decisions as they attempt to access services and support their loved ones. Making this process as straightforward and responsive to a patient's needs and symptoms as possible is what good palliative care is about.
The Department of Health & Human Services (DHHS) first developed a palliative care strategy in 2004 and refreshed it in 2011 with the Strengthening palliative care: Policy and strategic directions 2011–2015 (Strategic Directions). However, as palliative care continues to develop and becomes more widely understood and valued, demands on health services and community palliative care organisations are changing and escalating.
Advance care plans (ACP) are one of the central pillars of palliative care—helping patients to set out their personal decisions and preferences, and assisting palliative care staff and other health care professionals to make well-informed decisions. DHHS's new strategy—Advance care planning; have the conversation: A strategy for Victorian health services 2014–2018—places renewed focus on all parts of the health service to consistently adopt and communicate ACPs.
In this audit I looked at whether Victorians with a terminal illness have access to high-quality palliative care that is timely, coordinated and responsive to their needs and wishes.
I found that palliative care in Victoria is delivered by skilled and dedicated staff who specialise in caring for people with a terminal illness. Indeed, Victoria has a strong palliative care sector and DHHS has set a clear and ambitious agenda for what remains a relatively new area of health provision. However, a number of areas for further improvement remain.
Demand for home-based care is increasing and some metropolitan community palliative care services have struggled to meet this demand, resulting in waiting lists to access services. This can place additional stress on patients and carers, and can mean that some people who have chosen to die at home cannot spend their last days there. DHHS has committed to better forecasting demand for services and to work with palliative care services to better understand how to support carer needs and respond to unmet demand.
More also needs to be done to support carers and families. While there has been progress in some areas, improving respite provision and access to psychosocial support remain major priorities. Notably, 'support for carers' and 'engaging with the community' were two key priorities of DHHS's Strategic Directions that have not been met.
Going forward, it is imperative that DHHS sets clear expectations for service delivery across the state and provides sufficient and appropriate funding to health services and community organisations.
The majority of palliative care takes place in patient homes, provided by community palliative care services. However, the provisions of the Audit Act 1994 limited the extent to which we could assess non-government community palliative care, despite a Parliamentary inquiry recommending changes to the Act over four-years ago. I hope that promised changes to my mandate to introduce follow‑the‑dollar powers will enable me in future to provide Parliament and the public with greater assurance that palliative care services being delivered by non‑government and community organisations are effective.
I have made 12 recommendations to address the major issues identified in the audit. DHHS has accepted all recommendations and included an action plan detailing how it intends to address them. I will also follow up separately with all health services in Victoria who provide palliative care services to ensure that they act on my recommendations where appropriate.
I am particularly pleased with the constructive and considered way in which DHHS and audited health services approached the audit and assisted my staff to complete their work. I wish to thank them and their staff for their time, and for their ongoing commitment to patients in their care.
John Doyle
Auditor-General
April 2015
Audit Summary
About 36 000 people die in Victoria each year and this figure is projected to double in the next 25 years. Of those people, about half will die following a period of chronic illness such as heart disease, cancer, stroke or neurological illness—it is these people who will most benefit from palliative care. Palliative care aims to improve the quality of life of people with terminal illnesses by managing pain and distressing symptoms, and assisting patients to start making choices about how they want to be cared for as they die.
Victoria upholds the World Health Organisation's definition of palliative care—that it intends neither to hasten nor postpone death. Palliative care is delivered through a range of community, inpatient and consultancy services. Coordinating care for patients as they transition through these services requires systems that are integrated and staff that are skilled in communication and patient-centred care.
Palliative care services are largely funded by the Department of Health & Human Services (DHHS) and are administered by a range of public, private and non‑government providers. The majority of palliative care services are provided to people in community settings—home or home-like settings—by non-government providers.
With the population ageing and the need for palliative care on the rise, health services and community palliative care organisations face increasing pressure to manage the often complex needs of patients, their carers and families. There is also a shift in preference for palliative care to be provided in the home.
DHHS has an important role to guide and prepare the sector for these coming challenges. Its Strengthening palliative care: Policy and strategic directions 2011–2015 (Strategic Directions) identified seven strategic directions and 23 associated priorities that aim to provide a comprehensive and well-coordinated palliative care service to Victorians.
This audit assessed whether Victorians with a terminal illness have access to high‑quality palliative care that is timely, coordinated and responsive to their needs and wishes. The audit reviewed DHHS' Strategic Directions and guidance and assessed care in four public palliative care services:
- Two were inpatient‑only services.
- One had an inpatient service and a non-government community-based service.
- One had public inpatient and community-based services.
This audit was commenced under the Department of Health. On 1 January 2015, machinery-of-government changes took effect and the responsibilities of the former Department of Health transferred to DHHS.
While we consulted non-government community palliative care services as part of this audit, and they willingly contributed their time to broaden our understanding of the sector, the provisions of the Audit Act 1994 limited the extent to which we could assess non‑government community palliative care.
Conclusions
Victoria is a leader in palliative care provision in Australia and DHHS has set a clear and ambitious agenda for the palliative care sector. Palliative care is delivered by dedicated staff who coordinate across health services to make caring for people with a terminal illness as seamless and responsive as possible. However, as a relatively new area of health provision there is still considerable room for improvement.
DHHS first developed a palliative care policy in 2004 and further clarified the priorities in 2011 in its Strategic Directions. However, progress in some areas has been slow and problems with its performance monitoring framework make it difficult for DHHS to meaningfully track and report on how effectively its Strategic Directions have been implemented.
As palliative care takes on greater importance and is more widely understood and valued, demands on health services and community palliative care organisations are escalating. The community sector and inpatient hospital services are having to become more agile and coordinated to accommodate people's wishes, particularly where their final wish is to die comfortably at home.
Patients should be supported to die in their place of choice, be that in hospital or in their home. The provision of palliative care services at home is more cost-effective than in hospital. However, some metropolitan community palliative care services are struggling to cope with increasing demand. This means that some patients are not able to access services in their home and this, combined with increasing stress on carers at the end of life, can result in people spending their last days in their less preferred and more expensive hospital setting.
Health services are developing better systems to identify and manage palliative care patients including making wider use of advance care plans (ACP)—a patient's documented end-of-life preferences. However, the pace of change across health services is difficult to track. Audited health services made some pleasing but variable progress in the past 12 months. As ACPs are one of the central pillars of effective palliative care, more needs to be done to promote and embed them across the health system.
There is also more that could be done for carers and families. While there have been improvements in areas such as after-hours support for carers and families, further work is needed to ensure carers and families can access support at critical times. In particular, respite provision and access to psychosocial support remain major priorities.
DHHS has a major role to play in guiding the sector through this transitional period. It is imperative that it provides sufficient and appropriate funding to health services and community palliative care organisations. DHHS should set clear expectations for service delivery across the state, so that the palliative care sector can build on its achievements and respond to future challenges with a flexible and efficient palliative care system.
Findings
Policy framework and performance monitoring
DHHS' Strategic Directions is the product of in-depth consultation and provides health services with a sound policy and implementation strategy. DHHS' initial consultation on a successor strategy reveals that many in the sector are ready to aim higher and increasingly focus on patient-centred outcomes.
The Strategic Directions helped set the palliative care sector on an ambitious trajectory and has made some notable achievements, including:
- expanded consultation services for regional Victoria
- better access to after-hours support
- additional funding to build and upskill the workforce.
However, some goals will not be met because they were designed without due regard for the complexity and time needed to affect real change.
DHHS' current monitoring framework is overly complex and not fit for purpose. Some activities cannot be tracked because reporting mechanisms are not adequately developed to measure progress. It contains 314 key performance indicators yet fails to give a clear indication of the impact of activities.
This limits DHHS' ability to provide assurance that the sector is on track and that its strategy has been fully implemented. It also means that health services cannot understand how they perform at a system level. DHHS has committed to streamline its future monitoring framework and further develop existing reporting systems.
As well as fixing its monitoring framework, DHHS needs to improve its communication with health services and community palliative care providers about its reporting requirements. This would help them to understand how their information is used and have a better sense of their comparative achievements and weaknesses. This would enable DHHS to drive change at both the system‑wide and local level.
Support for carers
Audited health services consistently reported that carers' access to respite is inadequate. Some services are concerned that carers, who are likely to have significant needs after the death of their loved ones, are not adequately assessed or screened and therefore may not be linked to counselling and bereavement services.
There is scope for health services to make better use of DHHS' Bereavement support standards for specialist palliative care services to screen individuals at risk of complicated grief and provide appropriate bereavement support.
Families and carers of palliative patients shoulder enormous responsibilities and psychological stress, particularly as more people elect to die at home. For some families there are also financial pressures associated with withdrawing from the workforce for an unknown length of time to support their loved one.
DHHS needs to work closely with carers and the palliative care sector to provide better support options for carers. In addition, DHHS also needs to further research the effectiveness of bereavement services so that it is extended to those who need it.
Awareness of palliative care and advance care planning
DHHS has a number of initiatives aimed at increasing awareness of palliative care in culturally diverse communities. Progress is slow but on the right path—DHHS needs to continue to invest in making palliative care accessible and inclusive for all.
ACPs enable people who are dying to communicate their preferences and to have the choices they make about their care respected and carried out. Research shows that families and carers of people who have ACPs suffer less anxiety and grief. Reporting on ACP implementation is poor, but available data shows that only half of the patients being supported by community palliative care providers have ACPs in place. DHHS needs to look at ways to improve reporting so that it can better understand if inpatient services are using and promoting this vital tool.
Coordination and referrals
Coordinating patient care across palliative care settings is hindered by lack of access to integrated patient management systems—an issue that affects a range of health programs beyond palliative care. Some services would also benefit from greater investment in systems to manage internal electronic files.
Audited palliative care inpatient services have well-documented admission and referral systems and most meet the national benchmark for timely admission. However, routine audits would provide greater assurance that admission and referral processes are timely and appropriate.
Demand for services
DHHS promotes the right for people to choose where they wish to die. However, the resource-constrained community palliative care sector in metropolitan Melbourne is already struggling to keep up with demand. Audited health services in metropolitan areas are concerned that their patients are not always able to access palliative care at home in a timely way. For patients who have limited or no access to a carer this is a particularly daunting prospect.
There is a risk that patients discharged home will have to wait to access care in the home. DHHS needs to plan for growth and guide the sector to meet current and growing demand. It has allocated funding to the Centre for Palliative Care to develop a triage tool intended to ensure that patients with the most urgent needs are able to access palliative care in a timely way. Smaller, regionally‑based services need a clearer understanding of how to deliver or facilitate access to a range of allied health and psychosocial services so that their communities are not disadvantaged.
DHHS is developing a tool to understand gaps in services and plans to use it to assist with forecasting and future service planning. To complement this work there should be a statewide approach that encourages each region to work together to ensure all terminally ill people can access services. This tool needs to assist the sector to meet rising demand for services.
Recommendations
That the Department of Health & Human Services:
- reviews service provision as a priority to understand gaps in the system, better forecast demand and inform future service planning
- develops a robust policy evaluation method to monitor the implementation and outcomes of its new end-of-life care framework
- closely monitors health services' reporting on palliative care and follows up with health services when non‑compliance is identified so that all required reporting is completed and can be analysed and communicated back to services.
That health services:
- conduct regular audits of patient files to understand if referrals and admissions to palliative care were managed in a timely and appropriate manner
- prioritise integrating patient data systems and improve information sharing options for communicating with community palliative care services
- prioritise the implementation of advance care planning and comply with the Department of Health & Human Services' data collection and reporting requirements.
That the Department of Health & Human Services and health services work together to:
- understand barriers to accessing care, understand and respond to unmet demand, and engage communities who do not traditionally access palliative care
- provide patients and carers with more support to understand what services are available and how to access them when they need them.
That the Department of Health & Human Services:
- conducts a systematic review of respite and carer support provision
- develops clear expectations for health services to appropriately support carers including providing practical information on patient care and advice or referral as appropriate for emotional and bereavement needs
- reviews system-wide palliative care performance measures to improve how hospitals and palliative care services document and deliver patient- and carer-focused services
- reviews and improves the after-hours model for community palliative care services across Victoria.
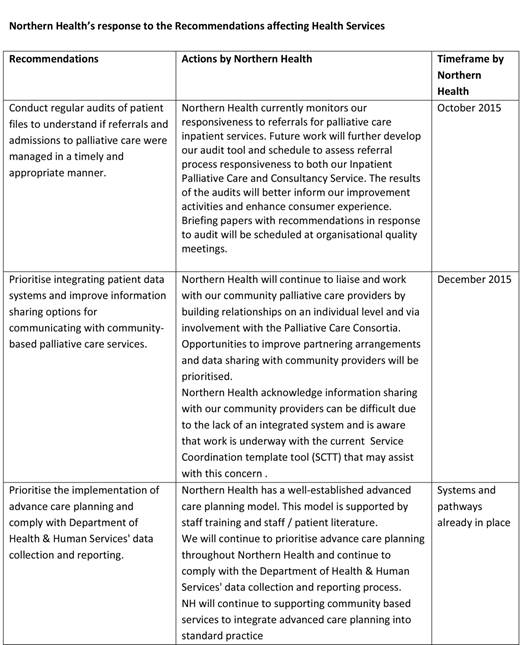
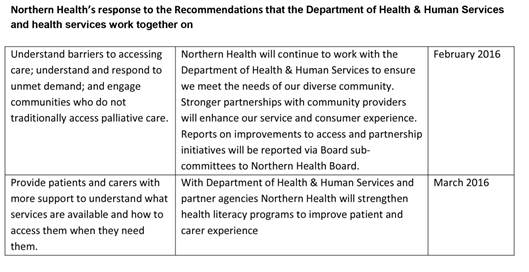
Submissions and comments received
We have professionally engaged with the Department of Health & Human Services, St Vincent's Hospital Melbourne (including Caritas Christi Hospice), Northern Health, Mercy Health (Werribee Campus) and Central Gippsland Health Service throughout the course of the audit. In accordance with section 16(3) of the Audit Act 1994 we provided a copy of this report, or relevant extracts to those agencies and requested their submissions or comments.
We have considered those views in reaching our audit conclusions and have represented them to the extent relevant and warranted. Their full section 16(3) submissions and comments are included in Appendix A.
1 Background
1.1 Introduction
The end of a person's life is always going to be difficult for them and their families. However, with the right planning, care and support, death can be made easier on all involved. Palliative care is delivered by a range of healthcare professionals and provides this type of support.
Around half of all Victorians who die each year would benefit from palliative care. Traditionally, people diagnosed with terminal cancer have represented the majority of palliative care patients. However, people with other chronic illnesses—such as motor neurone disease, HIV/AIDS, end-stage heart, lung or kidney disease, and advanced dementia—are increasingly accessing palliative care. Early referral to palliative care services can help people begin making decisions about the type of care they want.
Palliative care is different to curative treatment, but they can be provided alongside each other. While curative treatment is aimed at prolonging life, palliative care is aimed at improving the quality of life. Palliative care can be provided in an inpatient hospital setting or within the community, at a person's home, aged care facility or disability group home. In community-based settings, patients and their carers can also access after‑hours telephone support. Palliative care staff are trained to work with families, carers and patients to understand where the patient would like to die and the treatment they would prefer.
In 2013, the Australian Bureau of Statistics (ABS) conducted analysis of population trends in Australia. Its analysis shows that the Australian population is ageing and growing. It predicts that 19 per cent of the population will be aged over 65 by 2033 if current trends continue.
Similarly, the ABS predicts that in Victoria the median age of the population will increase significantly over the next 40 years—in 2012, the median age was 37.3 years and the ABS forecasts that it will increase to 39.5 years by 2013 and 42.4 years by 2061. This growth in the aged population will increase the need for palliative care services.
1.2 Palliative care service provision in Victoria
Palliative care is delivered through community, inpatient and consultancy services, administered by public, private and non-government providers:
- Consultancy services provide symptom management and discharge planning for patients in acute hospital wards and outpatient services for community palliative care services.
- Community palliative care services provide in-home and after-hours services to manage symptoms and provide end-of-life care.
- Inpatient palliative care wards provide symptom management, end-of-life care, discharge planning and respite. They also provide care aimed at controlling unstable or deteriorating symptoms. Inpatient staff also prepare patients and carers for the transition home where possible.
Figure 1A
Palliative care service map
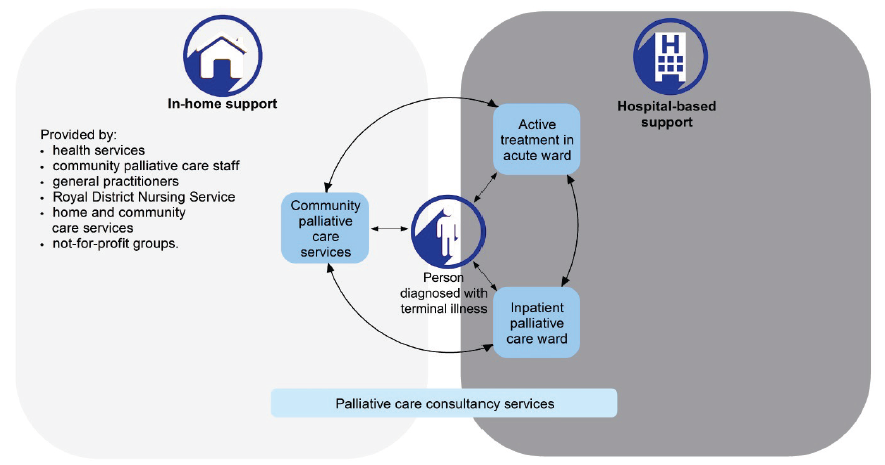
Source: Victorian Auditor-General's Office.
The majority of care occurs in community-based settings and is delivered by non‑government providers. Public and non-government community palliative care services also link with other services to provide palliative care in the patient's home:
- Royal District Nursing Service—contracted by some community palliative care services to provide after-hours nursing support.
- Home and community care services—provide basic support to people over 65 who live at home.
- Not-for-profit support groups and volunteers—may assist by providing meals for patients or transport to medical appointments.
Volunteers are also an essential part of the palliative care sector. A Department of Health & Human Services (DHHS) workforce study released in 2013 reported that the number of hours volunteers work in palliative care is equivalent to 30 per cent of paid full‑time employees. Further, it identified that in-home support was the main role undertaken by volunteers.
Patients move between different levels and places of care depending on the progression of their illness and their needs at each stage. There is no standard pathway that patients follow—rather their care should cater to their prognosis and personal needs and wishes. Figure 1B is a fictional example of one person's pathway through palliative care services.
Figure 1B
A journey through palliative care services
|
Mrs H is diagnosed with end-stage pancreatic cancer at the oncology ward of Hospital A. A consult team specialising in palliative care visits the oncology staff to discuss Mrs H's symptoms and needs and suggests a change in pain medication. A meeting is held with the treating specialist, a social worker and Mrs H's adult son and daughter. The daughter lives two hours away and has difficulty visiting more than once or twice a week. The son lives close-by but is worried his employer will not be happy if he takes a lot of time off work. He is also anxious that he does not know how to properly care for his mother. The following day the palliative care team held their weekly meeting to discuss newly admitted patients. Mrs H's pain symptoms are under control but she needs physical therapy. The physiotherapist arranges time to visit her. The social worker advises that he has provided some information about financial support for carers to the son, and suggests staff contact him to provide more information about what to expect in preparation for her discharge home. Staff agree that due to the family's financial circumstances they should seek funding to help with the cost of equipment that will be needed in the home. The next week Mrs H is in a stable condition and ready to be discharged home. She understands that she has only a few weeks left to live and told staff she prefers to die at home, if it is not too much of a burden for her family. Hospital staff brief the local community palliative care service on Mrs H's situation. It agrees to take on Mrs H as a client and plans for nursing staff to visit within five days of her discharge. Hospital staff arrange for a community worker to visit once a week to clean the house. The son draws up a care roster with his aunt, a neighbour and his sister. This makes him feel more at ease. Six weeks later, the community service nurse advises the son that Mrs H is likely to die soon. He calls his sister and two days later Mrs H dies peacefully at home with her family. |
Source: Victorian Auditor-General's Office.

1.2.1 Regional consortia
In 2004, DHHS set up eight palliative care regional consortia across the state to:
- undertake regional planning in line with departmental directions
- coordinate palliative care service provision in each region
- advise the department about regional priorities for future service development and funding in conjunction with the Palliative Care Clinical Network.
Palliative care consortia comprise members from all funded palliative care services in each region, as well as other health, community and aged care providers.
1.2.2 Funding
Under a devolved governance model, DHHS is responsible for devising policy and guidance for the sector, setting targets, providing funding and determining service priorities for public hospitals and other public health services. In return, these agencies provide a range of services to the public.
Inpatient palliative care is funded using an activity based funding model, which was introduced in the 2013–14 financial year. This funding approach applies daily payments weighted on the patients' phase of care—stable, unstable, deteriorating and terminal—during their hospital stay.
Formerly, palliative care bed-based activity was funded on a daily basis. The daily rate was higher for rural in-patient palliative care activity. In-patient services received block funding, where a price was assigned according to hospital size and geographic location, and whether the patient was in an acute, sub-acute or mental health ward. Smaller rural services attracted additional funds.
Community palliative care services are block funded. Base funding for community palliative care was determined from a 1998 tender process. In 2005 and 2011 additional growth funding was allocated using the Palliative Care Resource Allocation Model that includes a weighted population formula. Figure 1C shows that in 2013–14 DHHS' funding for palliative care provision was approximately $111.1 million.
Figure 1C
Funding for palliative care services, 2013–14
|
Service |
Budget ($ million) |
|---|---|
|
Inpatient services (bed-based and consultancy teams) |
56.8 |
|
Community palliative care services (home-based care, day hospices, flexible funding) |
39.4 |
|
Consultancy services (to hospitals and health services) |
10.3 |
|
Research, education and training |
3.5 |
|
Regional palliative care consortia |
1.1 |
|
Total |
111.1 |
Source: Victorian Auditor-General's Office based on information provided by DHHS.
1.2.3 Cost of dying
The Grattan Institute's 2014 report Dying well reported on palliative care in Australia. It projected that health and social care costs associated with dying will likely double to more than $10 billion a year in the next 25 years as the crude death rate increases. It also found that the cost of dying in hospitals and aged care facilities far exceeds the cost of dying at home, supported by community palliative care services. Figure 1D shows the relative cost of dying in different settings.
Figure 1D
Place and costs of death for older people in 2012
|
Place of death |
Deaths (number) |
Deaths (per cent) |
Costs ($ million) |
Costs (per cent) |
|---|---|---|---|---|
|
Acute inpatient(a) |
51 759 |
35 |
2 440 |
48 |
|
Sub-acute inpatient(b) |
21 470 |
15 |
221 |
4 |
|
Residential care |
50 866 |
35 |
2 330 |
46 |
|
Community-based care |
4 655 |
3 |
77 |
2 |
|
Other(c) |
18 182 |
12 |
– |
– |
|
Total |
146 932 |
100 |
5 066 |
100 |
(a) Acute—urgent inpatient care often through emergency admission that may require a short stay.
(b) Sub-acute—extended inpatient care that can include geriatric, rehabilitation and mental health care.
(c) Other—includes deaths that occurred outside hospital, group home or community-based care settings.
Note: Totals may vary due to rounding.
Source: Victorian Auditor-General's Office from Dying well, Grattan Institute, 2014.
1.3 Policy and legislative framework
1.3.1 Strengthening palliative care: Policy and strategic directions 2011–2015
DHHS' Strengthening palliative care: Policy and strategic directions 2011–2015 (Strategic Directions) identifies seven strategic directions and 23 associated priorities to provide comprehensive and well-coordinated palliative care services to Victoria. These are set out in Figure 1E.
Figure 1E
DHHS' Strategic Directions, 2011–15
|
Strategic direction |
Priorities |
|---|---|
|
Informing and involving clients and carers |
|
|
Caring for carers |
|
|
Working together to ensure people die in their place of choice |
|
|
Providing specialist palliative care when and where it is needed |
|
|
Coordinating care across settings |
|
|
Providing quality care supported by evidence |
|
|
Ensuring support from communities |
|
Source: Victorian Auditor-General's Office based on information provided by DHHS.
DHHS has implemented a number of other relevant policies and standards, including:
- Strengthening care for children with a life-threatening condition (2008)
- After-hours palliative care framework (2012)
- Bereavement support standards for specialist palliative care services (2012)
- Advance care planning; have the conversation: A strategy for Victorian health services 2014–2018 (2014).
1.3.2 National Palliative Care Strategy 2010
The National Palliative Care Strategy 2010 (NPCS) aims to inform policy and service development across Australia, and guide states and territories in planning for the development of palliative care services. NPCS identifies four goal areas and associated actions:
- 'Awareness and Understanding
- Appropriateness and Effectiveness
- Leadership and Governance
- Capacity and Capability'.
1.3.3 Palliative care patient data
DHHS collects a wide range of palliative care data from health services and community palliative care organisations. This data is a combination of mandatory and voluntary reporting and participation levels vary. This means that some of the information is more reliable than other information. Figure 1F sets out the key data collection methods.
Figure 1F
Palliative care data collection
|
Dataset |
Compulsory/ |
Information collected |
Health services |
|---|---|---|---|
|
Victorian Admitted Episodes Dataset |
Compulsory |
Clinical and administrative data, such as:
|
|
|
Victorian Integrated Non‑Admitted Health minimum dataset |
Compulsory |
Clinical and administrative data, as well as patient-centred data such as:
|
|
|
Policy Implementation Audit Tool |
Compulsory |
Survey data on policy implementation, such as:
|
|
|
Palliative Care Outcomes Collaboration |
Voluntary |
National benchmarking data related to patient outcomes, such as:
|
|
|
National Standards Assessment Program |
Voluntary |
Accreditation against national quality improvement standards including:
|
|
|
Victorian Palliative Care Satisfaction Survey |
Compulsory for health services to provide to patients and carers, whose response is optional |
Survey responses on palliative care services including satisfaction with:
|
|
Source: Victorian Auditor-General's Office.
1.4 Previous audit coverage
The 2012 VAGO report, Carer Support Programs, included carers involved in palliative care. The audit assessed the extent to which the former Department of Health, now DHHS, was effective in recognising and supporting people who care for others. It made five recommendations, all of which DHHS accepted. This included that DHHS:
- identifies and addresses gaps in the promotion of carer supports to improve carer awareness of services
- requires consistent carer identification and needs assessment
- improves administration and monitoring of carer brokerage funds
- monitor and reports on timeliness of access to carer supports
- develops outcome measures for carer supports and monitor outcomes.
In February 2015, the Auditor-General released the audit report Responses to 2012–13 Performance Audit Recommendations, which determined the extent of agency response to, and monitoring of, VAGO performance audit recommendations from 2012–13 audits. DHHS advised it has completed four of the five recommendations outlined in the Carer Support Programs audit. The first recommendation—to identify and address gaps in the promotion of carer supports to improve carer awareness of services—is still in progress. DHHS expects to complete it by June 2015.
In 2012 DHHS outlined that it would address this recommendation by requiring palliative care services to self-assess against national palliative care standards, as Standard Five includes quality elements in relation to carers. DHHS developed a Victorian service delivery framework for palliative care services to self-assess against, which includes assessment against the national standards. Part 2 of this report discusses the challenges associated with this framework in more detail.
1.5 Audit objectives and scope
The objective of the audit was to determine whether Victorians with a terminal illness have access to high-quality palliative care that is timely, coordinated and responsive to their needs and wishes.
To test this, the audit examined whether:
- DHHS' Strategic Directions has equipped health services in Victoria to efficiently meet growing demand for palliative care
- health services have effective planning and strategies to meet palliative care patients' needs and preferences
- health services work together to provide comprehensive and coordinated support for admitted and non-admitted palliative care patients and their carers.
This audit was commenced under the Department of Health. On 1 January 2015, machinery-of-government changes took effect and the responsibilities of the former Department of Health transferred to DHHS.
The audit included DHHS and four out of 59 public health services providing palliative care—St Vincent's Hospital Melbourne (including Caritas Christi Hospice), Northern Health, Mercy Health (Werribee Campus) and Central Gippsland Health Service. They were selected to provide a cross-section of different types of service in different socio‑demographic and geographic areas.
While we consulted non-government community palliative care services as part of this audit and they willingly contributed their time to broaden our understanding of the sector, the provisions of the Audit Act 1994 limited the extent to which we could assess non‑government community palliative care.
The audit did not consider services provided by general practitioners and residential aged care services. These are the responsibility of the Commonwealth Government.
1.6 Audit method and cost
The audit method involved:
- assessment of DHHS' policies, strategies, guidance, evaluation and assessment tools to support health services to diagnose, refer and care for palliative care patients
- assessment of the Victorian Palliative Care Satisfaction Survey
- analysis of DHHS data on public and community health services' key performance data
- analysis of health services' evaluation tools and patient data to understand referrals and documentation of patient choices
- assessment of health services' triage systems and waiting lists
- interviews with DHHS staff
- interviews with generalist and specialist staff from health services across the sector
- feedback from a community-based palliative care forum and a community visitors' forum—community visitors are responsible for monitoring disability group homes.
The audit was conducted in accordance with section 15 of the Audit Act 1994 and Australian Auditing and Assurance Standards. Pursuant to section 20(3) of the Audit Act 1994, unless otherwise indicated, any persons named in this report are not the subject of adverse comment or opinion.
The total cost of this audit was $375 000.
1.7 Structure of the report
This report is structured as follows:
2 Palliative care policy and planning
At a glance
Background
The Department of Health & Human Services (DHHS) released its second palliative care policy in 2011—Strengthening palliative care: Policy and strategic directions 2011–2015 (Strategic Directions). Palliative inpatient services work with other hospital wards and community palliative care services to coordinate patient care.
Conclusion
DHHS' Strategic Directions set ambitious goals for the sector. While these goals addressed the right issues, DHHS failed to appreciate the complexity and time required to implement some goals. Around 20 per cent of initiatives are unlikely to be completed on time and others require ongoing investment. A new refreshed policy is needed to advance and refocus this work. DHHS needs to set clear expectations for service delivery, monitor compliance with its requirements, develop measurable indicators and appropriately fund and support providers.
Findings
- Eighty per cent of DHHS' Strategic Direction actions have been completed.
- DHHS' monitoring framework for palliative care is unwieldy. It is burdensome and cannot track some activities, particularly in the community.
- Some terminally ill patients cannot access timely community-based support.
Recommendations
That the Department of Health & Human Services:
- reviews service provision to understand system gaps and inform planning
- develops a robust evaluation method to monitor its new framework
- closely monitors reporting on palliative care and intervenes when necessary.
That health services:
- conduct regular audits of patient files to understand if referrals and admissions to palliative care were managed in a timely and appropriate manner
- prioritise integrating patient data systems and improve information sharing.
2.1 Introduction
The Department of Health & Human Services (DHHS) released its first palliative care policy in 2004. It focused on developing skills and building awareness of palliative care across health settings, and emphasised providing timely, appropriate and coordinated care, and increased support for carers.
In 2011, DHHS released a successor policy—Strengthening palliative care: Policy and strategic directions 2011–2015 (Strategic Directions). The Strategic Directions extended the still relevant principles and introduced a new implementation plan to further develop palliative care services. An internal monitoring framework was developed to track progress of the policy and implementation plan.
This Part examines how effectively DHHS has implemented its Strategic Directions, including monitoring and reporting practices, coordination and collaboration between health services, and planning for future growth. It also considers the role of regional consortia.
2.2 Conclusion
The Strategic Directions set ambitious but relevant goals for palliative care. However, these targets were set without due regard for the complexity or the time needed to effect change. A number of its goals will not be met by the end of 2015. These relate to supporting carers, building community awareness of palliative care and taking steps to enable people to die in their place of choice. Arguably, these are some of the more challenging objectives in the Strategic Directions.
The Strategic Directions include 314 key performance indicators (KPI). This is a very large number of indicators for a program area of this size and it is a significant reporting burden on DHHS, health services and community palliative care organisations. The KPIs are further undermined by some poor quality evidentiary sources. Ultimately, this makes it difficult for DHHS to meaningfully track and report on the implementation or effectiveness of its Strategic Directions.
Demand for palliative care is growing as the population ages and people endure increasingly lengthy periods of chronic illness, sometimes with more than one disease. Further, as awareness of palliative care options grows, the number of those who elect to die at home or home-like settings—aged care facilities and disability group homes—is increasing.
These trends are shifting pressure from the palliative inpatient care system on to community palliative care services. This in turn is presenting new challenges, increasing the need for different services to work in increasingly joined-up, collaborative ways. This pressure is starting to result in patients in Melbourne having difficulty accessing appropriate community palliative care services on discharge from hospital.
DHHS plays an important role in guiding the sector. This will only increase as palliative care services try to adapt their service models to become more flexible and patient‑centred and provide the type of service required for a modern and effective palliative care system. It is important that DHHS sets clear and realistic expectations for service delivery across the state, provides sufficient and appropriate funding to health services and community palliative care organisations, and monitors compliance with reporting requirements.
2.3 Strengthening palliative care: Policy and strategic directions 2011–2015
Audited health services and other stakeholders advised that DHHS has consulted well on palliative care. They agreed that its Strategic Directions appropriately reflected the gaps and needs of the sector at the time. However, patient needs and expectations are changing and while some goals are still relevant, not all have been fully implemented.
The strategy is now in its fifth year and DHHS' evaluations indicate that 80 per cent of its action items have been addressed. It has not yet realised the outcomes of some ongoing actions. While the majority of actions are completed, DHHS will fall short of achieving the intended outcomes for strategic direction 2—Caring for carers. Similarly, further work is required to fully address strategic directions 3 and 7:
- Strategic direction 2: Caring for carers—while some important activities have been completed—such as the after-hours telephone triage service for patients and carers in community-based palliative care—these activities do not fully address complex carer needs. DHHS provided evidence of continued research on carer respite needs and advised that it plans to consult with the sector on priorities for carers to inform more feasible support options. Carer respite remains a high priority for DHHS and the sector and is discussed in greater detail in Part4.
- Strategic direction 3: Working together to ensure people die in their place of choice—slightly more community-based palliative care clients died in their preferred place of choice in 2012–13 (64 per cent) compared with 2009–10 (61 per cent). However, despite some initial progress with this important yet challenging goal, it will require sustained effort:
- training staff to have difficult conversations
- encouraging patients to consider advance care plans—discussed in Part 3
- linking to services that can respond.
- Strategic direction 7: Ensuring support from communities—this direction aims to raise community awareness of palliative care, particularly in culturally diverse communities and rural areas. In 2013–14, DHHS commissioned a culturally responsive community awareness project to begin working in Chinese, Italian, Maltese, Turkish and Vietnamese communities. While positive, this did not commence until the third year of the Strategic Directions. An earlier start would have allowed greater progress to be made as awareness raising and behaviour change takes time. DHHS needs to build on this work to ensure members of communities who don't traditionally access palliative care services have the knowledge and opportunity to access palliative care, and are supported by interpreters and culturally competent health staff. These projects are discussed further in Part3.
2.4 Monitoring and reporting
DHHS collects and uses a wide range of palliative care data. However, some of this data is of poor quality and provides limited information. Some services do not routinely submit the required data and DHHS has acknowledged that its monitoring system for palliative care has shortcomings. It has committed to develop and use a simplified model for its new policy framework. However, considerable work remains to develop comprehensive high-quality and relevant palliative care data sets.
2.4.1 Reporting against the Strategic Directions
The evaluation matrix for DHHS' Strategic Directions is overly complicated. Weaknesses in the evidence sources and the sheer number of KPIs make it difficult for DHHS to track activities—particularly around community provision—and report meaningfully on performance and progress. It includes 314 KPIs including some where:
- the source data cannot be identified
- the measure does not directly link to intended impacts and outcomes
- there is missing and duplicated information.
There is a risk that these data problems mask real progress, or result in DHHS missing important issues.
DHHS does not report publically on its progress against each KPI. Instead it produces an annual thematic report on the implementation of the policy. This allows it to communicate the major achievements to the sector in an accessible format, however, it limits the report's usefulness. While each report provides important information, the current approach is at the expense of systematic, comprehensive reporting. This reduces the capacity of the reports to demonstrate changing palliative care activities and outcomes over time. Consequently, each report exists as a stand-alone document rather than a report in a longitudinal series. It also limits the ability of the palliative care sector to understand gaps and challenges in implementation progress.
2.4.2 Palliative care reporting
DHHS draws on five main datasets to inform itself about palliative care activity and outcomes:
- Victorian Admitted Episodes Dataset (VAED)
- Victorian Integrated Non-Admitted Health (VINAH) minimum dataset
- Policy Implementation Audit Tool (PIAT)
- Palliative Care Outcomes Collaboration (PCOC)
- Victorian Palliative Care Satisfaction Survey (VPCSS)
Where possible throughout this audit, we have drawn on evidence contained within these datasets. However, in many cases it was not possible to obtain meaningful data to support specific issues or findings. While these systems provide comprehensive coverage, they have limitations that restrict their usefulness.
Victorian Admitted Episodes Dataset and Victorian Integrated Non-Admitted Health minimum dataset
Palliative care inpatient services are required to collect patient data and record it on VAED. Community and consultancy services are required to report their patient data on the VINAH minimum dataset. Together, these datasets provide a good baseline of information that allows DHHS to understand the frequency and length of hospital stays and the proportion of people dying in home settings or in hospital.
VAED data has been collected over an extended period of time and covers all hospitals' patient services. Palliative care data is a small component of this overall dataset. VAED data is complex to analyse and has a strong medical focus. It captures patient information following discharge or death only, whereas the VINAH minimum dataset captures each separate contact with a patient, typically over a longer period so the information should provide a fuller picture of care services.
If completed properly, the VINAH minimum dataset is a tool that provides greater understanding of the patient context, such as living arrangements and the availability of a carer. Given that the majority of palliative care is managed by non-government community palliative care services, the VINAH minimum dataset should allow DHHS to complete useful trend analysis. However, there are some challenges with this data:
- Participation varies between community palliative care organisations—some smaller services struggle to complete all reporting or at worst, not report at all.
- The VINAH minimum dataset shows how many patients have limited or no support from a carer. However, many patients who are recorded as having no carer reside in an aged care or disability group home and benefit from regular supervision.
DHHS also requests data on service coordination to understand the extent to which different health services and community palliative care organisations connect—response rates from palliative care services are inconsistent or low. DHHS needs to be strategic and coordinated in managing its demands on time-poor palliative care staff and in the work it creates for itself in assessing the considerable volume of data.
Policy Implementation Audit Tool
DHHS uses PIAT to collect information on advance care plans, consultation with aged care and disability support homes, and palliative care research. However, DHHS has not enforced compliance with this reporting requirement and response rates have hovered around 70 per cent. Further, not all data received has been useable.
DHHS has used PIAT since 2011–12 to measure progress against the goals in its Strategic Directions that it cannot track through other existing reporting mechanisms. In its first year, 57 out of 72 health services responded to the PIAT survey. However, some did not have adequate data systems to fully answer all questions.
In the next year, 59 services responded, but in 2013–14 responses dropped to 50. Only 31 services have reported each year since the survey started in 2011–12.
Audited health services reported that it is still takes a long time to complete this survey and they do not understand how the information is used or what value it provides. As a result, they do not prioritise completing it.
DHHS has not adequately enforced compliance with this reporting requirement. Consequently it does not have a baseline that it can measure progress against over time. Given the significant reporting requirements placed on health services, it is important that they can understand the value in the data they are being asked to submit.
Palliative Care Outcomes Collaboration
PCOC is a voluntary program that uses standardised clinical tools to measure and benchmark patient outcomes in palliative care. It is coordinated by the University of Wollongong. Many smaller services do not participate due to the resources required. Therefore the services that participate are likely to be better resourced and able to meet benchmarks. This limits the extent to which results can be extrapolated to the whole sector. Nevertheless, they provide a useful snapshot of performance for this cohort. For the period January to June 2014, only 18 out of 56 services in Victoria participated in PCOC's voluntary reporting, comprising:
- 10 inpatient services
- six community palliative care services
- two services providing both inpatient and community palliative care services.
Victorian Palliative Care Satisfaction Survey
DHHS has been funding the VPCSS since 2010. The survey collects responses from palliative care patients, carers and bereaved carers and a report is released annually with statewide results. Responses to the survey are positive overall, and health services receive their individual results to assist them to target improvements. These individual reports include five questions that the health service received the lowest satisfaction scores for. One audited service stated that issues for improvement identified in the VPCSS had become KPIs. This is a transparent way to improve delivery of care.
2.5 Growing demand for services
A growing demand for and awareness of palliative care is increasing pressure on services—particularly community palliative care services. Lengthy stays in hospital are costly and more people, if consulted, prefer to die at home. This shift is already being felt in metropolitan areas and will continue to put stress on the sector. Patient and carer needs are not being met due in part to gaps in the range and availability of community palliative care services.
2.5.1 Dying in your place of choice
Research shows that most people would prefer to die at home. In 2012–13, 67 per cent of people who died in the care of a Victorian community palliative care service recorded their preferred place of death. The majority indicated they would prefer to die at home, however, only half were able to do so.
As the health care profession gets better at discussing death, and models of health care allow patients to have a greater role in decision-making, it is likely that there will be growing demand for palliative care to be managed in the home. Audited services reported that some clinicians still struggle to discuss dying. DHHS has an important role in guiding the sector to manage this transition.
In its Strategic Directions, DHHS committed to modelling demand for palliative care and developing a business case to support the sector to cope with a growth in service need. This has not yet occurred. However, it did recently hold a forum to discuss options for a new policy framework to succeed the Strategic Directions. DHHS' early feedback from palliative care representatives suggests that the sector is ready to aim higher and is interested in exploring how to measure the impact of its activities by focusing more on reporting patient outcomes. An example would be to report on how much time patients were able to spend in their place of choice prior to dying, rather than just recording the percentage of patients who actually died in a specific place. The modelling and new policy will be critical to help the sector better manage and coordinate existing resources, and to build the case for gradually expanding services and attracting more skilled professionals to palliative care.
2.5.2 Service capability
DHHS developed a palliative care service capability framework for health services. It required all health services to complete an annual self-assessment tool against key palliative care capabilities. However, following the first round of assessments in 2014, a DHHS review found that most palliative care services did not meet the expected standards. Some services had a perception of their service capabilities that exceeded their level of service provision. DHHS also decided that the self-assessment tool that services used was too stringent.
The service capability assessments are intended to provide DHHS with information on quality and service levels across the Victorian palliative care sector, and help health services understand how their practices align with DHHS' requirements. This would be enhanced by setting regional expectations for palliative care so that services can increasingly provide patients in rural areas with access to complete services. Some rural services struggle to access the range of professionals expected for comprehensive palliative care. Identifying the existing mix of services in each region would help DHHS identify gaps and overlaps.
DHHS has revised the tool and sought advice from the Palliative Care Clinical Network working group on its revisions. It intends to release a revised tool in late 2015.
DHHS acknowledges the challenges facing rural services in attracting specialist palliative care physicians. It has funded two programs to improve access to specialist palliative care skills and support in rural communities, the:
- Rural Palliative Care Medical Purchasing Fund
- Victorian Palliative Care Nurse Practitioner Collaborative.
Planning for any future palliative care policy should include performance expectations and clear guidance to specialist palliative care services with a service capability framework or a more structured suite of tools.
2.5.3 Discharging patients home—community-based care
The majority of palliative care occurs in community settings operated by non‑government providers. Currently, 35 per cent of Victorian palliative care funding goes to community-based palliative care—based on individual tender negotiations dating back to 1998. This is supplemented by modest growth funding introduced and distributed in 2005–06 and again in 2011–12, according to a population and needs‑based model. Audited health services expressed concern that their catchment demographic has changed in this time, but without any change in the base funding arrangement.
Given that some community palliative care services are struggling to accommodate people within appropriate time frames, it is timely for DHHS to review the funding model, which has remained largely unchanged for 10 years.
In 2012–13, there were 15 859 episodes of care for community-based palliative care patients—an episode of care for a community patient begins when the palliative care organisation takes responsibility for them and ends when they complete their treatment, refuse further treatment, or they die. In the same year, there were 7 305 palliative care separations in hospital—a separation is counted each time a patient is admitted and discharged from hospital during the year.
Waiting times
Some terminally ill patients have struggled to access community-based palliative care in a timely manner. The two audited health services that had an integrated community service advised that they do not have waiting lists for palliative care services. However, the other audited health services advised that accessing community-based palliative care is more difficult.
One service advised it had difficulty in getting community palliative care services to see patients with significant symptoms but longer life expectancy, such as emphysema. The other service stated that while it encourages its palliative care consultancy teams to get involved with terminally ill patients at an early stage, they sometimes have difficulty getting community palliative care services to accept patients at this early stage of their illness.
Community palliative care services identified that patients in inner-metropolitan areas have been made to wait extended periods for support in the home and that it is likely to occur again. For a period in 2014, one community service had a waiting list of up to six weeks and did not accept new patients due to a spike in demand and an unexpected staffing shortfall. In this instance DHHS was able to work with the health service to find alternative solutions. While it is good that DHHS was able to intervene in this manner, it is far from an ideal set of circumstances. This remains a major concern for metropolitan-inpatient facilities wishing to discharge patients to the community. It could potentially result in patients staying in hospital longer than they want, or receiving basic, non-palliative care in the home, or even re-presenting to hospital if symptoms escalate or become distressing.
In the first half of 2014, six Victorian community palliative care services submitted data to PCOC to benchmark the timeliness of their services. To meet the benchmark, 90 per cent of patients must be contacted on the day they were ready for care or the following day, which may be just a telephone call. As shown in Figure 2A, Victoria's score was 75.8 per cent for January to June 2014—an improvement on 62 per cent for the previous reporting period of July to December 2013. This compares with 84.3 per cent of for all Australian participating community palliative care services. Over 18 per cent of contacts in Victoria were made between two and seven days, compared to 11 per cent for all Australian services. So while there is overall improvement, Victorian services are still comparatively underperforming.
Figure 2A
Time taken for palliative care services to make first contact with patients January–June 2014
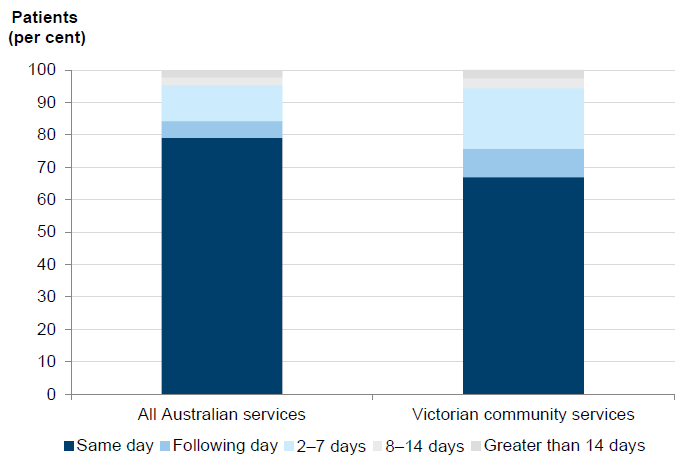
Source: Victorian Auditor-General's Office based on data provided by PCOC.
2.5.4 Gap for those with longer disease trajectories
Some palliative patients may be deemed to be in a stable condition but continue to need supervised care. In this case, the hospital may seek a bed in a residential aged care facility. However, community care and aged care is not suitable for many patients. Staff at two services spoke of the need for medium-term residential facilities for patients with longer disease trajectories, whose care requires palliative training and may be too physically demanding for a carer to manage unassisted.
A 2004 survey of carers of people with Alzheimer's disease found that 65 per cent provided care that is physically demanding and complicated due to the person's disorientation and confusion. Nearly one-in-four carers of people with Alzheimer's disease provided 40 hours or more of care a week. Further, 71 per cent sustain this for one year and 32 per cent for five years.
Staff from two services also identified difficulties associated with discharging people who are alone and have no family or support network to help with their care. There are limited facilities to support these people. In 2008, approximately 37 per cent of people with dementia received no formal care.
Community palliative care services said funding needs increase in the last days of the person's life as care needs increase. Often these people re-present to hospital as community palliative care services cannot provide the long-term or time-intensive support at the home.
2.5.5 Coordinating palliative care
Inpatient admissions
Audited health services have defined processes for admitting patients to their palliative care ward. Each used a different model for referrals and admissions depending in part on the capacity of their electronic patient information systems. The complexity of these systems and processes varied according to the size of the service. While the largest service had a lengthy, detailed admissions process, the smallest had a far simpler process in place more befitting a service of its size.
Each audited service used a different mix of health software for patient management and referrals and there is still a heavy reliance on faxes to transmit patient information. In particular, faxes and telephone calls were often relied on to refer patient information to community palliative care services.
All four audited health services had an arrangement in place with their emergency departments to directly admit known palliative patients to a palliative ward to avoid unnecessary queuing.
Allied health
Health services are expected to determine the staffing mix for their service based on local population needs and models of care. However, three of the four audited health services reported a lack of allied health support—social work, pastoral care, counselling, physiotherapy, occupational therapy, nutrition, speech therapy—for palliative patients.
DHHS advised that individual palliative care units need to advocate within their own organisations if they believe that allied health resourcing levels or mix are inadequate. However, as the system coordinator, it also has a significant role to play in monitoring and supporting service provision across the state.
Community referrals
DHHS has developed a tool to record patient information for health services to use when referring patients to community palliative care services. However, it is lengthy and audited health services advised that it took too long to complete. One health service had designed its admission process and electronic patient system to capture and automatically populate the data required by DHHS for referrals. There is, therefore, scope for other services to redesign and streamline their patient data systems to make referrals more efficient.
There is no evidence that patients in audited hospitals are not being referred to community palliative care services as a result of poor information systems. However, there is a risk that inadequate or out-dated patient tracking, transmission and storage of information could result in missed or delayed referrals.
As stated in Part 2.5.3, some patients who are discharged from hospital can experience difficulties accessing community palliative care services due to high demand.
Audited health services with integrated inpatient and community-based services were better able to support transition into community-based palliative care. Staff at these services reported that they do not have waiting lists. For one service, 2013 data shows that 78 per cent of community patients accessed care on the same day or the following day that they needed it. Data was not able to be verified for the other service.
Internal audits and reviews
One health service conducted routine audits on a selection of patient deaths—both those who had and had not received palliative care—to assess if there was an opportunity for earlier interaction with specialist palliative staff. This is a useful way for consult teams to understand how patient referrals happen across the health service and where there is more scope to build awareness of palliative care.
However, except for this one service, the audited health services did not routinely conduct internal audits of admission and referral processes.
2.5.6 Regional consortia
There was broad agreement among health services consulted that consortia are not fulfilling the planning role originally envisaged of them. Each consortium is run independently of DHHS, and feedback on their activities and effectiveness from health service staff varied between services. Those consortia that comprised largely dedicated palliative care staff and those that focused on education and improving clinical practice were generally more highly regarded.
Some positive consortium initiatives included training aged care staff and hiring nurses to train and promote palliative care to disability support and aged care staff. Not all consortia are progressing at the same pace and some have been slow to hire the staff required to complete training. DHHS monitors consortia performance through their annual reports, and provided guidance to assist consortia to report information that aligns with the Strategic Directions.
Consortia are not given a specific role in culturally-inclusive palliative care, but as demand for services increase, migrant populations will age and the sector needs to be prepared to respond to a variety of cultural and spiritual needs.
Cultural competency is required to ensure Aboriginal and Torres Strait Islander people and culturally and linguistically diverse communities feel comfortable accessing services. If the workforce cannot respond to a diverse population, the burden will fall to family and other carers. DHHS helped fund the Culturally Responsible Palliative Care Project in 2013–14, but there may also be a role for consortia to monitor cultural competency in their regional areas in future.
Recommendations
That the Department of Health & Human Services:
- reviews service provision as a priority to understand gaps in the system, better forecast demand and inform future service planning
- develops a robust policy evaluation method to monitor the implementation and outcomes of its new end-of-life care framework
- closely monitors health services' reporting on palliative care and follows up with health services when non-compliance is identified so that all required reporting is completed and can be analysed and communicated back to services.
That health services:
- conduct regular audits of patient files to understand if referrals and admissions to palliative care were managed in a timely and appropriate manner
- prioritise integrating patient data systems and improve information sharing options for communicating with community palliative care services.
3 Improving engagement with palliative care
At a glance
Background
Opening up discussion about care and treatment preferences early in preparation for death can help palliative care staff to best cater to patient needs and result in less anxiety and grief. Improving awareness of palliative care and advance care planning should improve access to services and help more people to make informed choices about their death. Coordinating these services is a significant challenge.
Conclusion
The Department of Health & Human Services (DHHS) has taken a slow but methodical approach to implementing actions outlined in its Strengthening palliative care: Policy and strategic directions 2011–2015 (Strategic Directions) to improve awareness of palliative care in communities that do not typically access these services. It is not yet clear what impact these actions have had on patient awareness. Similarly, advance care planning has been an accepted model of practice for many years, but it is only in the past 12 months that some health services have begun to adopt these practices.
Findings
- There has been little progress in improving community awareness since 2011, although a number of promising initiatives commenced in 2013.
- Low survey response rates prevent DHHS from understanding the use of advance care planning.
- Advance care plans are used with around half of all patients supported by community palliative care services. This has not changed over time.
Recommendations
That health services:
- prioritise the implementation of advance care planning and comply with DHHS' data collection and reporting requirements.
That DHHS and health services work to:
- understand barriers to accessing care, understand and respond to unmet demand, and engage communities who don't traditionally access palliative care
- provide patients and carers with more support to understand what services are available and how to access them when they need them.
3.1 Introduction
Awareness of palliative care starts in the community. Aged care services, general practitioners, disability support homes, religious and cultural organisations, universities and training institutions, and the government all have a role to play in communicating information about dying. The more organisations involved, the greater the chance that palliative care and real choices about where and how to die will be discussed. The challenge is to reach more people and parts of the community not currently utilising services.
In March 2014, the Department of Health & Human Services (DHHS) released Advance care planning; have the conversation: A strategy for Victorian health services 2014–2018 to support health services to develop, review and activate advance care plans (ACP). Advance care planning provides an effective tool for prompting discussions and preparations for the end of life. Ideally these discussions begin before an emergency brings someone to hospital.
This Part assesses initiatives to improve community awareness about palliative care and the implementation of advance care planning in audited health services.
3.2 Conclusion
Work has begun—albeit belatedly—to improve awareness of palliative care in communities that do not typically access these services, and within hospital settings. It is not yet clear what impact these actions have had on patient awareness. Further work is required to understand and address the barriers to particular sectors of the community engaging with palliative care.
Engaging patients and their carers needs to begin earlier so that they can make informed decisions about how to manage care independently and access support when they require it.
Advance care planning has been an accepted model of practice for many years. Despite this, use of advance care planning is low and shows no signs of growth. It is disappointing that greater progress has not been made as advance care planning is a central pillar of effective palliative care. It allows palliative care teams to understand what is important for a patient at the end of their life, and brings comfort to the patient, their family and carers that their final wishes are known and will be considered. DHHS should continue to promote advance care planning across all health settings and improve its reporting to better understand the level of uptake across the health system.
3.3 Raising community awareness
Progress to improve community awareness about palliative care has been slow. DHHS has started to introduce community awareness programs and encourages health services to develop consultancy services to guide and support hospital and community-based staff. However, further work is required to:
- engage communities that do not traditionally access palliative care
- understand barriers to accessing care
- understand and meet unmet demand.
DHHS' Strengthening palliative care: Policy and strategic directions 2011–2015 (Strategic Directions) recognised the need to raise community awareness about palliative care to encourage people to talk about dying and better understand the available options for support. It committed DHHS to raising awareness of palliative care among Aboriginal and Torres Strait Islander people and people from culturally diverse communities.
DHHS has made some progress towards this objective. It has introduced new programs for culturally and linguistically diverse communities and funded a number of projects to support the provision of culturally responsive palliative care for Aboriginal and Torres Strait Islander people. However, as DHHS was slow to implement this action, it is still too early to examine the impact of these actions.
Figure 3A
Advocacy in culturally and linguistically diverse communities
People from culturally and linguistically diverse communities are slightly more likely to die in hospital than Australian-born patients. Patients with a recognised need for an interpreter more commonly died in hospital (71.5 per cent of the time) compared to patients who spoke English (66.4 per cent of the time). In 2013–14, DHHS funded a project to raise awareness of palliative care among Chinese, Italian, Maltese, Turkish and Vietnamese communities and improve their access to palliative care services. This project included:
At the end of the first year, DHHS contracted a researcher to complete a project evaluation. It found that:
|
Source: Victorian Auditor-General's Office.
3.3.1 Engaging health care staff and carers
Staff from audited health services agreed that health professionals need to engage people in palliative care earlier in the patient's journey. The Strategic Directions intended to build 'awareness, capacity and resilience' in people with a terminal illness and their carers. To build the capacity and resilience of carers it is important to strengthen the skill base of staff across the healthcare system so that they are better able to:
- advise carers about the task ahead
- provide information on how to manage care independently and when and where extra support may be necessary.
DHHS' 2004–09 palliative care policy introduced the requirement for health services to develop palliative care consultancy services. These services consist of teams of doctors and nurses who provide advice, support, education and training to treating teams in hospitals, community palliative care services and general practitioners. These are now well established within hospitals and some also consult to aged care and disability services and support palliative care provision in rural areas. Palliative care consult teams have increased from four teams across the state in 2004 to 18 in 2015.
3.4 Advance care planning
DHHS has had difficulty tracking the use of advance care planning in health services—particularly inpatient services. In community palliative care services, use of ACPs has remained at around 50 per cent since 2012. Some Victorian health services have been using different models of ACPs for over 10 years.
Advance care planning is a process by which health professionals discuss and document their patient's end-of-life care preferences. Ideally a patient will complete an ACP prior to being admitted to palliative care, or following admission to an inpatient or a community palliative care service. Documented ACPs should guide future clinical decision‑making. This is particularly important where a patient later loses their decision-making capacity. Research, completed by Monash University, showed that completing an ACP can improve quality of care at the end of life and increase the likelihood of a person's wishes being known and respected.
DHHS' Advance care planning; have the conversation: A strategy for Victorian health services 2014–2018 promotes the use of advance care planning in health services and provides clear guidance for generalist health care staff on how it should work. However, some jurisdictions such as South Australia and Northern Territory now have legislation for advance care planning, including specific forms for health services and patients to create. New South Wales introduced a policy similar to Victoria's in 2013, Advance Planning for Quality Care at End of Life: Action Plan 2013–18.
Most of the audited health services had made significant progress towards implementing advance care planning in the past 12 months. However, progress varied by service as shown in Figure 3B.
Figure 3B
Progress of advance care planning in health services
|
Source: Victorian Auditor-General's Office.
Staff from audited inpatient services advised that while they are trained to start palliative care conversations, they feel that it is often not appropriate to begin end‑of‑life discussions at the late stage they see patients. Research, completed in 2013 by Monash University together with the Alfred Hospital, found that for 64 per cent of patient charts reviewed in metropolitan health services the first record of end-of-life discussions occurred in the last 24 hours of life.
Audited inpatient staff suggested that general practitioners—who are most likely to have a long-term relationship with a patient—should initiate these conversations earlier.
Figure 3C outlines a typical scenario that highlights the importance of having appropriate supports in place to facilitate palliative care conversations.

Figure 3C
Difficult discussions
Mr J had a fall at home triggering a heart attack. As his daughter sat waiting with her mother at the hospital they talked about Mr J's views on dying. Her mother said that despite his age, his relative good health meant that he had not thought too much about death—maybe he had assumed he would deal with it later or when a serious health issue came up. A nurse asked them if Mr J had an ACP. They advised they were not sure what this was. The nurse explained that a completed plan would help health care staff and family to decide what care is best for a patient—for example, if Mr J preferred to be resuscitated or not. The nurse left some information for them to look at later. When Mr J woke up, Mrs J and his daughter visited him, but they were too emotional to bring up the ACP. Mrs J left the information in a prominent spot in the house in the hope that Mr J would discover it and decide for himself without anyone needing to bring it up. Mrs J discussed her apprehension with the community palliative care nurse when she visited the house the following week. After making sure Mr J was comfortable, the nurse asked him about what care he might want at the end of his life—treatment to prolong life or to keep him as comfortable as possible. They looked at the ACP forms together and Mr J asked some questions—he wanted to know if he could change his mind once he had signed the documents—the nurse assured him that he could at any time. This made him feel more in control. A few days later he talked through his decisions with his wife. Mrs J hoped that they would not need to use the forms and was very relieved that she didn't need to make these decisions by herself and without having properly discussed it with her husband. |
Source: Victorian Auditor-General's Office.
3.4.1 Uptake of advance care plans
To track the progress of advance care planning implementation, DHHS requires community-based inpatient services—the palliative wards and the consulting teams based in hospitals—and day hospices—non-medical respite facilities—to use its Policy Implementation Audit Tool. This tool collects information that is not captured by current reporting requirements through a survey.
However, DHHS did not sufficiently consult with health services about the data required and its purpose, and response rates were too low to be usable. In 2011–12, 21 out of 57 health services who responded to the survey were unable to respond to the questions on documented ACPs, or could only provide an estimate. This means there is no true baseline from which to measure performance. DHHS advised that this data is unreliable and should not be reported.
DHHS also requires community palliative care services to provide information on advance care planning in its Victorian Integrated Non-Admitted Health (VINAH) minimum dataset. This data is more reliable as more services have been responding each year.
Figure 3D shows that the percentage of community palliative care service episodes with ACPs has remained steady at around 50 per cent since 2012. However, DHHS needs to improve its data collection to better understand if and how advance care planning is utilised in inpatient settings so that it can work with health services to better target advocacy.
Figure 3D
Community palliative care service episodes with an ACP
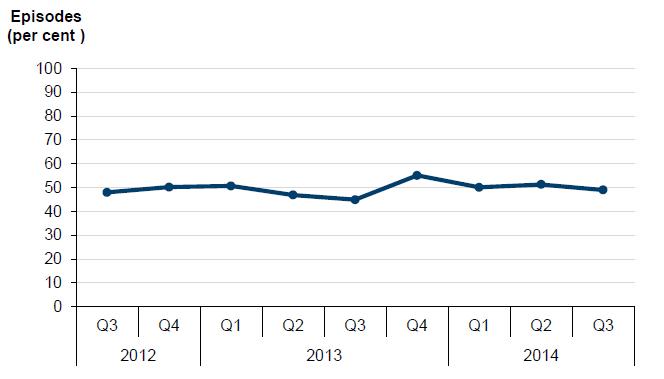
Note: An
increasing number of community palliative care services are submitting VINAH
data to DHHS each year—this graph tracks only community palliative care
services that submitted VINAH data in 2012–13.
Source: Victorian
Auditor-General's Office analysis of DHHS data.
3.5 Palliative care for people with a disability
Awareness of palliative needs in group homes—such as for people with a disability or in an aged care facility—is promoted by a nurse in each region, funded by DHHS promote existing palliative care guidance and provide links to community palliative care services.
In 2010, DHHS developed the Disability Residential Services Palliative Care guide: End-of-life care for residents of disability residential services that explains the key areas for support, and identifies useful documents, training and resources. One consortium advised that the guide was useful but not well known. Community visitors appointed to visit and report on support in group homes were consulted for the audit—they were not aware of the guide.
Community visitors outlined a number of positive examples of disability staff accessing palliative care services for residents. One example is seen in Figure 3E.
Figure 3E
Supporting people with disabilities
In one example, when a resident recently diagnosed with cancer expressed a wish to die at home, the manager contacted the regional palliative care consortium for advice. The consortium's disability link nurse organised a forum at the shared supported accommodation facility for the staff and family. At the forum, the disability link nurse provided advice about the treatment prognosis and palliative care. The disability link nurse then assisted the staff to contact a community palliative care service and organised regular visits. The house manager established a support group of nurses from the nearest hospital, the consortium disability link nurse, house staff and family. The community palliative care service provided direct care for the resident and the disability link nurse was available to support the staff, residents and family. |
Source: Victorian Auditor-General's Office based on community visitors' feedback.
Recommendations
That health services:
- prioritise the implementation of advance care planning and comply with the Department of Health & Human Services' data collection and reporting requirements.
That the Department of Health & Human Services and health services work together to:
- understand barriers to accessing care, understand and respond to unmet demand, and engage communities who do not traditionally access palliative care
- provide patients and carers with more support to understand what services are available and how to access them when they need them.
4 Support for carers
At a glance
Background
Carers and families play an essential and irreplaceable role in the palliative care system. Without them, patients would miss out on high levels of support, care and comfort. Carers and families can also bear significant physical and emotional strain.
Conclusion
Support for carers remains inadequate. Improving access to services such as respite and psychosocial support for carers of people with a terminal illness remains a major priority. The Department of Health & Human Services (DHHS) also needs to review patient and carer reporting and after-hours service provision.
Findings
- Access to overnight respite is one of the greatest carer needs, but is not widely available.
- Carer support needs to be well timed and flexible to best avoid carer stress.
- After-hours support is available to carers, however, a review of access and quality of support is needed.
- DHHS has developed bereavement support standards for use in specialist palliative care services, but many services do not use these.
Recommendations
That the Department of Health & Human Services:
- conducts a systematic review of respite and carer support provision
- develops clear expectations for health services to appropriately support carers
- reviews system-wide palliative care performance measures
- reviews and improves the after-hours model for community palliative care services across Victoria.
4.1 Introduction
Once a diagnosis of a terminal illness is made, hospital and community palliative care services can act to identify the needs and preferences of both the patient and their carers. As well as providing services to support the patient, health services and community palliative care services also monitor the wellbeing of carers and families. They provide or connect carers to services to support them through their loved one's end of life and death. These services include psychosocial care and advice in addition to respite and bereavement services.
This Part assesses carers' access to bereavement and respite services.
4.2 Conclusion
Despite the Department of Health & Human Services' (DHHS) attempts to address carer support through its palliative care policies, support for carers remains inadequate. Improving access to services such as respite and psychosocial support for carers of people with a terminal illness remains a major priority for the palliative care sector.
Some progress has been made—DHHS provides discretionary funding to help reduce the financial burden of care and there has been improvement in access to after-hours support, mainly through telephone advice. While these steps will help, they are not responsive or comprehensive enough to provide the level of support that is needed.
In addition to increasing the breadth and availability of support for carers, DHHS also needs to improve the quality of reporting on these matters. It could better monitor after‑hours service provision, bereavement support activity and carer satisfaction with a range of palliative care services.

4.3 Support for carers
While a range of support options are available to carers—including respite, after-hours support, and bereavement support—these are not always sufficient or responsive to their needs. In particular, there has been little improvement in respite since 2011.
Making sure that carers get the support they need begins with family and friends. Drawing on existing resources means the carer can talk about their needs with people they know and feel comfortable with and request help as necessary. However, even with support from family and friends, carers are likely to need to access specialist advice, have proper sleep and cleaning services.
VAGO's 2012 report Carer Support Programs reported that carers are more at risk of mental health problems, such as stress or depression, than other people of the same age and are more likely to suffer declines in their physical health due to caring.
DHHS' Strengthening palliative care: Policy and strategic directions 2011–2015 (Strategic Directions) had a strong focus on supporting carers. It identified the following four areas as key areas for improvement:
- access to after-hours support
- training for carers
- bereavement support
- appropriate respite—including access to in-home and out-of-home respite, overnight nursing, day hospices and volunteer visiting programs.
Feedback from audited health services and other stakeholders indicated that access to overnight respite is one of the greatest carer needs.
4.3.1 Carer satisfaction
DHHS uses the Victorian Palliative Care Satisfaction Survey (VPCSS) to assess carer satisfaction. However, response rates are variable and more work needs to done to understand the reasons for any carer dissatisfaction.
Since 2011, responses from carers, patients and bereaved carers to the question 'How satisfied were you with the overall standard of care provided by the palliative care service?' have remained stable. In 2014, the mean satisfaction score for all groups was 4.62 out of 5 indicating high levels of satisfaction with the overall standard of care.
The survey is optional and may not be provided to patients or carers at a time when they feel up to responding.
4.3.2 After-hours support
It has been a requirement for community palliative care services to provide after-hours support—outside of 7am and 4.30pm Monday to Friday and public holidays—since 1997. However, DHHS does not monitor compliance with this requirement and could not provide any assurance that the services currently being provided are sufficient or appropriate to meet the needs of carers.
Access to after-hours support is a reassuring option for carers who need advice on managing medication, pain and distress. It may also involve a visit from a nurse if the service assesses that it is required and it is safe for staff to do so. It is an important part of meeting carer needs but is not a substitute for respite.
Acknowledging that provision of after-hours support varied across the state, DHHS ran two pilot projects in 2009 to test different models. It then commissioned a review of the pilot projects in 2011.The evaluation noted that rural services were reluctant to switch to a more centralised model of after-hours support because they felt strongly that their clients should speak to a service or staff member they were familiar with.
The review did not propose a single after-hours model but recommended a range of different regional approaches. DHHS released its new framework for after-hours support in February 2012 following this review. The framework outlines the key elements of effective after-hours care and has a 'how-to' guide of protocols for community palliative care services and triage staff to use. While it is a useful resource it needs to be supported with ongoing training for responsible staff. Training and support was a part of the pilot phase but has not been provided more broadly since this was completed.
Currently, there are variations on three models of after-hours support across the state:
- a regional after-hours nursing telephone triage service provider supporting several community palliative care services
- a local hospital after-hours manager providing telephone triage to the local community palliative care service
- an individual palliative care service or local district nursing service providing after‑hours telephone triage support to the local community.
One metropolitan health service has been providing an after-hours telephone triage service for over seven years, supporting two metropolitan community palliative care services and two regional community palliative care services. This service covers around 25 per cent of Victoria.
Further to this, the Commonwealth Government recently launched Decision Assist—a national service that provides around the clock telephone support for general practitioners, aged care staff and other health professionals providing palliative care in residential aged care and home care. Decision Assist aims to improve access to appropriate and effective palliative care for ageing Australians by upskilling the health care workforce.
Given that several years have elapsed since DHHS completed its review and released its new framework, it would be timely to review the after-hours service model for community services across Victoria in 2016 to:
- determine how the different service models compare
- understand the extent to which technical concerns raised during the pilots have been resolved
- examine how services could best be aligned to ensure coverage across the state is equitable and consistent.
4.3.3 Respite
All stakeholders consulted during the audit agreed that improving access to respite for carers of people with a terminal illness remains a major priority for the palliative care sector.
Respite enables carers to have a break from caring for their loved one and catch up on sleep and other regular activities that might become neglected. Health service staff advised of instances where patients were admitted to inpatient services near death because their carers were unable to cope. Respite options in Victoria include:
- four hospices across the state, funded by DHHS, that cater for patient day-visits including one that caters for patients with motor neurone diseases
- in-home support from volunteers or community services such as the Royal District Nursing Service.
While these supports can provide reassurance and assistance to the carer, palliative care staff in audited health services advised of the 'catch 22' situation where carers, despite being overwhelmed, refrain from taking time away from the patient due to feelings of guilt at being apart so close to their death. In these circumstances, being away from the patient may be of limited assistance. Timing of interventions is therefore critical.
Audited health services had adopted differing approaches to prioritising respite services. The three audited metropolitan health services operated waiting lists, while the regional service scheduled staff to provide care in the home depending on availability:
- Service 1 prioritises admitting patients with complex symptoms over those on their waiting list for respite. VPCSS survey data showed a number of complaints about not being able to remain in the palliative care service. Carers and bereaved carers were pleased with availability of respite.
- Service 2 also has a waiting list for admission to palliative care. However, it is not clear how respite is prioritised at that service. Staff at the service identified that many carers in their community cannot afford to take leave from work, placing increased burden on hospital-based services.
- Service 3 also had waiting list for admission to inpatient palliative care. VPCSS survey data showed that patients, carers and bereaved carers had complained of waiting for access to palliative care services, including respite. The service acknowledged that significant population growth in its area had impacted on demand.
- Service 4 can schedule community staff to make regular respite visits depending on staff availability and the severity of the carers' needs. VPCSS survey data had only one complaint related to accessing community-based palliative care.
Inevitably, despite respite being recognised as a significant need, palliative care services prioritise care for patients needing medical attention over the needs of carers.
Further research on respite
DHHS completed further research on respite after releasing its Strategic Directions. The findings of this research were inconclusive, but did suggest that the initiatives outlined in the Strategic Directions were not sufficient to meet the gap in carer respite needs.
In June 2014, DHHS completed a literature review to look for evidence to back the use of respite to support carers of patients with palliative care needs. It found that there is limited rigorous evidence that respite care improves patient or caregiver outcomes. It found that:
- respite care should be available to support family carers of people with moderate or severe dementia
- respite care should be available to support family carers of frail or unwell older adults
- there is insufficient evidence to support whether respite should be made available to support carers of adults with chronic conditions.
DHHS is currently in the early stages of developing the next draft of its new palliative care strategy and has started to engage with the sector to devise more flexible support options for carers during particularly stressful periods—such as when a patient's symptoms or pain become unstable and when they enter the terminal phase at their end of life. It is therefore unlikely that any carer support programs will be implemented before the Strategic Directions finish in December 2015. DHHS needs to continue to prioritise respite and to better understand and cater for a range of, often considerable, carer needs.
4.3.4 Financial strain on patients and carers
Recognising that carers often bear considerable financial strain, DHHS provides health services with a limited amount of funding to provide medical equipment in the home on an as-needs basis. However, health services continue to be concerned about carers who cannot afford to be away from work on an indefinite basis.
Figure 4A shows rates of satisfaction with financial and legal assistance in DHHS' VPCSS. Responses to most questions are typically very positive, however, responses to financial and legal assistance questions are less positive than other areas surveyed.
Figure 4A
Carer satisfaction with financial and legal support
Question |
Carer |
Bereaved carer |
|---|---|---|
Extent to which you are aware of financial assistance available from the government |
3.67 |
3.53 |
Satisfaction with support for legal issues |
4.03 |
3.94 |
Satisfaction with support to minimise financial burden |
3.66 |
3.40 |
Extent to which you are coping with the financial burden of caring |
3.8 |
4.07 |
Note: Responses
provided on a 5-point Likert scale, where 1 = very dissatisfied and 5 = very
satisfied.
Source: Victorian
Auditor-General's Office from the Victorian Palliative Care Satisfaction
Survey Statewide Report 2013.
In the same year, the VPCSS measured patient, carer and bereaved carer satisfaction with the overall standard of care was 4.62, and the average satisfaction of all questions in the survey was 4.27. These results point to the need for health services to improve the way they communicate with carers and bereaved carers about financial assistance and other support to minimise financial burden.
A social worker at one audited health service estimated that about 20 per cent of patients experience financial stress. Patients or carers are referred to a financial advisor. However, aside from the VPCSS, there is very little data collected on these issues.
4.4 Bereavement and stress
DHHS' bereavement support standards provide guidance for services to assist carers most at risk of complex grief. However, reporting does not comprehensively capture the extent of bereavement activity that occurs and staff from audited health services expressed concern about the bereavement services offered.
It is not always clear when bereavement support should be provided as part of inpatient or community palliative care services, or through referral to a specialist service. DHHS advises that inpatient services may not be the most appropriate choice for bereavement services and that referral to a specialist is often more appropriate.

4.4.1 Bereavement in audited health services
Three of the four audited health services expressed concerns about the quality and amount of bereavement support available to carers of palliative care patients. Three services stated that their bereavement service is under-resourced and two were concerned that the range of different professionals providing bereavement services across the state could lead to fragmented and incomplete service:
- Service 1 uses a pastoral carer for bereavement and holds a memorial service for deceased patients twice a year. A bereavement package with information on counselling is sent out following a patient death and staff follow up with carers after three and six months. There is a standard process for referral to bereavement support.
- Service 2 provides the most comprehensive service, offering patients and carers access to a dedicated bereavement counsellor. A grief counselling service is available for anyone in the region who has experienced a loss. There is a comprehensive risk-screening tool and the service requests feedback on its services to improve performance.
- Service 3 also uses an extensive risk-screening tool, a pastoral carer and a referral process for expert support. This service advised it is under-resourced for psychosocial care and is unable to meet all the system needs.
- Service 4 has a social worker working with patients and carers. The service has just begun piloting a new risk-screening tool. Previously nurses had informal discussions together and made calls when time permitted.
4.4.2 Bereavement support standards
DHHS developed bereavement support standards in 2012 for use in Victorian government-funded, specialist palliative care services. However, many inpatient services do not use these and there is scope for DHHS to further promote them to health services.
Health services report on whether they use the bereavement support standards via the Policy Implementation Audit Tool survey. In 2013–14, 83 per cent of community-based palliative care services reported using the bereavement support standards compared with 58 per cent of inpatient services and 67 per cent of hospital consult services. None of the audited health services used the bereavement support standards.
The key principles of the bereavement standards are that bereavement support is delivered:
- in a targeted way, with those who would benefit most from specialist interventions being identified through structured screening and assessment
- with a focus on identifying the bereaved person's own resources and capacity to enhance their resilience
- over a period from pre-death to several months post-death and beyond where required
- with a focus on the palliative care client's primary carer and extending to other carers/family members where resources allow.
4.4.3 Bereavement reporting
A lack of bereavement reporting may undermine the importance of this service to carers.
Patients in inpatient and community palliative care services have an identifier linked to their care which can be used to determine funding. These identifiers are not created for carers who may need bereavement services. Interviewed staff from community palliative care services had experienced difficulty recording more than one bereavement contact on the Victorian Integrated Non-Admitted Health minimum dataset. This limits the tracking of bereavement activity in inpatient and community‑based settings. Two audited service advised that the lack of performance indicators for bereavement reduces the importance of the activity within the service.
Limited bereavement activity is recorded in community palliative care services but they may also provide bereavement support that is not able to be reported on. DHHS should assist health services to ensure all carers are screened and referrals for complex grief are made to appropriate services.
Recommendations
That the Department of Health & Human Services:
- conducts a systematic review of respite and carer support provision
- develops clear expectations for health services to appropriately support carers including providing practical information on patient care and advice or referral as appropriate for emotional and bereavement needs
- reviews system-wide palliative care performance measures to improve how hospitals and palliative care services document and deliver patient- and carer‑focused services
- reviews and improves the after-hours model for community palliative care services across Victoria.
Appendix A. Audit Act 1994 section 16—submissions and comments
Introduction
In accordance with section 16(3) of the Audit Act 1994 we provided a copy of this report to the Department of Health & Human Services, St Vincent's Hospital Melbourne (including Caritas Christi Hospice), Northern Health, Mercy Health (Werribee Campus) and Central Gippsland Health Service with a request for their submissions or comments.
The submissions and comments provided are not subject to audit nor the evidentiary standards required to reach an audit conclusion. Responsibility for the accuracy, fairness and balance of those comments rests solely with the agency head.
Responses were received as follows:
- Department of Health & Human Services
- St Vincent's Health Australia, the governing body of St Vincent's Hospital Melbourne
- Northern Health
RESPONSE provided by the Secretary, Department of Health & Human Services
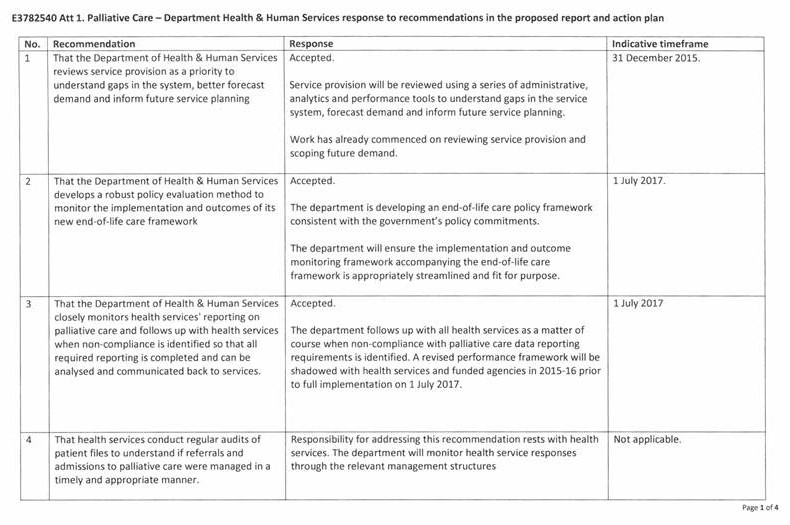
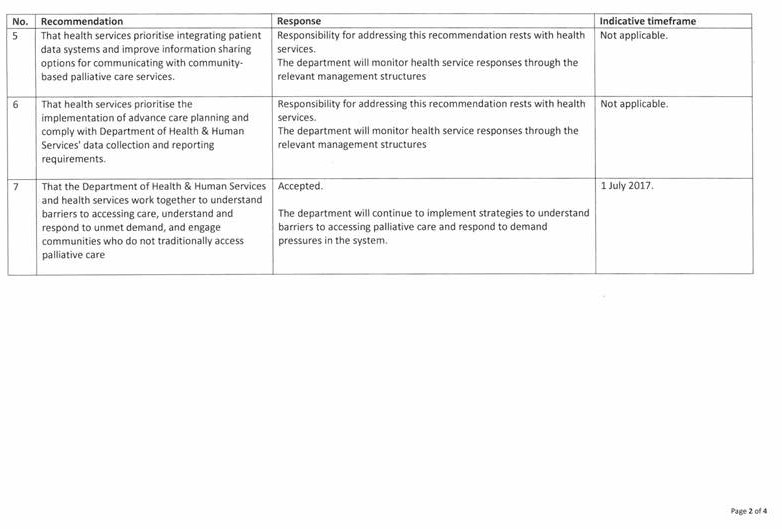
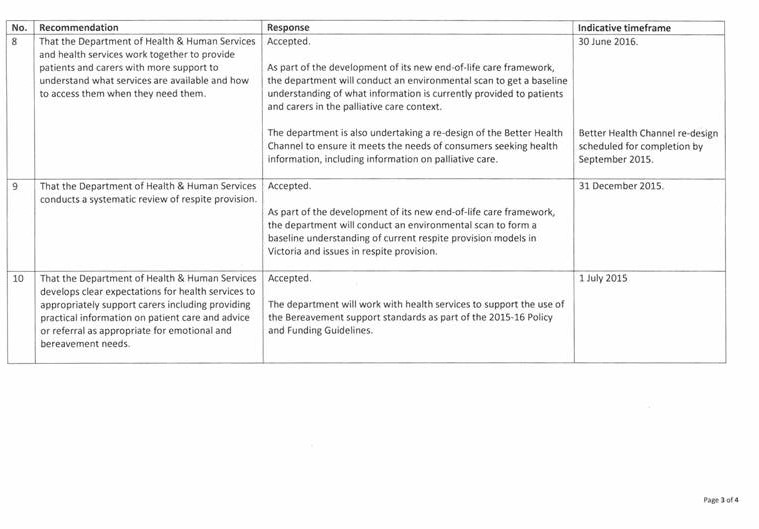
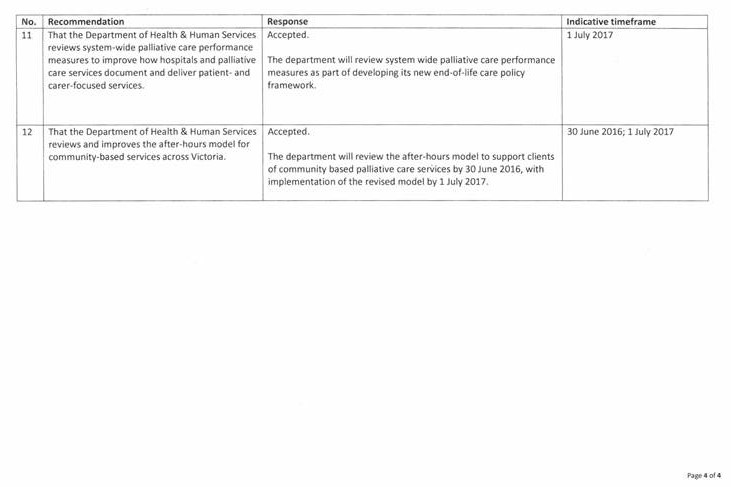
RESPONSE provided by the Chairman, St Vincent's Health Australia
RESPONSE provided by the Acting Chief Executive Officer, Northern Health